Bouveret’s Syndrome: A Rare Case Presentation
Dhvani Bharat Shah1, Hiranya Deka2, Priyanka Gopal Chilbule3, Rajesh Kumar C Mahley4, Divakar Jain5
1 Junior Resident, Department of General Surgery, Topiwala National Medical College and B.Y.L. Nair Hospital, Mumbai, Maharashtra, India.
2 Junior Resident, Department of General Surgery, Topiwala National Medical College and B.Y.L. Nair Hospital, Mumbai, Maharashtra, India.
3 Junior Resident, Department of General Surgery, Topiwala National Medical College and B.Y.L. Nair Hospital, Mumbai, Maharashtra, India.
4 Associate Professor, Department of General Surgery, Topiwala National Medical College and B.Y.L. Nair Hospital, Mumbai, Maharashtra, India.
5 Junior Resident, Department of General Surgery, Topiwala National Medical College and B.Y.L. Nair Hospital, Mumbai, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Dhvani Bharat Shah, 503, Mathrubhumi, Shree Nagar Colony, Off M.G. Road, Goregaon (W), Mumbai-400104, Maharashtra, India.
E-mail: dhvani_shah15@yahoo.in
Gall stone ileus is a rare complication of gall stones. A rarer entity is Bouveret’s syndrome which causes gastric outlet obstruction due to migration of gall stones into duodenal bulb through cholecystoduodenal fistula. Bouveret’s syndrome constitutes 1–3% of the cases of gall stone ileus which in turn complicates only 0.3–4% cases of cholelithisasis. Bouveret’s syndrome is managed surgically.
The present case is of a 66-year-old man who presented with gastric outlet obstruction and was diagnosed with Bouveret’s syndrome later. Bouveret’s syndrome is an uncommon condition whose awareness is essential as it may pose a difficulty in diagnosis.
Cholecystoduodenal fistula, Gall stone ileus, Gastric outlet obstruction
Case Report
A 66-year-old man presented with complaints of recurrent mild pain in the epigastrium, radiating to the right hypochondriac region for the last one year, aggravated since one month. This was associated with multiple episodes of projectile, non-bilious vomiting containing food particles. Patient had history of constipation since one month. He was a known case of diabetes mellitus since one year and was on treatment (oral hypoglycemic drugs). Patient had no other significant history.
On abdominal examination, there was mild tenderness in the epigastrium without guarding or rigidity. No organomegaly was present. Blood parameters were normal. Chest and abdominal radiographs were not contributory. An ultrasonography of the abdomen revealed dilated small bowel loops, and rest was normal. An upper gastro-intestinal endoscopy was performed which revealed residual food particles and a normal pyloric region. The scope could not be negotiated beyond pylorus. In view of inconclusive Oesophago gastro duodenoscopy (OGD) findings, a Contrast Enhanced Computed Tomographic (CECT) scan [Table/Fig-1] of abdomen was done which depicted a circumferential wall thickening at pyloroduodenal junction causing gastric outlet obstruction with acute calculous cholecystitis with cholecystoduodenal fistula connecting gall bladder and first part of duodenum. Air specks were noted in the gall bladder.
CECT showing cholecystoduodenal fistula.

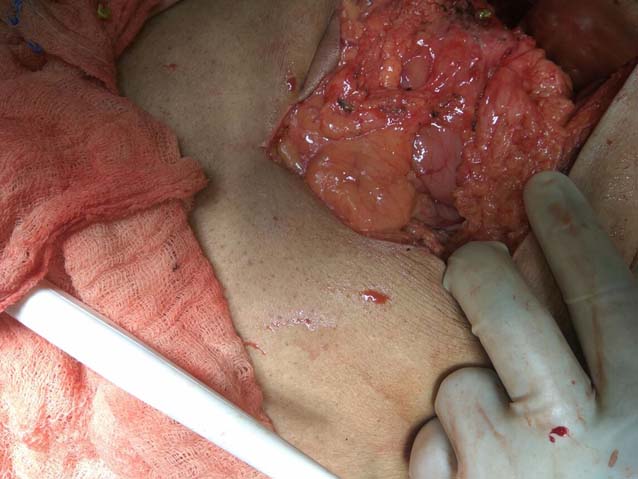
In view of the CT scan findings, decision for exploratory laparotomy was taken after stabilisation of the patient. Operative findings included multiple adhesions of the fundus of the gall bladder with first part of duodenum with dense adhesion in infra-hepatic region. Firm constricting thickening in the pylorus was felt. Multiple stones were present in the gall bladder and a single large stone measuring 1.5cm in diameter was found in the first part of the duodenum [Table/Fig-2].
