Earlier, plain radiographs and other radiological investigations were the main source of radiation. But with the invention of CT scan and its increased use worldwide make this imaging technique to become the main source of radiation load over paediatric patients [1]. When compared with conventional radiography, CT comes with 100-500 times higher radiation exposure and thus can be related with higher risk of carcinoma [2]. According to a recent study, the risks of leukemia and brain tumors in children become three times higher with a cumulative dose of 50 mSv and a dose of 60 mSv respectively [3].
Among the children coming to the hospital with mild head injury (Glasgow Coma Scale, GCS scores of 13-15), clinical attention is needed in less than 5% and less than 1% requires neurosurgical intervention [4]. Decision analyses (making effective decision by providing logical, systematic analysis with imagination) suggest that the risks of radiation outweigh the risks of Traumatic Brain Injury (TBI) in most of the children, who are at low risk of TBI, and thus CT is not warranted. Despite this, over one third of children with minor head injury undergo CT [5].
In comparing all imaging modalities in terms of radiation emission, CT comes highest with 67% though it represents only 10% to 15% of all imaging [6,7]. Moreover, paediatric patients are more vulnerable to CT as they are 10 times higher radiosensitive than adults [8].
A large number of children per year are being exposed to the hazardous effects of radiation due to use of CT. Moreover, this radiological investigation also causes a large addition to health care expenses [9]. Currently, there are no widely accepted, evidence-based guidelines on the use of CT for children who are at low risk of TBI [10].
The present study was carried out to draw attention on the unnecessary use of CT scan of brain in paediatrics patients and the need of valid guidelines for the use of CT in children with head injury.
Materials and Methods
The present study was a retrospective study based on the CT brain reports of paediatric patients (less than 18 years age) of last three years from September 2014 to September 2017, referred to the Department of Radiology, Gauhati Medical College and Hospital, Guwahati, Assam, India. The study was approved by the Institutional Ethical Committee.
CT scanner used was Siemens (Equipment ID: 1006582472) Somatom Spirit dual slice (spiral) and manufactured in China on May 2007. In CT protocol, patients were in supine position with arms by the side of the body. Plane of imaging was parallel to cantho-meatal line and 5 mm contiguous slice without inter-slice gap. Reconstruction was 5 mm (for bone window).
Inclusion Criteria: Paediatric cases referred to the Department of Radiology for CT scan of brain were included in the study.
Exclusion Criteria: CT brain of paediatric cases with prior imaging findings of tumours or other pathological causes were excluded from the study.
Subjects were divided into three groups A, B and C based on CT report findings. Group A: paediatric head injury patients with normal CT scan reports, group B: children of head injury patients with CT scan reports of soft tissue swelling or scalp laceration and group C: paediatric head injury patients with positive CT scan findings of brain injury.
Statistical Analysis
Various particulars of the patients like age, sex along with normal or any findings of CT reports were recorded, tabulated and statistically analysed with Statistical Package of Social Science (SPSS Version 19.0; Chicago Inc., USA).
Results
Total of 1056 paediatric head injury patients CT scan reports were collected and thoroughly reviewed. Among 1056 cases, 690 were male and 366 were female paediatric patients. Thus, male patients outnumbered female paediatric patients with male to female ratio of 1:89.
After putting all the particulars of 1056 paediatric patients from CT reports in Microsoft office excel sheet with important findings of the reports, it was found that 526 paediatric patients (group A) had normal CT head findings [Table/Fig-1] with percentage of 49.81% (out of 1056). This figure which is almost 50% indicates that half of the head injury paediatric patients could be managed without CT scan exposure. Out of these 526 cases, 346 were male and 180 were female paediatric patients.
Normal CT of a 10-year-old female patient, a) (bone window) thick black, purple, green and yellow arrows show petrous temporal bone, mastoid temporal bone, squamous temporal bone and frontal bone respectively; b) (brain window), thin blue, red, black arrows show lateral ventricle, cerebrum and skull bone respectively; c and d) CT images of a 14-year-old male patient with scalp laceration and haematoma.
