Cardiovascular Diseases (CVDs) are significantly associated with morbidity and mortality in diabetic patients [1,2]. HbA1c is a time-integrated biomarker which reflects the glycaemic control over the preceding 2-3 months [3], and it has been considered as an important tool in diagnosis and management of diabetes [4,5]. Increased HbA1c levels in blood probably indicate long-term insulin resistance and co-existed consequences such as hyperglycaemia, dyslipidaemia, and system inflammatory response [6].
Diabetes mellitus is majorly associated with the macrovascular diseases like CVD and microvascular diseases like diabetic retinopathy, diabetic nephropathy, and diabetic neuropathy [7]. Association of HbA1c is much stronger with the risks of Atherosclerotic CVD (ASCVD) when compared to fasting plasma glucose [8]. On the other hand, HbA1c shows unsatisfactory correlation with fasting blood sugar and in patients with renal injury and anaemia [9].
The current study was designed to determine the association between glycosylated haemoglobin and incidence of CAD in non-diabetic and diabetic populations. The clinical implication of this study will add some idea regarding whether HbA1c might be used to predict the CAD risk in the non-diabetic patients.
Materials and Methods
Study Population
This study was a prospective observational study conducted from January 2016-December 2016. A total of 144 subjects with stable angina and/or positive stress test (Treadmill Stress Test) for coronary ischaemia and undergoing CAG at Kasturba Medical College and Hospital, Manipal Academy of Higher Education, Manipal, Karnataka, India, were enrolled. The patients belonged to the age group of 25-80 years.
The patients with the previous history of CAD and heart failure were excluded. The patients with ongoing non-cardiac comorbidities like infectious diseases, chronic inflammatory disorders and viral illness (retroviral, hepatitis B and C) and Chronic Kidney Disease (CKD) were not included.
Patients were classified into three groups according to their glycaemic status [1]:
Normal group (HbA1c: <5.6);
Pre diabetic group (HbA1c: 5.7-6.4);
Diabetic group (HbA1c: >6.4).
Demographic and clinical data were collected. Laboratory findings and the angiographic report have been noted. The Institutional Ethical Committee approved this study and the informed consent was obtained from all the participants.
Diagnostic Criteria
Routine clinical and physical examinations were performed. Fasting blood samples (12 hours fasting) were collected to check the plasma glucose and glycated haemoglobin (HbA1c). Hypertension is defined as systolic blood pressure ≥140 mmHg and diastolic ≥90 mmHg, or if the patient is currently receiving any antihypertensive medications [10].
CAD was defined as the presence of significant obstructive stenosis (at least 50% of the vessel lumen diameters) in any of the main coronary arteries, confirmed by coronary angiography. The severity of CAD was classified into normal (absent or minimal atherosclerotic involvement), Single Vessel Disease (SVD), and Two-Vessel Disease (DVD), Triple-Vessel Disease (TVD).
Biochemical Assessment
Blood sample of the patient was collected at baseline admission (before undergoing coronary angiography). Plasma blood glucose was measured by hexokinase method and serum creatinine by an enzymatic method using autoanalyser (Roche Diagnostics, Basel, Switzerland). HbA1c levels were measured using the Automated HPLC Analyser (Bio-Rad D-10) and hsCRP was measured by using turbidimetric assay.
Statistical Analysis
SPSS software version 20.0 (SPSS, Inc., Chicago, Illinois) was used to analyse the results. One-way ANOVA test analysed baseline characteristics of the study population. The association between HbA1c level and the risk of CADs was calculated by univariate and multivariate regression analysis. A p-value less than 0.05 considered to be significant.
Results
A total of 144 patients were included in this study. [Table/Fig-1] shows the baseline demographic data, laboratory and clinical findings. The mean age of study population was 56.6±9.5 years, and 101 (70.13%) were male. No significant difference of Body Mass Index (BMI), Waist Circumference (WC), Waist Hip Ratio (WHR) Creatinine level and also in serum hsCRP level were found between these three groups. Fasting Plasma Glucose (FPG) were significantly higher in the diabetic group compared to normal group.