Intraoperative picture showing gall stone at the first part of duodenum.

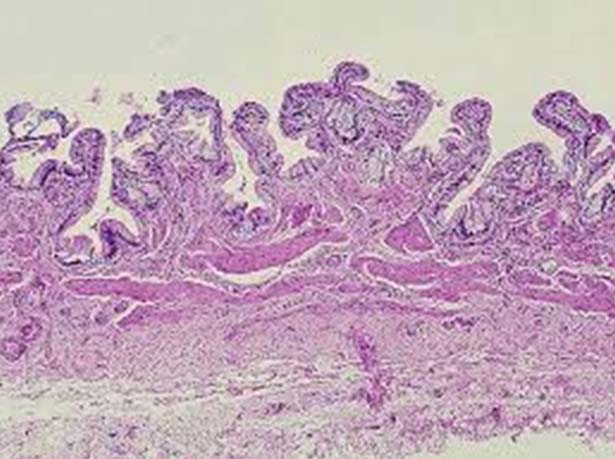
Cholecystectomy with primary suturing of duodenal perforation with omentoplasty with retrocolic gastro-jejunostomy [Table/Fig-3] was performed. Postoperative period was uneventful and the patient was discharged on postoperative day seven. Histopathological examination showed benign calculous cholecystitis [Table/Fig-4]. Mild chronic inflammation with Rokitansky-Aschoff sinuses, granulomas, smooth muscle hypertrophy, hyalinised collagen, dystrophic calcification, lymphoid aggregates was seen.
Intraoperative picture - repair of fistula and gastrojejunostomy was done.
Histopathology (H&E stain, X20) showing chronic calculous cholecystitis with chronic inflammation and Rockitansky-Aschoff sinuses.
Discussion
Gall stone ileus is a known complication of cholelithiasis (0.3–4%). In descending order, the most common level of obstruction is the terminal ileum (60–70%), followed by the proximal ileum (25%), distal ileum (10%), jejunum (9%), colon (4%), rectum (2%), and lastly the duodenum (1–3%) [1,2]. Cholecystoenteric fistulas are a rare complication of gall stone disease and affects 3-5% cases of cholelithiasis. Fistula formation is thought to occur as a result of adhesions between the gall bladder and the bowel wall secondary to chronic inflammation and ischemia. This causes pressure necrosis of the gall bladder and passage of stone through the fistula which may get enlarged due to accumulation of salts and fecal matter on its surface. The incidence of cholecystoduodenal fistula is 19%. Bouveret’s syndrome is a term used for gastric outlet obstruction due to cholecystoduodenal fistula. It is 3 to16 times more common in the females than in males. Early diagnosis is important because of high mortality. This syndrome was first described by Beaussier [1] in 1770 but it has been named after the French physician Bouveret L after his publication of two case reports in the Revue Medicale in 1896 [1].
