T2DM is a chronic metabolic condition with hyperglycaemia due to insulin resistance [1]. T2DM is a concern world over as it is increasing at a startling rate, particularly in developing countries. The International Diabetes Federation (IDF) reported that the total number of people with diabetes in India was 72.9 million in 2017 and this would rise to 119.6 million by the year 2045 [1]. Increased prevalence of T2DM in India is primarily attributed to lifestyle changes and other factors associated with societal transitions [2].
T2DM is a complex, chronic illness requiring continuous medical care. Patient self-management programs are critical in preventing acute complications and reducing the risk of long-term complications [3]. Self-management of T2DM often involves lifestyle modification (including glucose management, dietary management, physical activities, stress management, drug adherence), periodic health review while managing their health expenditure on a routine basis for a lifetime [3-6].
Based on existing literature, three parameters emerge as key factors influencing the HbA1c viz., knowledge about diabetes, patients’ attitude towards management of diabetes and the practice of self-management [7,8]. Furthermore, these parameters are significantly associated with age, gender, educational status, duration of diabetes and history of previous hospitalization [7-10].
T2DM, being chronic lifestyle disorder, requires a high level of motivation for self-management [3]. While people have access to exhaustive information on diabetes and its self-management through easy sources like internet, family, friends and quacks, this also poses a real challenge for healthcare teams. This is so, especially because most of the information available freely is not reliable. It is imperative to facilitate uptake of the right information and behaviour through planned and well-structured educational modules on diabetes self-management [11,12]. The investigation of the comprehensive relationship between knowledge, attitude, and self-management practices with the HbA1c level among people with diabetes, as undertaken in this study, is expected to set precedent for the development of an innovative intervention model which will help negate these challenges.
In an exhaustive literature search, we could not find any community-based studies evaluating the comprehensive relationship of knowledge, attitude, and self-management practices with HbA1c levels among people with T2DM. Most studies have examined bivariate relationships between knowledge, attitude, self-management practice, and HbA1c [7-9,13-17]. However, examining all the relationships comprehensively in one model will be beneficial in deepening the understanding of factors associated with the glycaemic control. Such a model predicts the paths between the key variables, which also examine the paths suggested by previous research on bivariate relationships. By using a structural equation modelling approach, we can achieve simultaneous examination of all these paths.
In the present community-based study, we aimed to address the gap in research on the inter-relationship between the key variables of knowledge, attitude, self-management practices, and HbA1c levels. To begin with, we designed a hypothetical model [Table/Fig-1] and conducted a cross-sectional study to gather baseline data. Based on the findings (presented in this paper) and literature review, we drafted an initial model. After the structural modelling, path analysis, and other modifications, the final structural model was developed. Currently, we are testing the effectiveness of the final model in people with T2DM, along with considering the influence of certain demographic variables.
Materials and Methods
After obtaining an institutional ethical committee approval, a cross-sectional study was conducted amongst people with T2DM in Udupi taluk, Karnataka, India. This study protocol is registered with the Clinical Trials Registry of India (bearing the registration number: CTRI/2017/02/007945). For recruitment of participants, a comprehensive registry of 12,478 people with diabetes was developed. A sample size of 600 was determined for the study. Using simple random sampling technique, we selected and contacted 600 people from the diabetes registry. Out of these, 482 responded to the researcher. A final sample size of the study was 432, as these patients fulfilled the inclusion criteria (people with T2DM, age between 30 to 65 years, people who are able to understand Kannada language). Other participants were excluded from the study as per the exclusion criteria (people not on medication, people with Type1DM, those who are critically ill, inability and refusal to sign the informed consent or comply with protocol, serious psychiatric illness, self-reported alcoholic or illicit drug use). In addition, 11 participants were excluded as their blood samples coagulated during transport from community to the central biochemistry laboratory.