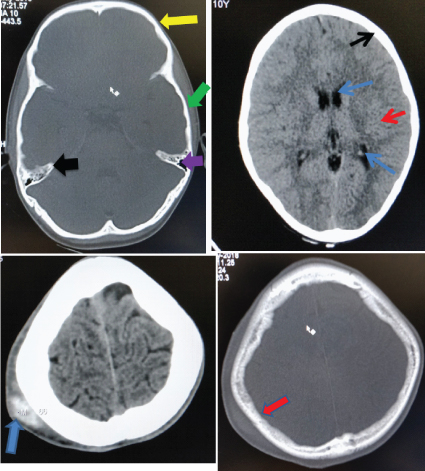
Moreover, 119 paediatric (Group B) cases had soft tissue swellings or soft tissue lacerations without major CT scan head findings [Table/Fig-1a-d] with percentage of 11.27% (out of 1056). Out of these 119 cases, 75 were male and 44 were female paediatric patients. Thus, these 119 cases could also be managed without CT scan investigation. Also, if these minor head injury cases added with normal cases (Group A+ Group B) then the figure came out to be 645 with percentage of 61.08% (out of 1056). Hence, about 61% head injury paediatric patients could be diagnosed and treated with clinical evaluation without putting these growing children into radiation exposure.
In [Table/Fig-1c], thick blue arrow shows scalp swelling over the right parietal region with hyperdensity within suggestive of scalp haematoma. In [Table/Fig-1d], thick red arrow shows the scalp swelling with intact underlying bone and absence of any fracture.
Group C [Table/Fig-2,3 and 4] comprised of 411 paediatric head injury patients with 38.92% (out of 1056).
Number of paediatric head injury patients with various CT scan head findings.
| CT Scan Head Findings in Paediatric Head Injury Patients | Number of Paediatric Head Injury Patients |
|---|
| Hydrocephalus | Communicating | 25 |
| Non-communicating | 13 |
| Sub-arachnoid haemorrhage (SAH) | 13 |
| Extra Dural Haemorrhage (EDH) | 19 |
| Sub-Dural Haemorrhage (SDH) | 15 |
| Calvarial Fracture | 41 |
| Frontal Bone Fracture | 8 |
| Parietal Bone Fracture | 9 |
| Temporal Bone Fracture | 3 |
| Occipital Bone Fracture | 7 |
| Orbital Bone Fracture | 7 |
| Nasal Bone Fracture | 6 |
| Maxillary Fracture | 9 |
| Mastoid Fracture | 2 |
| Cerebral Edema | 16 |
| Hypoxic Ischemic Injury (HII) | 49 |
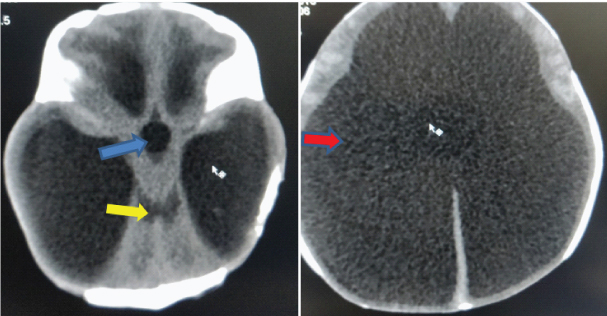
CT scan of a 28-day-old male with obstructive hydrocephalus (non-communicating) dilated lateral ventricles and third ventricle with normal 4th ventricle suggestive of aqueductal stenosis; a) blue arrow shows dilated third ventricle, yellow arrows show normal 4th ventricle; b) red arrow shows dilated lateral ventricles.
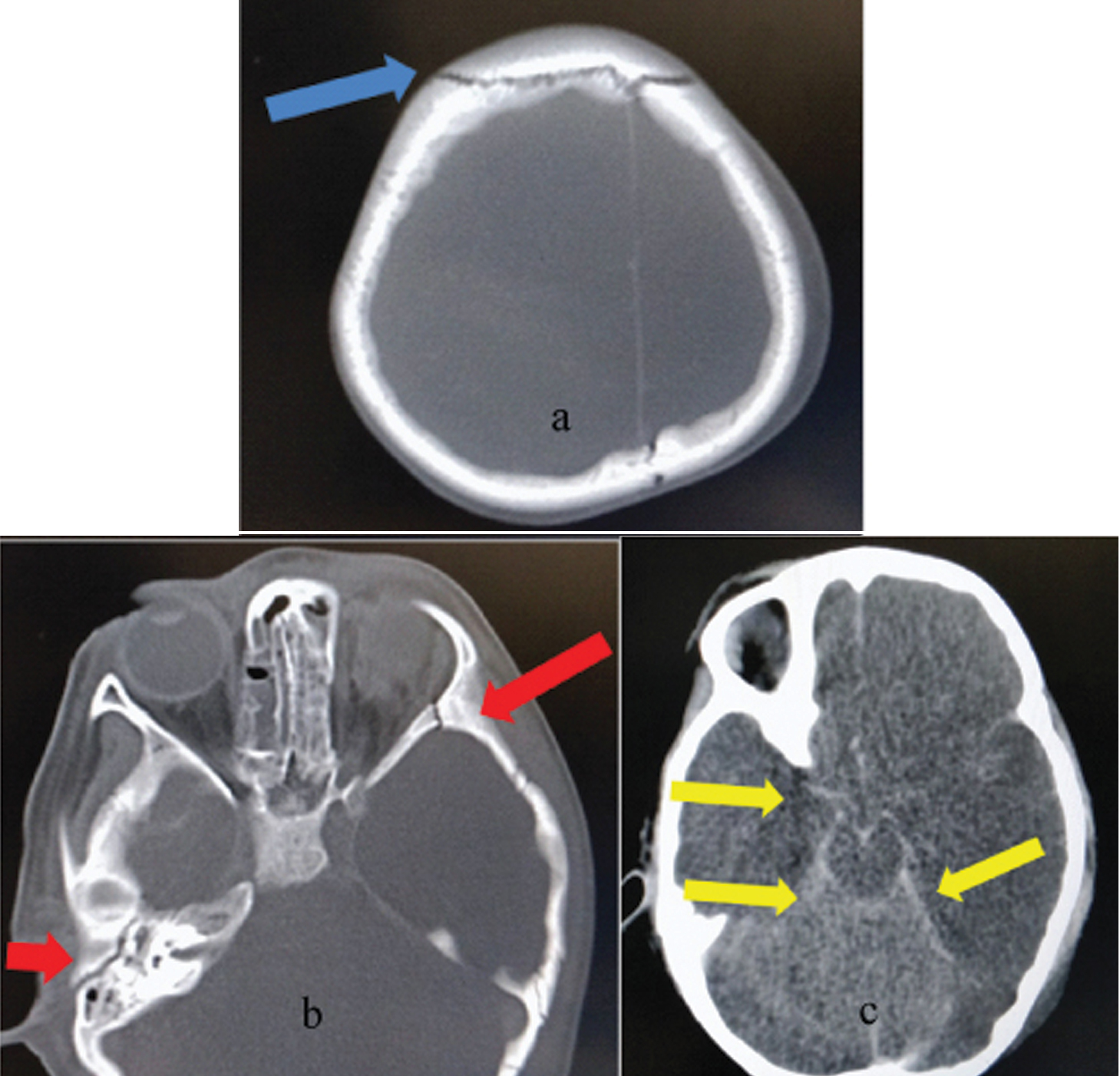
