HF has been defined as a global pandemic, since it affects around 26 million people worldwide [1]. Clinical history, symptoms, and signs when used in isolation, have only a limited value in diagnosing HF [2]. However, noninvasive imaging technology such as MRI, Nuclear imaging such as Single Photon Emission Computed Tomography (SPECT) have come up in recent times but biochemical markers such as Cardiac Troponin I, Pro Brain Natriuretic Peptide, N-Terminal -pro Brain Natriuretic Peptide (NT-proBNP) still play an important role in diagnosis and prognosticating HF [3,4].
Cardiac biomarkers like NT-proBNP has revolutionized the diagnosis of HF and continues to dazzle across the spectrum of cardiovascular diseases in view of their versatile role [5,6]. Availability of cardiac biomarkers have not yet penetrated enough to the base line diagnostic work up in a setting of a resource poor country. Not many studies have been done in this part of the country to extrapolate its applicability to Indian set up. Certain cases of HF that present as dyspnea may pose a diagnostic dilemma where cardiac biomarkers such as NT-proBNP and Galecetin-3 can help in differential diagnosis and planning of therapy [7]. This study was intended to find out the utility of first week NT-proBNP levels as a prognostic indicator (duration of hospital stay and mortality) in various aetiologies of HF.
Materials and Methods
This was a hospital based cross-sectional study carried out from October 2015 to October 2017 in IMS and SUM hospital, Bhubaneswar which was approved by institutional ethics committee. Assuming margin of error of 5% with a confidence interval of 95% and considering population size of 300, sample size was estimated to be around 169. A total of 160 patients aged between 25 and 65 years (82 males and 78 females) admitted to the hospital with clinical evidence of HF (using Framingham’s criteria) and classified into New York Heart Association (NYHA) functional class of HF were included in the study [8]. Diagnosis of HF according to Framingham criteria requires the simultaneous presence of at least two major criteria or one major criterion in conjunction with two minor criteria. Major criteria includes Paroxysmal nocturnal dyspnea, Neck vein distention, Rales, Radiographic cardiomegaly, Acute pulmonary oedema, S3 gallop, Increased central venous pressure (>16 cm H2O at right atrium), Hepatojugular reflux, Weight loss >4.5 kg in five days in response to treatment. Minor criteria includes Bilateral ankle oedema, Nocturnal cough, Dyspnea on ordinary exertion, Hepatomegaly, Pleural effusion, Decrease in vital capacity by one third from maximum recorded, Tachycardia. The Framingham Heart Study criteria are 100% sensitive and 78% specific for identifying persons with definite congestive HF.
Those patients who had prosthetic valve replacement, ventricular pacemaker, chronic kidney disease, liver cirrhosis, anaemia, severe sepsis were excluded from the study. Informed consent was taken from all the patients. Each patient underwent thorough physical examinations including electrocardiogram, echocardiography, chest radiology, and routine laboratory tests including NT-proBNP. NT-proBNP was evaluated at admission and after one week of drug therapy, at discharge and at follow up. Out of 160 patients, 16 patients died and 20 patients were lost during follow up duration of six months.
Statistical Analysis
Statistical analysis was done using SPSS version 20. Comparisons of clinical characteristics between patients and association with risk factors were done by chi-square tests for categorical data. A p-value of <0.001 was considered significant. Correlation between variables was calculated by using regression analysis.
Results
Out of 160 patients, 82 were males (51.25%) and 78 were females (48.75%) with a mean NT-proBNP levels of 7436 and 6998 pg/dL respectively at admission. NT-proBNP levels increases with the advancement of age but it was not statistically significant.
Patients who had both Diabetes Mellitus (DM) and Hypertension (HTN) had mean NT-proBNP levels of 8612 pg/dL, which was higher than the patients with only DM (NT-proBNP levels of 5901 pg/dL) and only HTN (mean NT-proBNP levels of 6806 pg/dL) which was statistically significant (p<0.001) [Table/Fig-1].