Instruments
The data collection instruments included a demographic proforma, three questionnaires (measuring diabetes knowledge, attitude to living with diabetes, and diabetes self-management) and HbA1c test. Many knowledge, attitude and self-management practice questionnaires have been developed worldwide for assessing knowledge about T2DM and its management [18-25]. We modified existing tools for contextualisation and validated them for our use. The questionnaires used are all open-access, the authors were contacted before use, and they have been duly cited.
The demographic proforma included age, gender, duration of diabetes (time elapsed since diagnosis), previous hospitalisation, education, and income.
Diabetes Knowledge Questionnaire (DKQ): Developed by Eigenmann CA et al., [22], this represents questions on ideal range of blood glucose level and HbA1c, nature of diabetes, dietary management, physical activities, complications, management of diabetes when person is ill, frequency of medical check-up, and National Program for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke.
Diabetes Integration Scale – 19 (ATT-19): This encompassed six key factors linked to the management of diabetes including diabetes stress, responsiveness to treatment, trust on treatment, personal effectiveness, perception about health and social acceptance [26].
Diabetes Self-Management Questionnaire (DSMQ): This allowed the summation of four “subscale” score as well as estimation of four subscale scores. Contents of the subscales are labelled “Glucose Management,” “Dietary Control” “Physical Activity,” and “Health-Care Use” and “overall” rating [27].
HbA1c Testing: Primarily used for monitoring diabetes control, this test is also used to diagnose the T2DM [3] and hence was used. The National Glyco-haemoglobin Standardization Program (NGSP) approved HbA1c test method was followed to assess the glycaemic control of the participants inthis study. The blood sample collected in the field was tested, subsequently, in the biochemistry laboratory of a medical college that is NABH (National Accreditation Board for Hospitals and Healthcare Providers) accredited.
Validation and Reliability Testing of Questionnaires
Vigorous standard procedures were followed to culturally contextualise and adapt the questionnaires for this study. A professional translator was employed for the translation of these questionnaires into Kannada, the local language. A team of experts validated the translated questionnaire; the experts included a physician, a community medicine specialist, a private medical practitioner, a government medical officer, a Taluk Health Officer, a physiotherapist, a statistician, a dietician, a medical-surgical nursing specialist, a mental-health nursing specialist and a language expert. Once scrutinised, comparison of Kannada questionnaires with the original was made, and they were finalised. A professional translated the finalised tools back into English, and these back-translated versions were compared with the original English tools, as well. Two senior medical practitioners assessed the English version of the questionnaires, for good face and content validity.
For comprehensive evaluation of the reliability of the tool and its cross-cultural validation, the instruments were pilot tested. These questionnaires were administered to 30 people with T2DM at the Diabetic Foot Clinic of Kasturba Hospital, Manipal, Karnataka, India. After test and re-test, the items in these tools were found to be internally consistent, and strength of the agreement was substantial.
Cronbach’s alpha for testing the internal consistency: DKQ (0.774: acceptable), ATT 19 (0.931: excellent) and DSMQ (0.909: excellent).
Intra-Class Correlation Coefficient for testing for the test and retest: DKQ (0.751: acceptable), ATT 19 (0.89: good) and DSMQ (0.92: excellent).
Data Collection
The researcher personally contacted the participants and scheduled an interview based on participants’ availability and convenience. The interviews were conducted at patients’ homes, wherein first, their informed consent was obtained, and then the interview was recorded, along with blood sample collection. Demographic details were recorded according to proforma, and then the DKQ, ATT 19 and DSMQ were administered. Also, 2 mL of participant’s blood was collected in an EDTA container, for HbA1c evaluation. The researcher spent around 35 minutes per participant for data collection. The participants did not receive any monetary incentives or reimbursements for participating in the study.