General characteristics of study population.
| Characteristics | Normal(n=53)Mean±SD | Pre diabetic(n=62)Mean±SD | Diabetic(n=29)Mean±SD | p-value |
|---|
| Age | 53.8±9.6 | 58.18±8.92 | 58.48±9.87 | 0.027 |
| BMI | 23.88±3.54 | 24.42±4.30 | 24.90±3.79 | 0.51 |
| WC (cm) | 85.57±8.19 | 87.40±9.44 | 87.60±7.60 | 0.44 |
| HC (cm) | 89.19±8.90 | 91.15±11.08 | 90.8±8.74 | 0.55 |
| WHR | 0.95±0.32 | 0.95±0.034 | 0.96±0.23 | 0.89 |
| HbA1C (%) | 5.46±0.23 | 6.08±0.18 | 7.47±0.84 | <0.001 |
| FPG (mg/dL) | 96.55±13.70 | 103.68±20.04 | 113.7±31.72 | 0.002 |
| SBP (mmHg) | 134.75±14.72 | 133.03±14.68 | 136.09±14.87 | 0.53 |
| DBP (mmHg) | 82.34±8.24 | 80.35±7.29 | 81.66±7.69 | 0.38 |
| CREA (mg/dL) | 0.96±0.25 | 0.96±0.20 | 0.88±0.17 | 0.21 |
| Hb (gm/dL) | 13.55±1.68 | 13.47±1.55 | 13.61±1.64 | 0.321 |
| hsCRP | 5.26±5.46 | 5.7±5.1 | 6.4±7.9 | 0.67 |
One-way Anova test was done; Data are presented as Mean±standard deviation; BMI: Body mass index; WC: Waist circumference; HC: Hip circumference; WHR: Waisthip ratio; HbA1c: HemoglobinA1c SBP: Systolic blood pressure; DBP: Diastolic blood pressure; CREA: Creatinine; Hb: Haemoglobin; hsCRP: high sensitive CRP
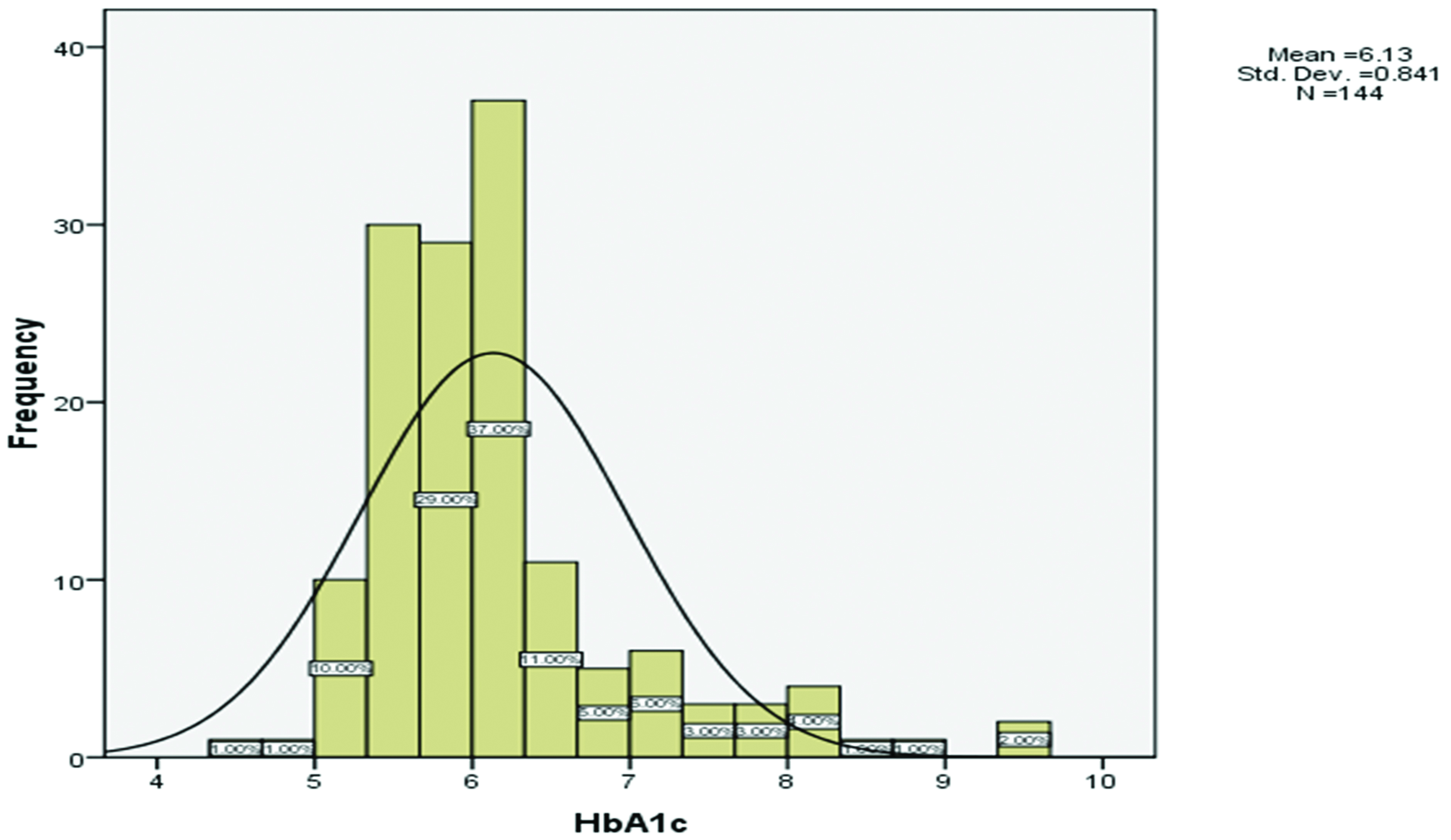
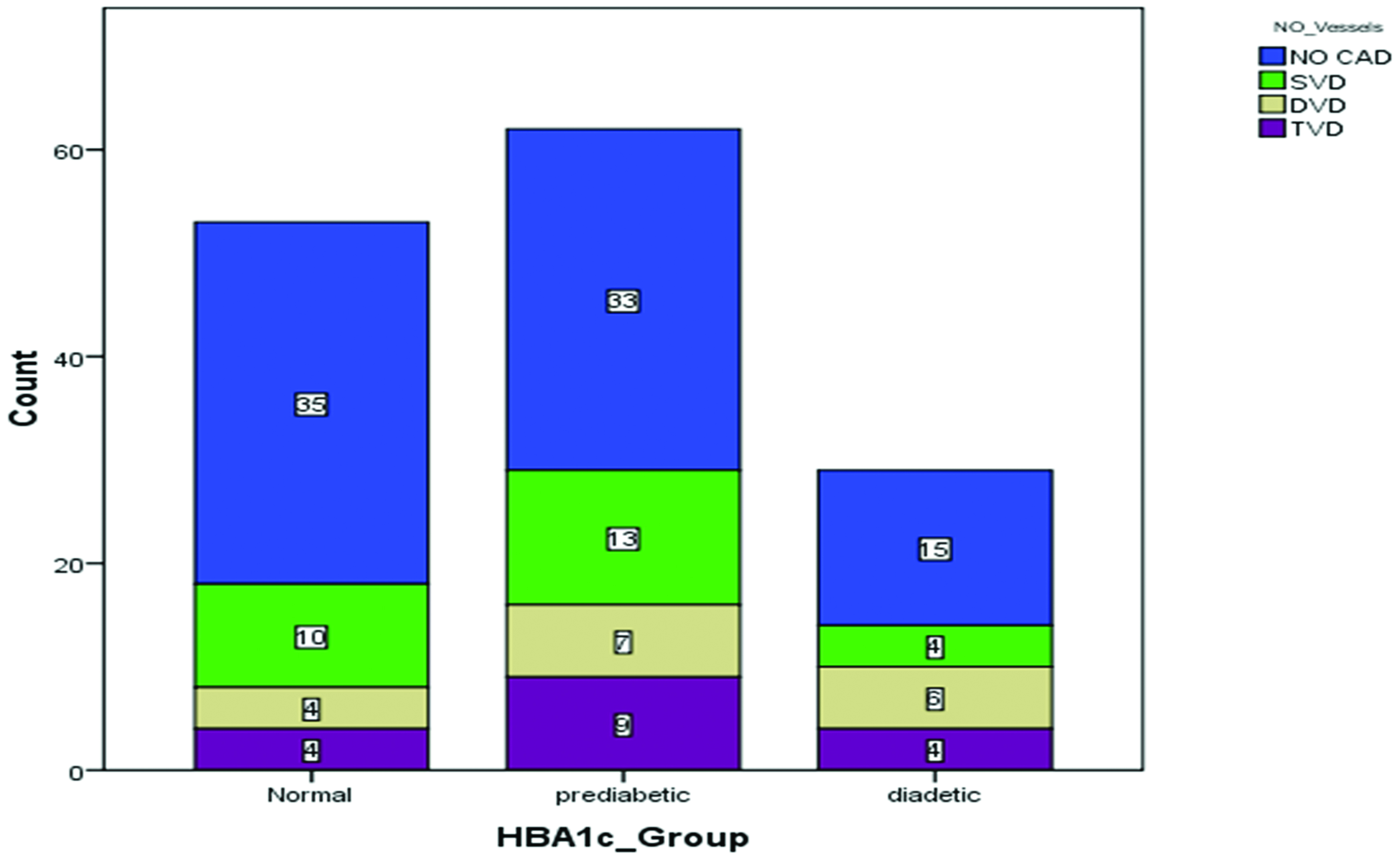
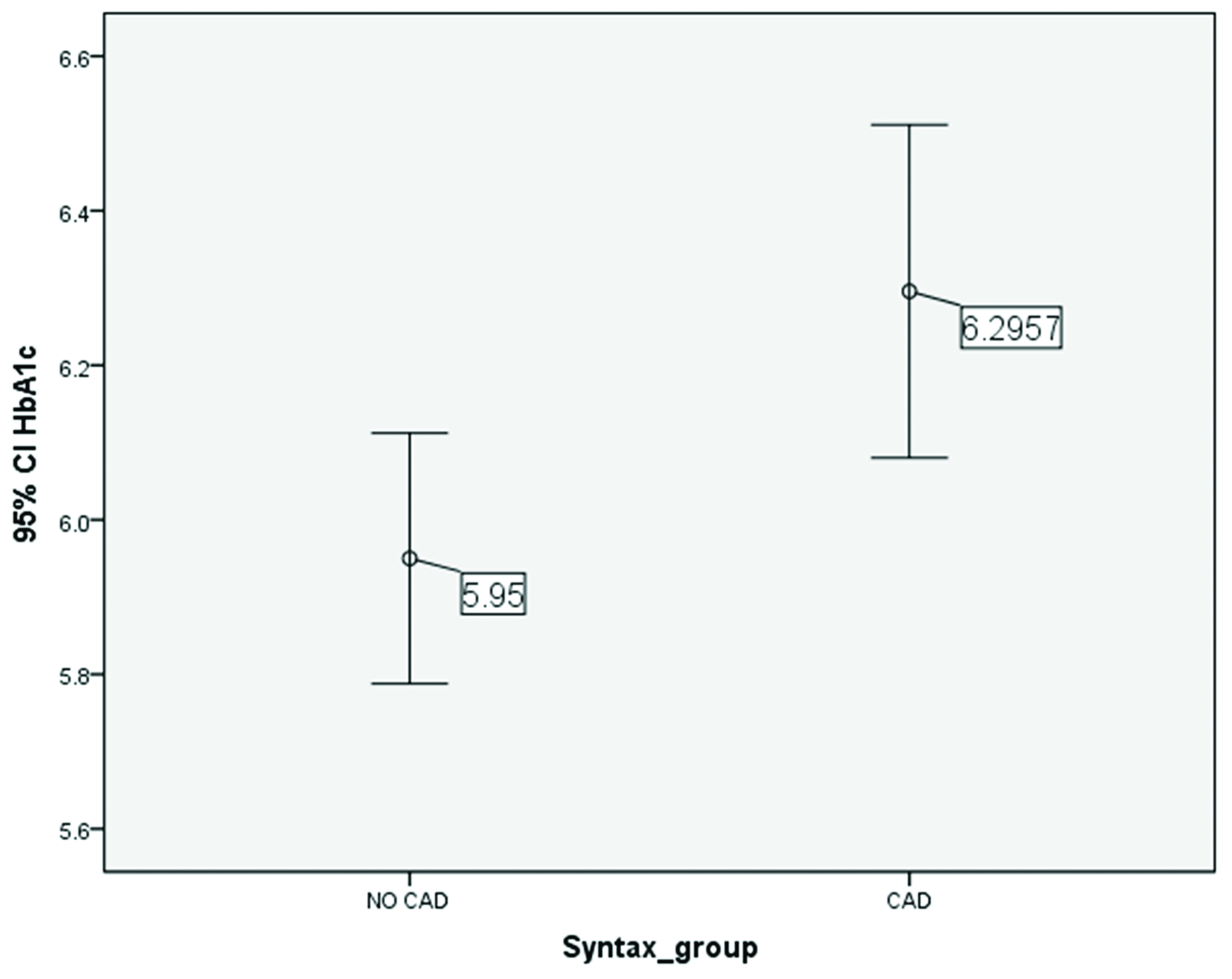
The distribution of HbA1c level in the study population is described in [Table/Fig-2], mean HbA1c level in study population was 6.13±0.84. It was observed that subjects with elevated HbA1c level were more than 50 years of age and has elevated BMI. The patients who are pre diabetic have 1.77 times more odds of having CAD than the patients who are normal, OR (95%, CI)=1.77 (0.84, 3.73), p=0.13; [Table/Fig-3]. The patients who have diabetes have 3.13 times more odds of having CAD than the patients who are normal OR (95%,CI)=3.13 (1.20, 8.16), p=0.02 [Table/Fig-4]. There was an association between HbA1c and severity of CAD which was calculated by pearson correlation analysis with r=0.20 and p-value=0.013 [Table/Fig-5].