Risk factors and its association with NT-proBNP.
| Risk factor | No. of Patients | Mean NT-proBNP levels pg/dL | Mean LVEF% |
|---|
| DM & HTN both | 76(47.5) | 8612 | 42.68 |
| DM only | 14(8.75) | 5901 | 47.142 |
| HTN only | 32(20) | 6806 | 49 |
| Alcohol | 30(18.75) | 8825 | 42.7 |
| Tobacco | 46(28.75) | 8552 | 42.478 |
| Age > 60 | 78(48.75) | 7966.128 | 43.128 |
LVEF – Left Ventricular Ejection Fraction, DM – Diabetes Mellitus, HTN – Hypertension
Alcohol use disorder – satisfying DSM-5 criteria
Tobacco – those who have smoked at least 100 cigarettes in their lifetime and currently may or may not smoke
The most common aetiology for HF in this study was Ischemic Heart Disease (IHD) n=76(47.5). NT-proBNP levels were highest in groups of HF with aetiology of Rheumatic Heart Disease (RHD) and myocarditis, and lowest with aetiology of Subacute Bacterial Endocarditis (SBE) and cor-pulmonale [Table/Fig-2].
Specific aetiology of heart failure and its association with NT-proBNP.
| Aetiology | No. of Patients | Average EF% | NT-proBNP |
|---|
| IHD | 76 (47.5) | 40 | 9029 |
| DCM | 18(11.25) | 33.5 | 3926 |
| RHD | 6 (3.75) | 55.3 | 13583 |
| Myocarditis | 18 (11.25) | 53.7 | 9176.77 |
| Cor-pulmonale | 40(25) | 52.7 | 3634.8 |
| SBE | 2 | 46 | 3340 |
EF – Ejection Fraction, IHD – Ischemic Heart Disease, DCM – Dilated Cardio Myopathy, RHD – Rhe umatic Heart Disease, SBE – Subacute Bacterial Endocarditis
Most of the patients were of NYHA class IV n=78(48.5%). It was observed that as NYHA class increased and Left Ventricular Ejection Fraction (LVEF) decreased, NT-proBNP levels increased which was statistically significant (p<0.001) [Table/Fig-3]. The average duration of the hospital stay also increased with the increase in average NT-proBNP levels (r2 = 0.4936) [Table/Fig-3].
NYHA grades of heart failure and its correlation with ejection fraction, NT-proBNP and hospital stay (r2 = 0.49).
| NYHA Class | No. of Patients (N=160) | Avg. NT-proBNP (pg/dL) | Avg. EF % | Average duration of hospital stay in days |
|---|
| I | 8 (5) | 794 | 64 | 3.3 |
| II | 24 (15) | 1990 | 53.91 | 4.3 |
| III | 50 (31.25) | 4533 | 47.24 | 7.3 |
| IV | 78 (48.75) | 11215 | 38.358 | 10.9 |
EF- Ejection Fraction
Average NT-proBNP levels in patients with aetiology of IHD were 9029 pg/dL and that of other aetiologies combined was 6731 pg/dL which was statistically non-significant (p-value 0.0238).
Interestingly, there was a statistically significant difference (p<0.001) in NT-proBNP levels with pulmonary cause of HF i.e., cor-pulmonale patients (3634.8 pg/dL) vs patients with non-pulmonary causes of HF (8418.7 pg/dL). Those with NYHA class IV HF, the mean NT-proBNP levels in patients with cor-pulmonale was 6000 pg/dL in comparison to 12,561 pg/dL in patients with non cor-pulmonale patients which was statistically significant (p<0.001).
NT-proBNP levels in cor-pulmonale patients with LVEF <50% (HFrEF) (n=10) had a mean NT-proBNP level of 7056 and LVEF ≥ 50% (HFpEF) (n =30) had a mean NT-proBNP level of 2494 pg/dL which was statistically significant with p-value of <0.0001.
NT-proBNP levels were found to be higher in patients of age above 60 years as compared to those below 60 years. 82 (51.25%) patients were below 60 years of age had mean NT-proBNP values of 6515 pg/mL, whereas 78 (48.75%) patients aged above 60 years had mean values of 7966.1 pg/mL which were statistically insignificant.
Mean NT-proBNP levels of all cases of HF at time of diagnosis was 7649.5 pg/dL and values of NT-proBNP levels post treatment at one-week interval was 2952 pg/dL.
In this study 160 cases were followed up in a span of six months following discharge, out of which 124 patients survived, 20 were lost in follow up and 16 died during subsequent follow up. Mean NT-proBNP levels at time of admission was much lower in patients who were alive (5,561 pg/dL) than patients who died within six months of follow-up (18,554 pg/dL) (p<0.001).
The mean repeat NT-proBNP levels at one-week post treatment who survived was 566.1 pg/dL and those who died during subsequent follow-up was 11,316.4 pg/dL respectively. This comparison was statistically significant with p<0.001 [Table/Fig-4].