Statistical Analysis
Using SPSS version 16.0, the data set was prepared and analysed. Descriptive statistics were used to analyse the characteristics of the participants and compare the relationship between gender, education and previous hospitalisation. Correlations were tested to explore the strength of relationships between various variables (age, duration of diabetes since diagnosis) and knowledge, attitude, and self-management practices. Independent t-tests were used to analyse the strength of the relationship between gender and education with knowledge, attitude, and practices of self-management.
Structural Modelling
Parsimonious model is preferred in path analysis [28,29]. Therefore, the significant correlation of variables was taken into consideration when the initial path model was developed. AMOS version 25.0 software was used for path analysis in SEM. Several fit indices were considered to determine the goodness-of-fit of the path model. The statistics included chi-square (with the desired value of p >0.05), the Root Mean Square Error of Approximation (RMSEA) (with desired value of >0.05), the Comparative Fit Index (CFI) and Normed Fit Index (NFI) it ranges from 0 to 1, with desired values of greater than 0.95 indicate good fit [29]. After obtaining the final path model, the significance of the indirect effect of diabetes knowledge, attitude and self-management practices on HbA1c were examined through AMOS. In order to determine the significance level (p-value) of the indirect effect, we performed bootstrapping in the modelling analysis [29].
Results
Characteristics of Participants
The descriptive analysis of all the study participants is presented in [Table/Fig-2]. In addition, the mean of HbA1c of study participants was 8.57% (SD=1.98%). Mean percent score of DKQ was 57.88 (SD=15.71), mean score of ATT-19 was 53.88 (SD=24.06) and mean score of DSMQ was 7.10 (SD=7.10).
Participants’ characteristics (n = 432).
| Participant characteristics | Mean (SD) | Number of Participants (Frequency %) |
|---|
| Age (years) | 55.03 (8.13) | |
| Gender • Females • Males | | 199 (46.1 %)233 (53.9 %) |
| Duration of diabetes since diagnosis (in years) | 7.19 (5.66) | |
| Education • Secondary or below • PUC or above | | 183 (42.4%)249 (57.6%) |
| Previous Hospitalisation • Yes • No | | 73 (16.9%)359 (83.1%) |
| Income (In Rupees per month) • less than 10,000 • 10000-20000 • 20000-30000 • 30000-40000 • 40000-50000 • above 50000 | | 307 (71.1%)82 (19.0%)24 (5.6%)9 (2.1%)5 (1.2%)5 (1.2%) |
The relationship between variables
A correlation matrix was created, which tested correlations between age and duration of diabetes with the knowledge, attitude, practices, and HbA1c levels [Table/Fig-3]. The correlation between attitude and self-management practices was very strongly positive. Additionally, there was a very strong negative correlation of HbA1c levels with attitude and self-management practices, individually, at 99% confidence interval. This implies that improved attitude and greater adherence to self management practices translate to lower HbA1c level.
Correlation of study variables (n = 432).
