A Case of Infective Pulmonary Endarteritis in a Young Male
Surender Deora1, Pawan Garg2
1 Assistant Professor, Department of Cardiology, All India Institute of Medical Sciences, Jodhpur, Rajasthan, India.
2 Assistant Professor, Department of Diagnostic and Interventional Radiology, All India Institute of Medical Sciences, Jodhpur, Rajasthan, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Surender Deora, Assistant Professor, Department of Cardiology, All India Institute of Medical Sciences, Jodhpur-342005, Rajasthan, India.
E-mail: drsdeora@gmail.com
Atrial septal defect, Pulmonary artery, Pulmonary infarct, Pulmonary stenosis, Vegetation
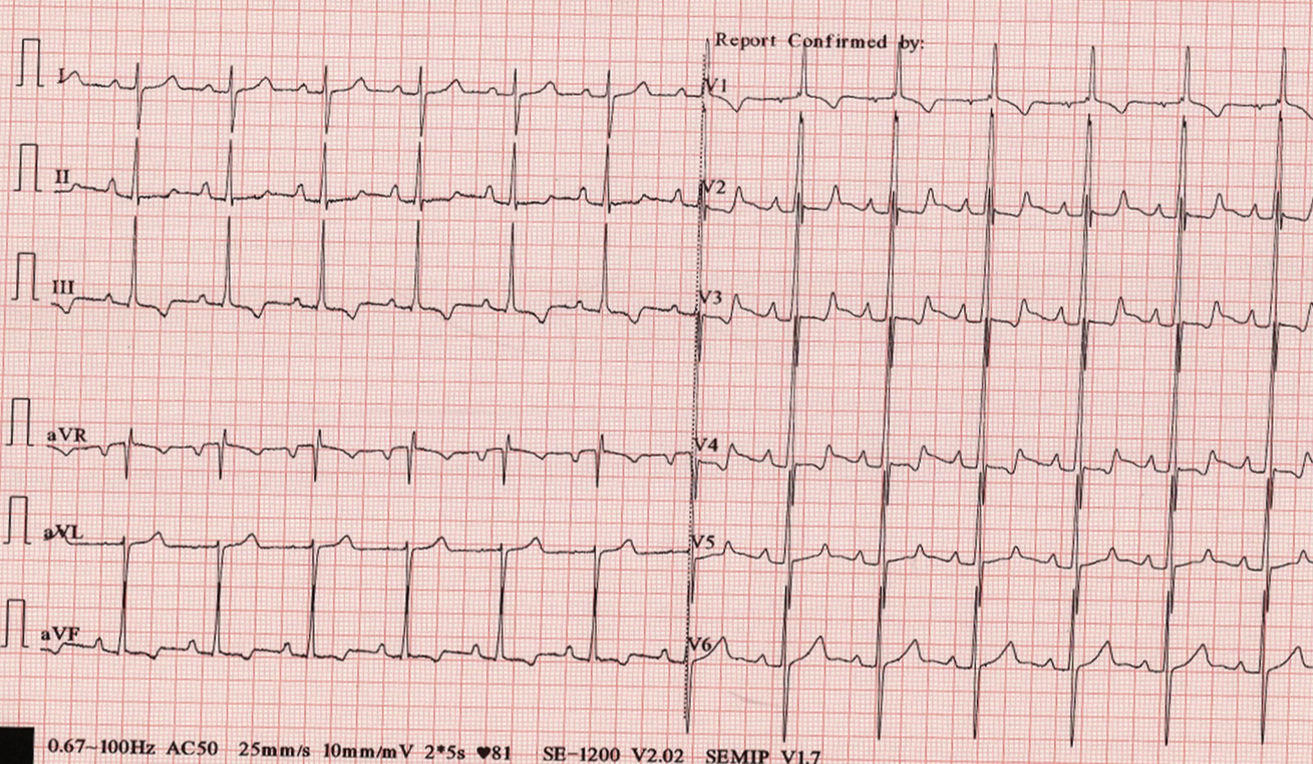
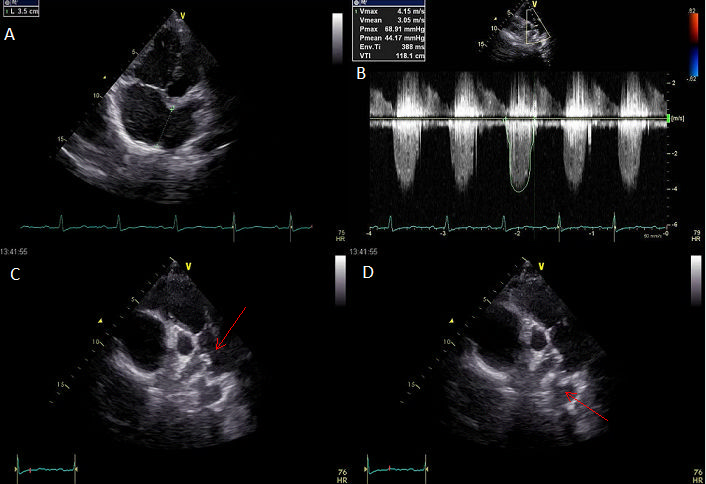
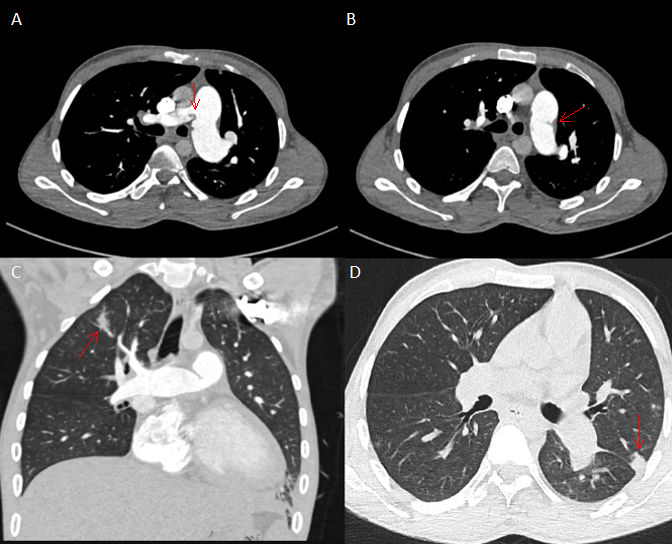
A 21-year-old male was admitted to the hospital with a complaint of low grade fever, shortness of breath, fatigue and palpitations (NYHA II) of 1-month duration. He was treated at a primary health centre and was diagnosed to have heart problem and thus referred to higher centre. There was no significant relevant past history or any history of hospitalisation. On general clinical examination, patient was febrile with temperature 99oF with conjunctival pallor. Cardiovascular examination revealed thrill in second left intercostal space near to sternum, wide and fixed second heart sound with grade IV/VI ejection systolic murmur heard all over the precordium. 