Age, LVEF, NT-proBNP levels at time of admission and post one-week treatment in patients who survived versus patients who died during treatment and follow up of six months.
| Patients who were alive at six months follow up (n=124) | Patients who died during treatment and six months follow up (n=16) |
|---|
| Mean age in years | 62.5 | 65.2 |
| Average LVEF% | 45.8 | 32.2 |
| Mean NT-proBNP in pg/dL at admission | 5,561 .1 | 18,554 |
| Mean NT-proBNP in pg/dL at one-week post therapy | 566.1 | 11,316.4 |
LVEF – Left Ventricular Ejection Fraction
Chi-square test was used to calculate significance. p-value was <0.001 for all groups which was considered significant.
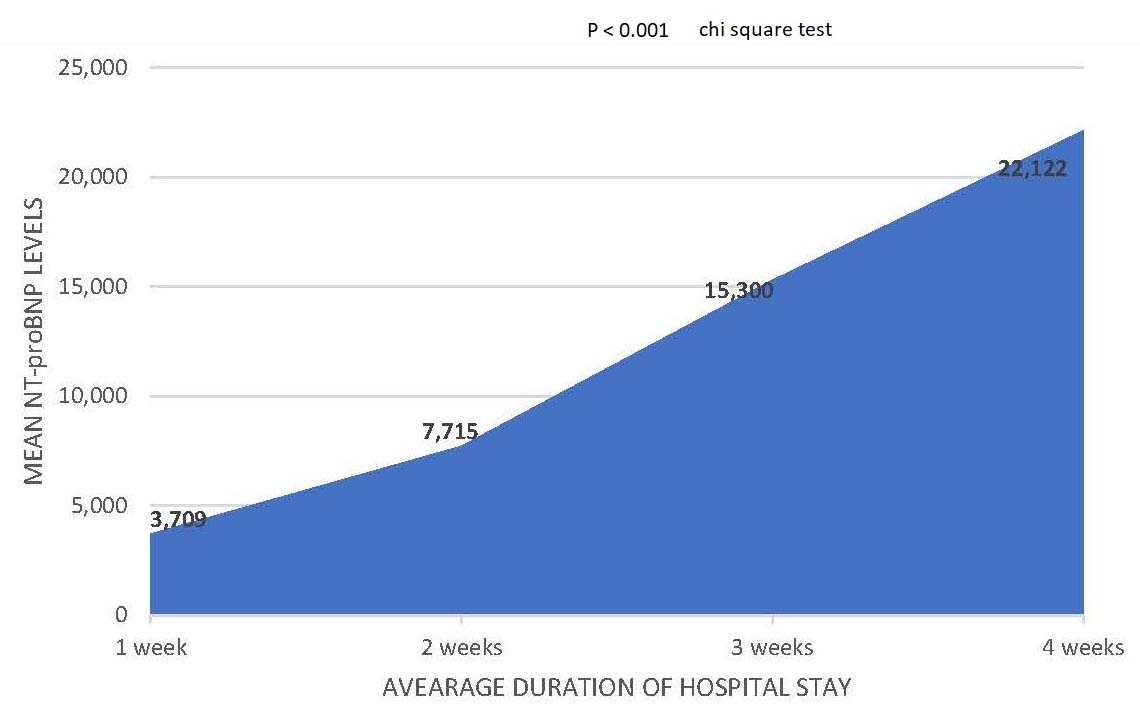
It was observed that patients who were discharged within 1st, 2nd, 3rd and 4th weeks of hospital stay had mean NT-proBNP levels of 3,709 pg/dL, 7,715 pg/dL, 15,300 pg/dL, 22,122 pg/dL respectively. This was statistically significant with p<0.001 [Table/Fig-5].
Correlation of average duration of hospital stay in weeks with Mean NT-proBNP levels (p<0.001).