| Variable | 1 | 2 | 3 | 4 | 5 | 6 |
|---|
| 1. Age | 1 | 0.386* | 0.018 | 0.088 | 0.128** | -0.086 |
| 2. Duration of diabetes since diagnosis | | 1 | 0.022 | -0.091 | -0.069 | 0.080 |
| 3. Knowledge of Diabetes | | | 1 | 0.278** | 0.248** | -0.244** |
| 4. Attitude | | | | 1 | 0.921** | -0.891** |
| 5. Diabetes Self-Management Practice | | | | | 1 | -0.899** |
| 6. HbA1c | | | | | | 1 |
*p<0.05
**p<0.01
Structural Model
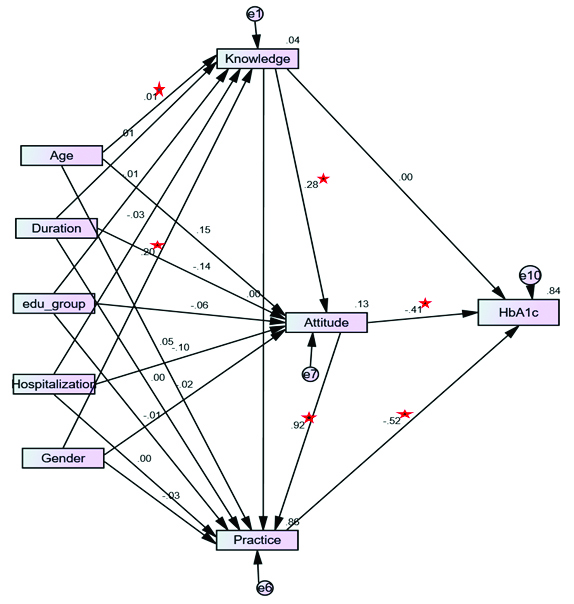
The hypothetical model based on the empirical findings is illustrated in [Table/Fig-1]. Based on the literature review, and results from the correlation and comparative analysis in this study, an initial hypothetical model was developed [Table/Fig-4]. This initially hypothesized model did not result in a good fit to data (χ2 (15) =132.455, p <0.001, RMSEA= 0.130, CFI= 0.939, NFI= 0.932). An evaluation of each of the 15 path relationships in the initially hypothesized model, showed that some paths were not significant, and three variables (duration of diabetes, previous hospitalisation and education level) contributed to a poor fit of the model.
Initialstructural model of age, duration of diabetes, education level, hospitalization, gender, knowledge, attitudes, self-management practice and HbA1c. Path loadings are standardised path coefficient.
*p-value < 0.05.
Based on these initial assessments, some modifications were made. Path relationships that were not significant were removed, variables that contributed to poor fit of the model were omitted. Non-significant pathways linking knowledge and self-management practice and HbA1c were removed. The model was retested, and any variable that did not contribute as a significant predictor was also removed from the initial model. The fit indices of the final model [Table/Fig-5] resulted in good fit (χ2 (5) =5.849, p=0.321, RMSEA= 0.019, CFI= 1, NFI=0.997). The regression coefficients between the variables improved.
Final Structural model of age, gender, knowledge, attitude, self-management practice, and HbA1c. Path loadings are standardised path coefficient. *p-value < 0.05.
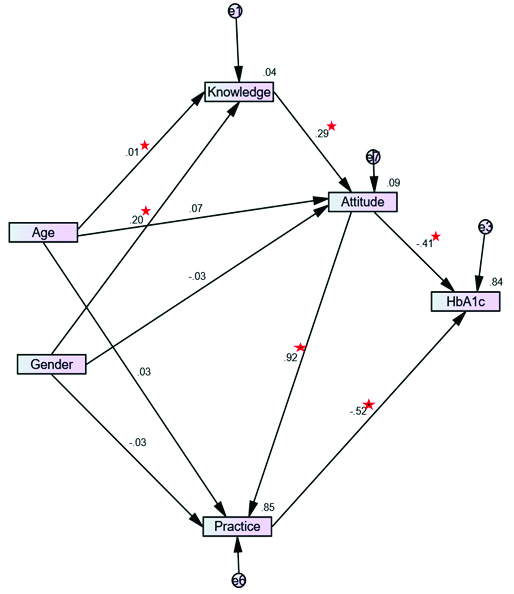
In the final model, better knowledge enhanced positive attitude there by improving HbA1c level. While there was no direct effect of knowledge on HbA1c, positive attitude contributed indirectly to better HbA1c levels through enhanced self-management practices. Age and gender were, also found to have a direct influence on diabetes knowledge.
Discussion
T2DM, being a chronic lifestyle condition with no day-to-day symptoms, presents some unique challenges in its management. People with T2DM need to stay motivated to maintain a healthy lifestyle and medication compliance. While there is an information explosion, along with ease of access due to the advent of the Internet over the last 20 years, it also offers some unique challenges. Social media affects their knowledge about diseases, influences their attitude and practices towards their management. In the middle of this “noise,” it is a challenge for clinicians to channel critically useful health information to patients. Therefore, patients’ existing knowledge and its effects on attitude, self-management plays a pivotal for any interventions.
