Scrub typhus is an endemic rickettsial disease causing vasculitis involving the small vessels of the body. Haemophagocytic Lymphohistiocytosis (HLH) is a hyperinflammatory syndrome characterised by excessive unbalanced cytokine release. An 11-year-old child presented with high grade fever with chills and rigors with respiratory distress. Chest X-ray showed right-sided consolidation. Serological tests for H1N1, Immunoassay for HIV, Montoux test were negative, BACTEC was sterile and CBNAAT of gastric aspirate was normal. Anti Nuclear Antibody and Anti ds-DNA tests were also negative. Rickettsial serology was positive for Scrub typhus, by IgM ELISA. The bone marrow examination showed macrophages with phagocytosis of erythrocytes, lymphocytes and platelets. A diagnosis of HLH was given. Flow cytometry revealed CD4 expression by 42.6% of T-cells and CD8 expression by 99.4% of T-cells leading to a reversal of CD4/CD8 ratio of 1:2. The patient did not respond to treatment and died soon after.
Early diagnosis of scrub typhus and its complications is essential as prognosis of the patient depends on time to start of treatment.
Case Report
An 11-year-old girl presented to our tertiary care hospital with chief complaints of high grade fever with chills and rigors for the past 20 days. The child also had a complaint of reduced oral intake for the past 3 days. There was decreased consciousness and altered sensorium since the past two days.
There was no history of exposure to tuberculosis or family history of similar illness. Since the past 20 days she had received paracetamol, ceftriaxone and chloroquine at a secondary care centre. On examination, the child appeared sick, irritable, pale and had increased respiratory rate of 60 breaths per minute. Other signs were small petechiae on extensor aspect of both upper limbs, bluish discoloration of lips, nasal grunting, flaring and excessive sweating. The blood pressure was normal, pulse rate was on the upper side of normal (100 beats per minute). Spleen was mildly enlarged (14 cm on ultrasound) and liver was 2 cm below costal margin (18 cm liver span on ultrasound). No rashes were seen on the body. The child was pale, without icterus, with no significant lymphadenopathy. No signs and symptoms of meningial irritation were found.
On haemogram the child had pancytopenia (WBC- 1.88×109/L, Hb- 8.6 g/dL, platelet- 40×109/L). The coagulation profile was deranged with increased Prothrombin Time (PT) (T=16.6 s, C=13.5 s) and Activated Partial Thromboplastin Time (APTT) (T=28.2 s, C=37.7 s) and raised D-dimer levels (2-4 microgram/mL by semi-quantitative method, n=N<0.5 microgram/mL). The serum electrolytes and kidney function tests were normal, but the liver function tests showed elevated serum bilirubin levels 2.4 mg (Direct- 1.9 mg and Indirect- 0.5 mg) and increased transaminases (Aspartate serumtransaminase-450 IU/L, Alanine aminotransferase - 93 IU/L). The serum protein and albumin levels were reduced (5.9 gm/dL and 2.2 gm/dL respectively). Thus, a provisional diagnosis of fever with pancytopenia and acute respiratory distress syndrome was made.