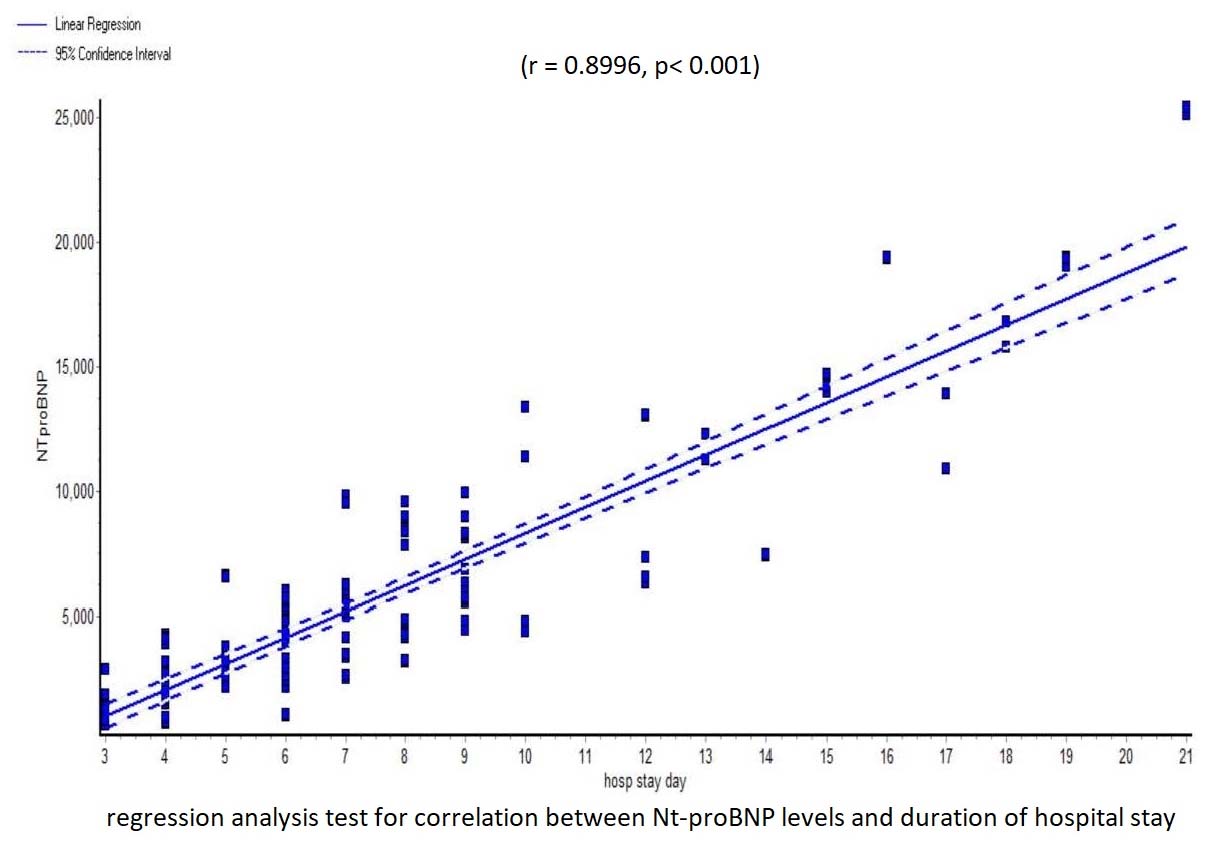
A significant positive correlation was found between NT-proBNP levels at the time of admission and duration of hospital stay using regression analysis. (r=0.8996, p<0.001) [Table/Fig-6].
Correlation between NT-proBNP levels at admission and hospital stay in days (r=0.8996, p<0.001).
Regression analysis test was used to calculate correlation between NT-proBNP levels at admission and hospital stay in days.
Discussion
In present study the average levels of NT-proBNP were 7222.72 pg/dL amongst the patients. Januzzi JL et al., showed that for diagnosis of acute congestive HF cut off of >450 pg/mL and >900 pg/mL for <50 year and >50 year group respectively were highly sensitive and specific [9]. Ozturk TC et al., found in their study that the mean NT-proBNP value of the patients was 9741.9±8973 pg/mL [10].
In the present study out of total 160 patients 82 (51.25%) were male and 78 (48.75%) were female with a mean NT-proBNP levels of 7436 pg/dL and 6998 pg/dL respectively. This study had almost equal proportion of male and female cases. There was no significant difference in the NT-proBNP values among males and females for a given NYHA class heart failure and for a given LVEF. Studies done by Seino Y et al., showed significant higher values in females for a given class of HF [11].
Patients with Ejection Fraction (EF) less than 40% had a mean NT-proBNP levels of 11374.8 pg/dL, between 40-49% had a mean NT-proBNP levels of 7175.7 pg/dL and more than 50% had a mean NT-proBNP levels of 3685. In this study NT-proBNP levels were inversely proportional to the EF. These results are in tune with PRIDE study and Seino Y et al., study [9,11].