The present study provides valuable insights into this with the use of path analysis (an extension of multiple regressions) for testing the hypothesis in data related to diabetes knowledge, CS, the practice of self-management, and HbA1c levels among people with T2DM. Path analysis is different from other traditional regression analysis. Path analysis is the family of Structured Equation. This model allowed the probe of a network, those are relationships between levels of diabetes knowledge, attitude, self-management, HbA1c and other variables such as age, gender, duration of diabetes since diagnosis, hospitalisation and education level and among people with T2DM in one single model.
We identified a significant relationship between knowledge on diabetes and attitude on diabetes management, attitude on diabetes management and practice of diabetes self-management, attitude and HbA1c, diabetes self-management and HbA1c.
In the present study, diabetes knowledge has a positive linear relationship with attitude, which is in line with other existing reports [7,30]. This finding will benefit health care providers who are involved in imparting education on diabetes self-management for people with diabetes [3,31]. We also found that diabetes self-management education helped in improving HbA1c levels at immediate follow-up. However, the same was not evident one to three months post conclusion of intervention [32], indicating the importance of regular support in glycaemic control among people with T2DM.
There was no significant association found between the knowledge on diabetes and diabetes self-management practice, as well as knowledge and HbA1c in the present study. Contrary to our findings, knowledge was established as a direct predictor for diabetes self-management and glycaemic control [7,8,28,33]. Though there was no significant relationship amongst knowledge and diabetes self-management, between knowledge and HbA1c in this study, we found that lack of knowledge and understanding of the plan of care adversely affects diabetes self-management, that could sway glycaemic control [34].
The present study also demonstrated that positive attitude among participants led to better diabetes self-management practices as well as resulting in effective glycaemic control. Earlier reports suggest that positive attitude is a predictor of diabetes self-management and glycaemic control [7,28]. Thus, it was essential to create a positive attitude about the six key factors linked to management of diabetes (including stress, response to treatment, trust on treatment, personal effectiveness, perception about health and social acceptance) [26], which is reported to help improve compliance in relation to dietary control [28], more regular physical activity, health care use, overall diabetes self-management practice and glycaemic control.
Further, we also noted an inverse correlation between diabetes self-management practice and HbA1c levels, indicating that regularity in glucose management, dietary control, and physical activity improves the overall self-management of people with T2DM. Earlier reports from a qualitative study carried out in Mexico also concluded that regular concurrence to naturally occurring lifestyle and self-care practices resulted in effective glycaemic control [10]. Another recent study found people with T2DM with better glycaemic control had better knowledge scores, attitude scores and practice scores [7].
Limitation
The participants for this study were recruited from the People with Diabetes registry (developed under World Diabetes Foundation 15:941 project), which is not an extensive registry. Except HbA1c levels, all other parameters were self-reported by participants during the interview. Thus, conclusions need to be drawn carefully from this study, and they will be restricted to a population defined by these characteristics.
Conclusion
This study concludes that attitude and diabetes self-management practices are reliable predictors of HbA1c values. Diabetes knowledge plays a pivotal role in developing positive attitude in diabetes management, which consequently improves glycaemic control. Attitude and diabetes self-management practice are an amalgamation of different factors such as diabetes stress, responsiveness to treatment, trust on treatment, personal effectiveness, perception about health, social acceptance and glucose management, dietary control, physical activity, health care use, and overall self-care management. Hence, Diabetes Self-Diabetes Self-Management Education (DSME) should be individually tailored and person-centred which aims to achieve a broader humanistic and societal perspective on the needs of people with diabetes. Consequently, DSME is likely to be more effective and evolve into a sustainable model in the community. This, in turn, might foster a positive attitude and help ease the practice of self-management in diabetes thereby leading to better glycaemic control.