Risk factors for Bouveret’s syndrome are age more than 70 years, female gender, gall stones more than 2.5 cm in size, post surgical altered gastrointestinal anatomy. Symptoms include vomiting (87%), abdominal pain (71%), hematemesis (15%), recent weight loss (14%), anorexia (13%) [2]. Common signs encompass abdominal tenderness (44%), signs of dehydration (31%), abdominal distension (26%). Extrinsic duodenal compression by a massively enlarged gall bladder containing multiple calculi may also cause gastric outlet obstruction (pseudo-Bouveret’s syndrome). Bouveret’s syndrome results in complications such as duodenal perforation, hematemesis (Mallory-Weiss tear), distal oesophageal rupture (Boerhaave’s syndrome), gastric bezoar [2].
Abdominal X-ray shows Rigler’s triad (pneumobilia, small bowel obstruction and gall stones) in the cases of gall stones ileus [3,4]. Ultrasonography of the abdomen reveals fluid filled distended stomach, features suggestive of cholecystitis, ectopic gall stone, pneumobilia [3]. CT scan is the best imaging modality to detect Rigler’s triad. CECT abdomen is more sensitive [5,6]. It can demonstrate the exact site of obstruction, fistula and gall bladder status. Magnetic Resonance Cholangiopancreatography (MRCP) has main utility in patients intolerant to oral contrast [7]. Upper gastro-instestinal endoscopy is both diagnostic and therapeutic.
Treatment options available are endoscopic, open surgery and laparoscopic approach [2].
Endoscopic Methods: Endoscopic approaches include endoscopic extraction, endoscopic laser lithotripsy, extracorporeal shockwave lithotripsy [8] and intra-corporeal electrohydraulic lithotripsy [9]. Endoscopic management uses different sized and shaped snares, grasping forceps, retrieval baskets and nets, biliary balloons [10], and a side-viewing endoscope. This is technically challenging and has obtained lower success rates in the past (<10%) [11,12].
Surgical Methods: Failure of endoscopic procedure, stone size >2.5 cm, residual stone in the gall bladder, sepsis, perforation, multiple stones in the intestinal lumen indicates an open approach. [14]. Open surgery involves enterolithotomy with cholecystectomy with fistula repair [13]. Usually enterolithotomy is performed at the site of impaction. Bouveret syndrome still has high mortality rate (35%) attributed to characteristics of the affected population like elderly population with comorbidities and due to delayed diagnosis. Surgical procedures also carry the mortality of 17% in one-stage procedure and 12% for enterolithotomy [14].
An open enterolithotomy with cholecystectomy with fistula repair and gastro-jejunostomy was done in our case. As the patient was well-optimised with no co-morbidities, enterolithotomy and cholecystectomy with fistula repair and gastrojejunostomy was done in a single sitting.
Bedogni G et al., in the year 1985 had reported a similar case of 84-year-old female with Bouveret’s syndrome who had undergone endoscopic extraction of stone at the duodenum [12]. Kalwaniya DS et al., reported a similar case of a 40-year-old female with gastric outlet obstruction with cholecystojejunal fistula repair with cholecystectomy and gastrojejunostomy [13].
Nickel F et al., in their study reported two cases of Bouveret’s syndrome, a 74-year-old male with cholecystoduodenal fistula who underwent open cholecystectomy with gastrojejunostomy without fistula repair and another 78-year-old male with cholecystoduodenal fistula and stone in the proximal jejunum who underwent open laparotomy with cholecystectomy and stone extraction with duodenojejunostomy [14].
Conclusion
Bouveret’s syndrome creates a diagnostic dilemma for which high degree of suspicion is required if a case of cholelithiasis presents with gastric outlet obstruction. The management depends on the site of the stone lodgement, the pathological attrition and the anatomical distortions caused by the stone.