Higher values of NT-proBNP were observed in patients of age above 60 years as compared to those below 60 years which were statistically insignificant. Bay M et al., showed higher values of NT-proBNP in elderly patients [12]. The cause of which was attributed to poorer Glomerular Filtration Rate in elderly patients. This justifies that age could behave as a confounding factor provided a different cut off was taken for elderly and others.
It was found that highest number of patients had IHD {n=76(47.5%), with higher range of NT-proBNP levels (9029 pg/dL} when compared with non-ischemic heart disease {n=84(52.5%) with their mean NT-proBNP levels of 6731 pg/dL which was consistent with COPERNICUS sub-study [13].
Patients of HF presented with Myocarditis had a mean NT-proBNP level of 9176.7 pg/dL even when they had higher levels of EF, when compared to the patients with IHD with low EF, who had mean NT-proBNP levels of 9029 pg/dL. No similar observation was reported in other studies.
From this study it was found that the mean NT-proBNP levels of patients with Cor-pulmonale was significantly lower (3634.8 pg/dL) than patients of HF with non- pulmonary cause (8418 pg/dL). Observations by Blyth KG et al., was consistent with this study [14].
In patients with NYHA class IV HF, the mean NT-proBNP levels in patients with cor-pulmonale was significantly lower in comparison to patients with non cor-pulmonale patients (p<0.001).
It was also found that cor-pulmonale patients with LVEF <50% has significant higher NT-proBNP levels (7056 pg/dL) when compared to those with normal ejection fraction (2494 pg/dL). This disproportionate increase in NT-proBNP levels in cases of cor-pulmonale is probably due to associated LV dysfunction.
Differences in age, LVEF, and mean NT-proBNP levels were compared in patients who were alive and patients who died during treatment or follow up and it was found that mean NT-proBNP levels at time of admission was much lower in patients who were alive at six months (5,561 pg/dL) versus the patients who died within six months of follow-up (18,554 pg/dL) (p=0.001). Study by Pereira-Barretto AC et al., was consistent with observations of this study [15].
The patients who were alive at follow up had a significantly lower mean NT-proBNP levels at the time of admission and 1st week post therapy as compared to those who died during the follow-up period of six months (p<0.001).
Patients with NT-proBNP levels more than 15,000 pg/dL invariably stayed more than two weeks. Patients who had higher levels of NT-proBNP (>10,000 pg/dL) at time of admission, had higher risk of mortality. Higher the levels of NT-proBNP at time of admission, more was the duration of hospital stay (p <0.001).
Patients, whose NT-proBNP levels were less than 1,000 pg/dL after one week of follow up, responded to the therapy, survived and were discharged in less than two weeks. The decline of NT-proBNP levels more than 90% of the initial values in one week follow up NT-proBNP were prognostic marker for recovery with p-value of <0.01.
Patients who had NT-proBNP levels of more than 10,000 pg/dL, and or the fall of NT-proBNP levels less than 50% after one week of therapy had higher risk of mortality and increased duration of hospital stay. Similar finding couldn’t be found in other studies.
This study highlights the plausibility of the routine use of NT-proBNP in monitoring the response of therapy and also prognosticate the outcome, hospital stay, and mortality risk of various cases of HF after one week of therapy which have not been depicted in other studies especially in an Indian scenario.
Limitation
Around 20 out of 160 patients were lost to follow up in the six months following discharge from the hospital. Around 13 patients developed acute kidney injury during the course of treatment which might act as a confounding factor in the interpretation of NT-proBNP levels in those patients. Sample size was relatively small due to socio-economic constraints.
Conclusion
In view of extreme morbidity and mortality, HF need to be diagnosed, treated and prognosticated in real time to avoid fatal outcomes. This study highlights the importance of temporal rise or fall of first week NT-proBNP levels as a routine marker to assess the response to treatment and prognosticate individual cases of HF in a tertiary care setup.
LVEF – Left Ventricular Ejection Fraction, DM – Diabetes Mellitus, HTN – Hypertension
Alcohol use disorder – satisfying DSM-5 criteria
Tobacco – those who have smoked at least 100 cigarettes in their lifetime and currently may or may not smoke
EF – Ejection Fraction, IHD – Ischemic Heart Disease, DCM – Dilated Cardio Myopathy, RHD – Rhe umatic Heart Disease, SBE – Subacute Bacterial Endocarditis
EF- Ejection Fraction
LVEF – Left Ventricular Ejection Fraction
Chi-square test was used to calculate significance. p-value was <0.001 for all groups which was considered significant.