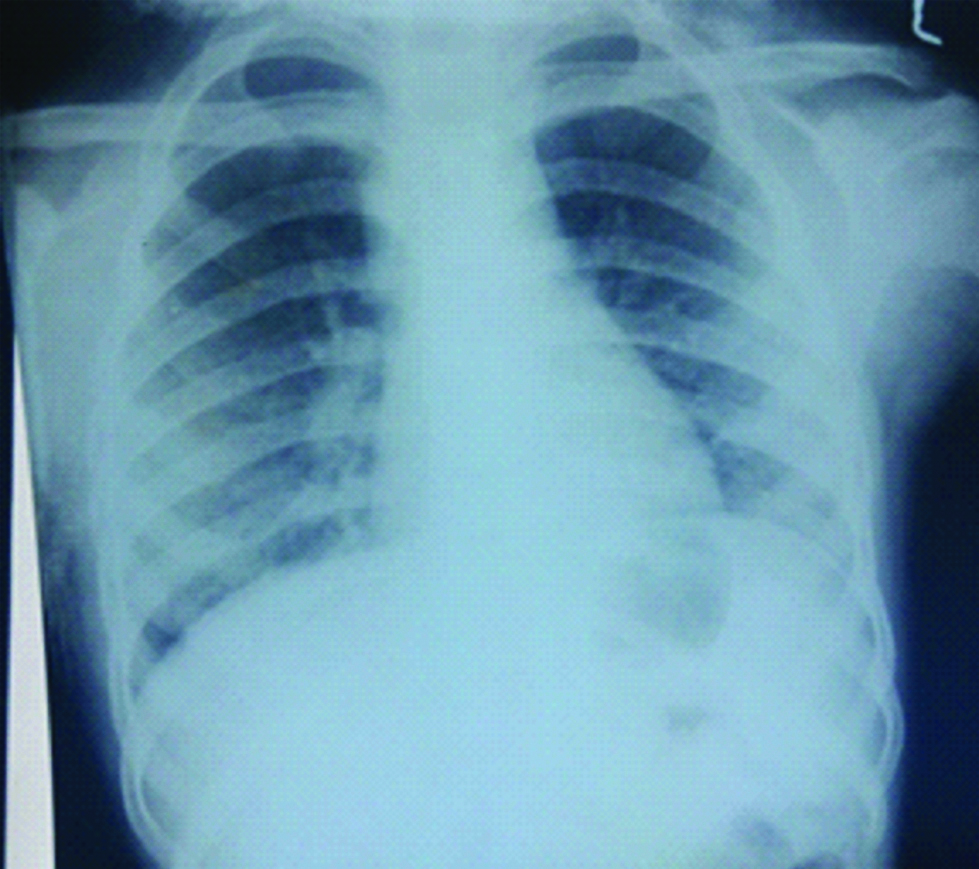
Chest X-ray showed consolidation on the right side with patchy opacities [Table/Fig-1,2]. On further investigation-Serological tests for H1N1, Dot immunoassay for HIV, Montoux test were negative, BACTEC was sterile and gastric aspirate for CBNAAT was negative. Rapid malarial antigen test and peripheral smear for malarial parasite was negative. Widal and viral markers–ELISA for HbsAg, HCVAg+Ab, HIV (Biorad 4th generation ELISA) were also negative. Anti Nuclear Antibody and Anti ds-DNA tests were also Negative.
Chest X-ray at the time of presentation showing right middle zone haziness.
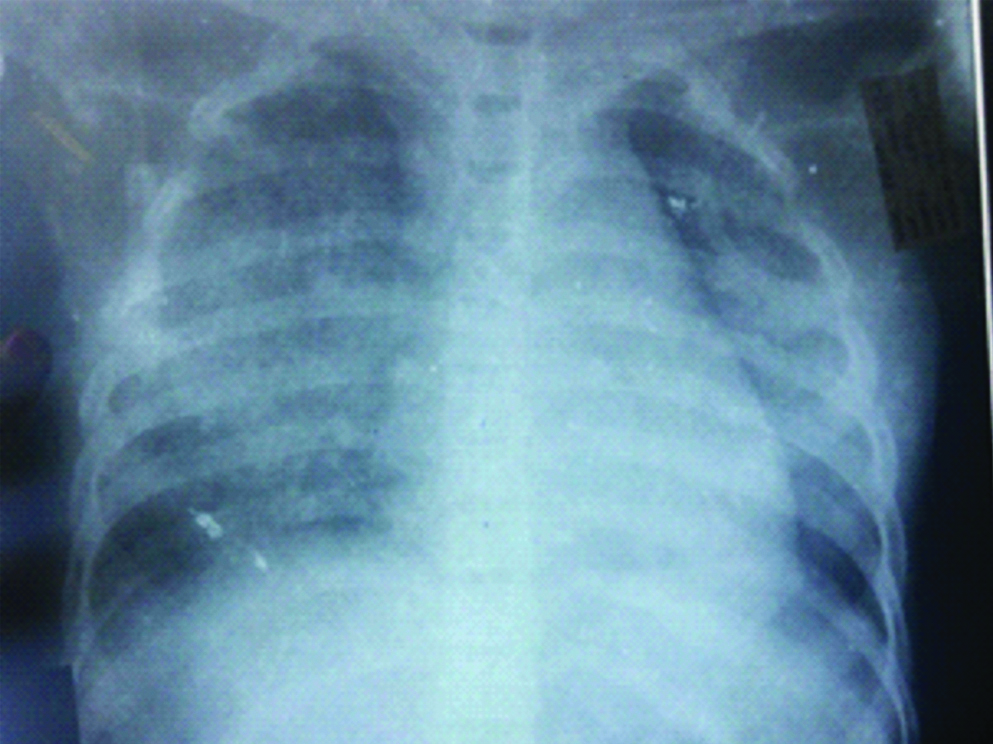
Chest X-ray just before ICU admission showing bilateral consolidation.