[1]. Bouveret L, Stenose du pylore adherent a la vesicleRev Med 1896 16:1 [Google Scholar]
[2]. Sica GS, Sileri P, Gaspari AL, Laparoscopic treatment of Bouveret’s syndrome presenting as acute pancreatitisJSLS: Journal of the Society of Laparoendoscopic Surgeons 2005 9(4):472 [Google Scholar]
[3]. Trubek S, Bhama JK, Lamki N, Radiological findings in bouveret’s syndromeEmergency Radiology 2001 8(6):335-37.10.1007/PL00011935 [Google Scholar] [CrossRef]
[4]. Rigler LG, Borman CN, Noble JF, Gallstone obstruction: pathogenesis and roentgen manifestationsJournal of the American Medical Association 1941 117(21):1753-59.10.1001/jama.1941.02820470001001 [Google Scholar] [CrossRef]
[5]. Singh AK, Shirkhoda A, Lal N, Sagar P, Bouveret’s syndrome: appearance on CT and upper gastrointestinal radiography before and after stone obturationAmerican Journal of Roentgenology 2003 181(3):828-30.10.2214/ajr.181.3.181082812933489 [Google Scholar] [CrossRef] [PubMed]
[6]. Yu CY, Lin CC, Shyu RY, Hsieh CB, Wu HS, Tyan YS, Value of CT in the diagnosis and management of gallstone ileusWorld Journal of Gastroenterology: WJG 2005 11(14):214210.3748/wjg.v11.i14.214215810081 [Google Scholar] [CrossRef] [PubMed]
[7]. El Sorogy M, El Hanafy E, Hamed H, Atef E, Rafee AA, El-Ebeidy G, Bouveret’s syndrome: a report of two casesThe Egyptian Journal of Surgery 2016 35(4):45610.4103/1110-1121.194730 [Google Scholar] [CrossRef]
[8]. Langhorst J, Schumacher B, Deselaers T, Neuhaus H, Successful endoscopic therapy of a gastric outlet obstruction due to a gallstone with intracorporeal laser lithotripsy: a case of Bouveret’s syndromeGastrointestinal Endoscopy 2000 51(2):209-13.10.1016/S0016-5107(00)70421-4 [Google Scholar] [CrossRef]
[9]. Gemmel C, Weickert U, Eickhoff A, Schilling D, Riemann JF, Successful treatment of gallstone ileus (Bouveret’s syndrome) by using extracorporal shock wave lithotripsy and argon plasma coagulationGastrointestinal Endoscopy 2007 65(1):173-75.10.1016/j.gie.2006.05.02517137860 [Google Scholar] [CrossRef] [PubMed]
[10]. Lübbers H, Mahlke R, Lankisch PG, Gallstone ileus: endoscopic removal of a gallstone obstructing the upper jejunumJournal of Internal Medicine 1999 246(6):593-97.10.1046/j.1365-2796.1999.00597.x10620104 [Google Scholar] [CrossRef] [PubMed]
[11]. Thompson RJ, Gidwanai Caddy G, McKenna E, McCallion K, Endoscopically assisted minimally invasive surgery for gallstonesIrish Journal of Medical Science 2009 178(1):85-87.10.1007/s11845-007-0096-917973154 [Google Scholar] [CrossRef] [PubMed]
[12]. Bedogni G, Contini S, Meinero M, Pedrazzoli C, Piccinini GC, Pyloroduodenal obstruction due to a biliary stone (Bouveret’s syndrome) managed by endoscopic extractionGastrointestinal Endoscopy 1985 31(1):36-38.10.1016/S0016-5107(85)71965-7 [Google Scholar] [CrossRef]
[13]. Kalwaniya DS, Arya SV, Guha S, Kuppuswamy M, Chaggar JG, Ralte L, A rare presentation of gastric outlet obstruction (GOO)–The Bouveret’s syndromeAnnals of Medicine and Surgery 2015 4(1):67-71.10.1016/j.amsu.2015.02.00125830020 [Google Scholar] [CrossRef] [PubMed]
[14]. Nickel F, Müller-Eschner MM, Chu J, von Tengg-Kobligk H, Müller-Stich BP, Bouveret’s syndrome: presentation of two cases with review of the literature and development of a surgical treatment strategyBMC Surgery 2013 13(1):3310.1186/1471-2482-13-3324006869 [Google Scholar] [CrossRef] [PubMed]