12-lead Electrocardiogram (ECG) showed significant ‘R’ wave in V1 with inverted ‘T’ waves in V1, III, aVF and right axis deviation suggestive of right ventricular pressure overload haemodynamics [Table/Fig-1]. Chest X-ray was unremarkable and no significant findings [Table/Fig-2]. Transthoracic echocardiography showed large ostium secundum atrial septal defect (35 mm) and significant pulmonary valve stenosis with peak systolic gradient of 69 mmHg and mean systolic gradient of 44 mmHg. It also revealed small mobile vegetations in left and right pulmonary artery near bifurcation [Table/Fig-3]. The laboratory findings included a haemoglobin of 8 gm/dL, white cell count of 15,300/mm3 with predominant neutrophils. Liver and renal functions were within normal limits. Three blood culture specimens collected on separate occasions was sent for growth and sensitivity. A provisional diagnosis of infective pulmonary endarteritis was made and patient was treated with ceftriaxone and gentamycin while awaiting the blood culture results. Blood culture was positive for Streptococcusviridans and sensitive to ceftriaxone and gentamycin. Patient improved symptomatically and the course was satisfactory until 12 days after treatment when patient developed sharp, severe localized chest pain in left lower axilla and right upper chest which increased with coughing. Clinical suspicion of septic pulmonary infarct was made and Computerised Tomography (CT) thorax was done which revealed small peripheral wedge shape infarct in right and left upper lobes of lung and also showed vegetations in pulmonary arteries on angiography [Table/Fig-4]. Patient was managed medically with antibiotics for four weeks and discharged in a haemodynamically stable condition and was advised intracardiac repair.