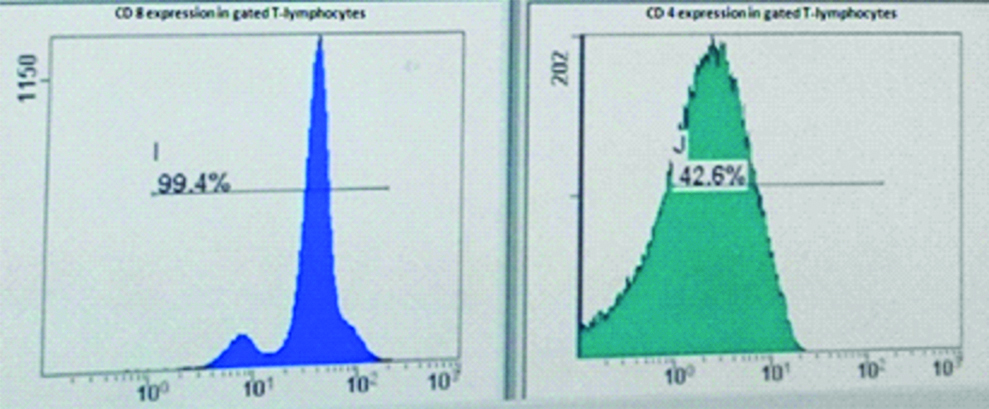
Since all the serological tests came out to be negative and patient had pancytopenia, flow cytometry of peripheral blood and Bone marrow examination were done to exclude aplastic anaemia or haematological malignancy. Flow cytometric examination of peripheral blood did not reveal any blasts or atypical cells. But a significant finding observed was CD4 expression by 42.6% of T-cells and CD8 expression by 99.4% of T-cells leading to a reversal of normal CD4/CD8 ratio [Table/Fig-3].
CD8 and CD4 expression on flow cytometry.