Distribution of baseline serum haemoglobinA1c level.
Predictive value of serum HbA1c levels for coronary artery disease (CAD).
| Groups | CAD | OR (95%CI) | p-value |
|---|
| Yes (n%) | No (n%) |
|---|
| Normal | 31 (46.3) | 22 (28.9) | 1 | - |
| Pre diabetic | 27 (40.3) | 34 (44.7) | 1.77 (0.84,3.73) | 0.13 |
| Diabetic | 9 (13.4) | 20 (26.3) | 3.13 (1.20,8.16) | 0.02 |
Association of extent of coronary artery disease (CAD) in three groups according to serum HbA1c level.
Association between HbA1c level and severity of coronary artery disease.
Comparison of HbA1c levels among CAD and No CAD goups. Pearson correlation analysis was done, p-value <0.05 considered to be significant
Discussion
In the present study, the HbA1c level was found to be associated with higher risk of incidence of CAD. The multivariate logistic regression analysis confirmed the relative risk of HbA1c and CAD. It is already demonstrated in some previous studies that diabetes is one of the significant risk factors for cardiovascular events and atherosclerosis. Zoungas S et al., stated that HbA1c levels were associated with the risk of macrovascular events [11,12].
The cardiologist’s role is still not settled in the case of management of patients with diabetes. Most of the patients are diagnosed to have diabetes after onset of CAD. Therefore, it is essential to understand about the disease progression and necessary interventions to improve outcomes [13].
In present study, we measured the severity of CAD by the involvement of the vessels and presence of thrombus whereas the other studies used Gensini [14] and SYNTAX scoring [15].
There are studies which suggested an association of HbA1c level and the presence of CAD in asymptomatic individuals with or without diabetes and also in non-diabetic individuals. Epidemiology of diabetes complication studied by Prince CT et al., suggested that HbA1c level differs significantly in CAD cases compared to non-CAD and can be an independent predictor of CAD [16,17]. Rogowski O et al., suggested in their study that Glycated Haemoglobin (GlyHb) should be perceived as a continuous variable without a normal cut-off point, as it may exhibit detrimental role in predicting CAD [18]. However, in this study, we have divided the whole study population into three groups according to HbA1c level, and all the patients are with stress test positive and or with stable angina and undergoing a CAG. We found that HbA1c could significantly confer to clinical discriminators for predicting the risk of the presence of CAD.
The hypothesis of current study referred to glucose metabolism and associated CVD risk. However, it’s connection with inflammation and atherosclerotic plaque formation is not hidden. In present study also group of patients with elevated HbA1c and the High sensitive CRP (hsCRP) levels are associated with higher cardiovascular risk profile when compared to the normal HbA1c level group.
Previous studies suggested that elevated plasma HbA1c might give a clear picture on the impact of hyperglycaemia on vasculature atherosclerosis disease. Studies on the risk factors burden of CAD, concluded that group of patients with normal FPG and elevated HbA1c level are associated with higher coronary and atherosclerotic burden in non-diabetic patients [19].
Ertan C et al., found that pre diabetic patients have a smaller coronary size and in both the gender, it showed diffused coronary narrowing [20].
Therefore in the day to day cardiology practice, early detection of diabetes (pre-diabetic condition) may provide more appropriate vision about coronary lesion and its treatment (percutaneous or surgical).
Limitation
The present study has some limitations as due to the prospective observational design, its results cannot be generalised to the whole population. Factors such as anaemia or haemoglobinopathies were excluded which may alter the HbA1c levels. Long-term follow-ups might be needed to reveal further information regarding HbA1c association with future risk of CAD.
Conclusion
The study concluded that there was a significant association between raised baseline HbA1c levels and occurrence of CAD in patients with positive cardiac stress test/stable angina. HbA1c is a simple and reliable measure to predict the severity of CAD.
One-way Anova test was done; Data are presented as Mean±standard deviation; BMI: Body mass index; WC: Waist circumference; HC: Hip circumference; WHR: Waisthip ratio; HbA1c: HemoglobinA1c SBP: Systolic blood pressure; DBP: Diastolic blood pressure; CREA: Creatinine; Hb: Haemoglobin; hsCRP: high sensitive CRP