12-lead electrocardiogram showing right axis deviation with significant ‘R’ wave in V1 with inverted ‘T’ waves in V1, III, aVF.
Chest X-Ray Postero-Anterior (PA) view with no significant findings.

Panel A) Transthoracic 2D and Doppler echocardiography: Large atrial septal defect (35 mm); Panel B) Doppler echocardiography revealing severe pulmonary valve stenosis with pressure gradient 69/44 mm Hg; Panel C) Small vegetation seen at main pulmonary artery bifurcation (Arrow); Panel D) left pulmonary artery (Arrow).
Panel A, B) Computerised tomography: Axial images of pulmonary angiography showing small vegetations at bifurcation of main pulmonary artery and in left pulmonary artery (arrow); Panel C, D) Coronal and axial lung window showing small peripheral wedge shape infarct in right and left upper lobes of lung (Arrow).
Right-sided infective endocarditis is rare because of low pressure haemodynamics and is seen in 10% cases of infective endocarditis [1]. In adults, usually it is seen in patients with intravenous drug use or central catheter use with tricuspid valve involvement alone or in combination with pulmonary valve [2]. It may also be seen in patients with congenital heart diseases like Atrial Septal Defect (ASD) and Ventricular Septal Defect (VSD) [3-4]. Infective involvement of pulmonary artery leading to pulmonary endarteritis has been reported in patients with Patent Ductus Arteriosus (PDA) but to the best of our knowledge, has never been reported in patient with ASD and pulmonary stenosis [5].
In conclusion, prolonged fever with precordial murmurs should make clinical suspicion of infective endocarditis. Pulmonary artery should be evaluated even if no vegetation is seen at tricuspid valve and pulmonary valve in ASD patients. Chest pain during treatment of right sided infective endocarditis should make clinical suspicion of septic pulmonary infarction.
[1]. Vereckei A, Vándor L, Halász J, Karádi I, Lengyel M, Infective endocarditis resulting in rupture of sinus of valsalva with a rupture site communicating with both the rightatrium and right ventricleJ Am Soc Echocardiogr 2004 17:995-97.10.1016/j.echo.2004.04.03315337966 [Google Scholar] [CrossRef] [PubMed]
[2]. Akram M, Khan IA, Isolated pulmonic valve endocarditis caused by group B streprococcus (Streptococcus agalactiae)-a case report and literature reviewAngiology 2001 52:211-15.10.1177/00033197010520030911269786 [Google Scholar] [CrossRef] [PubMed]
[3]. Shimbo M, Watanabe H, Abe T, Sato T, Koyama T, Yamamoto H, Ito H, Isolated atrial septal defect complicated by tricuspid valve infective endocarditisIntern Med 2015 54:2463-65.10.2169/internalmedicine.54.423326424304 [Google Scholar] [CrossRef] [PubMed]
[4]. Fazlinezhad A, Fallah A, Esfahanizadeh J, Pulmonic valve endocarditis with pulmonary artery endarteritis in a young man with congenital ventral septal defectARYA Atheroscler 2010 6:42-44. [Google Scholar]
[5]. Bilge M, Uner A, Ozeren A, Aydin M, Demirel F, Ermis B, Pulmonary endarteritis and subsequent embolization to the lung as a complication of a patent ductusarteriosus-a case reportAngiology 2004 55:99-102.10.1177/00033197040550011514759097 [Google Scholar] [CrossRef] [PubMed]