Four-year-old male patient with CT show skull bone fracture and subarachnoid haemorrhage. a) blue arrow shows sutural diastasis; b) red arrows show fracture; c) yellow arrows show subarachnoid haemorrhage. Blood within the perimesencephalic cistern and suprasellar cistern is seen as hyperdensity.
[Table/Fig-5] showed that highest number of patients with head injury were in age group between 0 to less than three years and lowest number of patients between 15 to 18 years age group.
Number of paediatric head injury patients with different age groups.
| Age groups of paediatric head injury patients | Number of paediatric head injury patients |
|---|
| 0-<3 years | 314 |
| 3 years -<6 years | 181 |
| 6 years -<9 years | 204 |
| 9 years -<12 years | 245 |
| 12 years -<15 years | 107 |
| 15 years -≤18 years | 5 |
| Total | 1056 |
From the [Table/Fig-6], it can be concluded that 60.08% (316 of 526) paediatric patients with head injury with normal CT scan were less than 9 years of age.
Number of paediatric head injury patients having normal CT scan findings with different age groups.
| Age groups of paediatric head injury patients | Number of paediatric head injury patients with Normal CT scan report |
|---|
| 0 -<3 years | 129 |
| 3 years -<6 years | 97 |
| 6 years -<9 years | 90 |
| 9 years -<12 years | 141 |
| 12 years -<15 years | 65 |
| 15 years -≤18 years | 4 |
| Total | 526 |
On comparing between two groups that is all the paediatric head injury patients of different age groups [Table/Fig-5] under study (Groups A, B, C) and paediatric patients with normal CT reports (Group A) [Table/Fig-6], the p-value was 0.0990, considered not significant (Significance level was fixed at p<0.05).
Discussion
The human body in paediatric ages is highly radiosensitive to carcinogenic effects as the cells of the body in these age groups are in the stage of division and replication [11,12]. Still due to the rapidity, veracity and easy availability, CT scan is frequently preferred as investigation for children [13]. According to International Commission on Radiological Protection (ICRP), due to presence of dividing cells and longer probable lifetime for growth of oncogenic cells, children are more radiosensitive than adults [14]. Another cause of high susceptibility of children to radiation is due to wide cellular circulation of red bone marrow [2,15].
During CT scanning of paediatric patients, there is always a tendency to put these patients under adult CT protocols causing higher radiation exposure. But this can easily be avoided by adjusting the CT parameters according to paediatric body size. Also, if a child undergoes repeated CT investigations then there will be collective radiation hazards during the lifetime of the child causing higher lifetime risks of cancer [16,17].
Children are frequently suffered from brain trauma, abdominal injury, pain abdomen etc., and these common problems can quickly and correctly diagnosed by CT scan. Also, the main cause for rising trend of CT is that by giving negative results it helps to avoid many unwanted surgical operations [1]. Moreover, relatively lower cost, wider availability, overcautious use by the clinician in the era of consumer litigations and undue pressure exerted by affording parents to perform high-end investigations for their wards play role for increased CT usage [1].
The original definition of minor traumatic brain injury was a Glasgow Coma Score (GCS) of 13–15 [18]. Traumatic Brain Injury (TBI) is a non-degradative, non-congenital injury to the brain from an outward impact which causes permanent or short lived damage of mental, physical, and psychosocial functions with decrease or changing state of consciousness [18].
A child is said to be suffered from mild traumatic brain injury, if he/she underwent brain trauma with one of the following manifestations:
If the child become unconscious for any period of time.
If the child shows any memory loss immediate before or after the injury.
If the child shows any change in mental state at the time of injury.
If the child shows focal neurologic signs which may or may not be temporary [19,20].
It is very important for the physicians to distinguish whether minor head injury patients are at risk of intracranial damage or not. To assist physicians, two sets of guidelines have been suggested: the NOC (the New Orleans Criteria) and CCHR (The Canadian Computed Tomography Head Rule) [18].
CT recommendations in guideline “Head injury in infants, children and adults: triage, assessment, investigation and early management” by National Institute of Clinical Excellence (NICE), in 2003 are similar to the Canadian CT rule. The only modifications are: in “medium risk” criteria, CT can be delayed up to eight hours and “high risk” indication for CT is coagulopathy [18].
In UK, Ionising Radiation (Medical Exposure) Regulations (IRMER), 2000 emphasises on the responsibilities of the employer and the requirements for justification and optimisation of individual exposures. Three persons are considered very important by IRMER, these are: referrer, practitioner and operator. The role of practitioner (radiologist) is to decide whether the investigation asked for is justified or not on the basis of the clinical benefit against the radiation hazards [21]. Unlike UK, in India, radiologists just report the findings of the imaging techniques and are not authorised to justify the requested investigation. Moreover, there is lack of awareness about the radiation hazards of imaging techniques among patients, patient’s attendants as well as referring physicians.
The radiology group perceived and accepted the significance of these issues, and responded by propelling a worldwide campaign for optimising the radiation doses and utilising exclusive paediatric CT guidelines. In 2008, many radiology groups including the Society of Paediatric Radiology and American College of Radiology, began the activity, appropriately named ‘Image Gently Campaign’ with the objective to feature the significance of reduction of paediatric radiation dose emphasising on CT scanning, by performing several awareness and educational activities [16]. The campaign basically underlines the idea of ‘ALARA’ which stands for ‘As Low As Reasonably Achievable’ is required to be comprehended and received by all experts involved in paediatric care with the aim to protect child from radiation exposure. It is the obligation of the clinician, who is requesting the CT investigation, to guarantee that the investigation is justified and the duty of the radiologist is to inspect that the radiation dose is minimised by adopting appropriate procedures and factors. The advantage of a correctly performed and clinically justified CT investigation ought to exceed the hazards [22].
Most recently a study has suggested that if brain cells are damaged by a Traumatic Brain Injury (TBI) event then inflammation occurs which in turn causes change in concentration of pro-inflammatory and anti-inflammatory proteins. Later, the study result showed that anti-inflammatory protein interleukin-10 might be a useful diagnostic tool which can help in distinguishing whether CT investigation is required or not in mild TBI patients [23].
Limitation
Now-a-days, all district based civil hospitals (of the state in which the present study was conducted) have been equipped with CT scan facilities which are provided at free of cost to all the patients. So these patients at rural areas go for CT because of increased tendency to make use of high level radiological services and there is also unawareness regarding the radiation hazards. Thus, the limitation of this study is that a large number of these children are not reaching the tertiary care hospitals leading to under estimation of these paediatric patients who are undergoing unnecessary CT brain in district hospitals if we consider society as a whole.
Conclusion
Total of 1056 paediatric head injury patients undergone CT scan head and out of which about 50% were diagnosed with normal CT scan report. Thus, in half of the paediatric patients CT scan could be avoided with unnecessary radiation exposure.