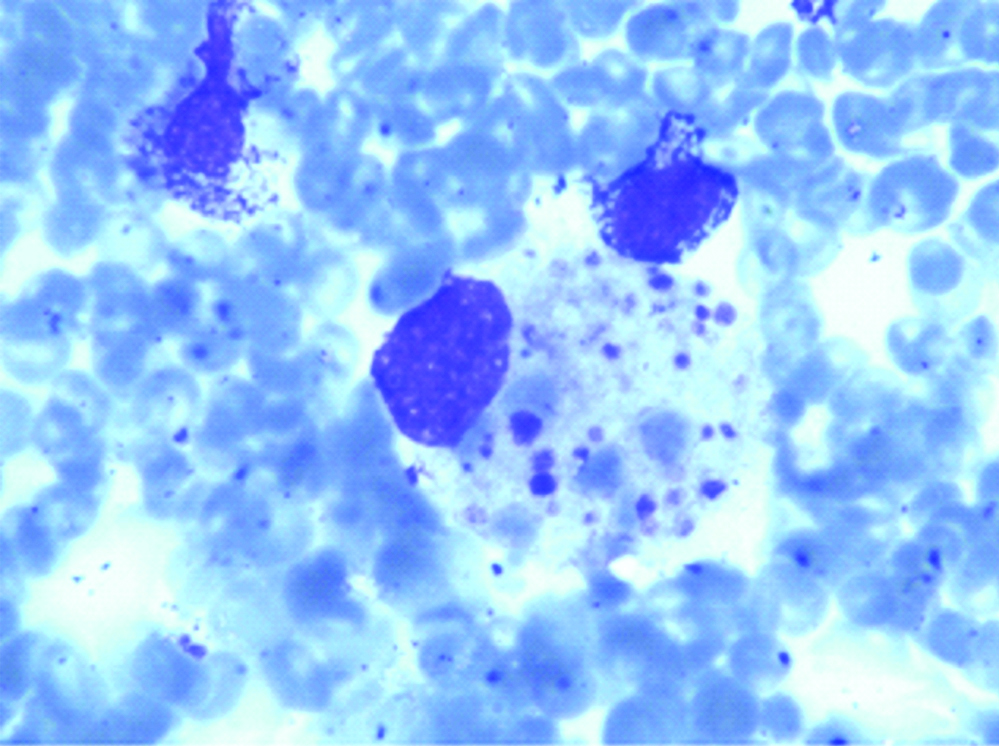
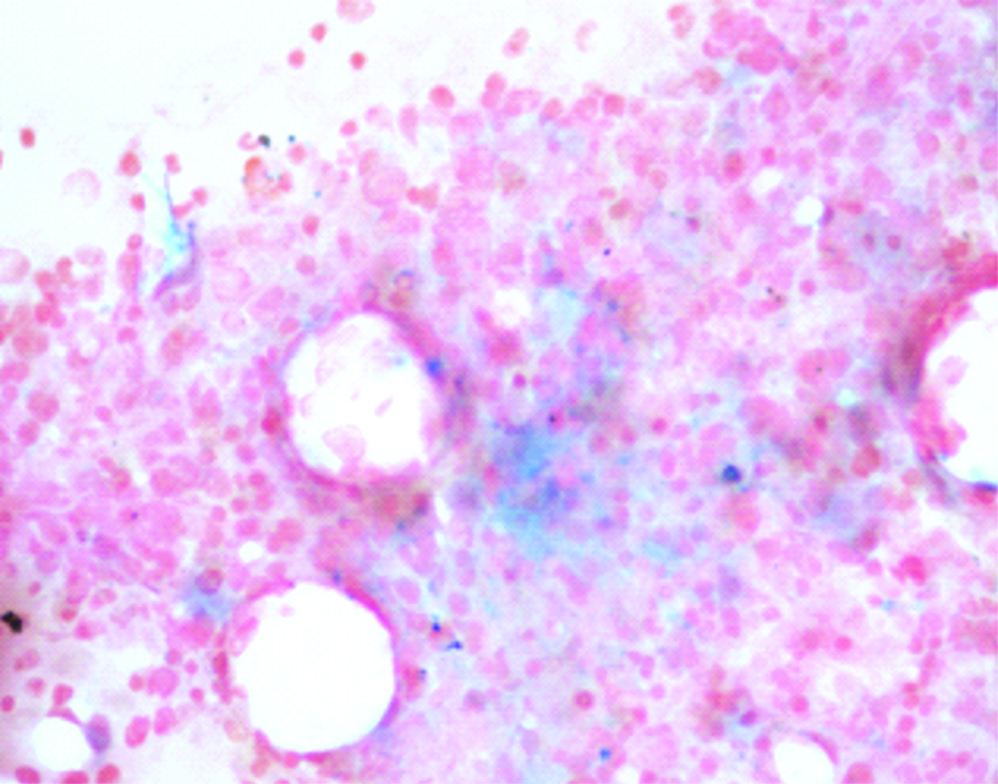
The bone marrow examination showed normoblasticerythroid hyperplasia along with increased number of macrophages. No parasite/blasts were seen in the smears examined. The macrophages showed phagocytosis of erythrocytes, lymphocytes and platelets [Table/Fig-4]. A suspicion of HLH was considered in the patient. Fibrinogen levels were reduced (87 mg/dL; N=212-433 mg/dL). The serum triglycerides were raised- 285 mg/dL (n=50-150 mg/dL). Serum ferritin levels were also raised (3570 microgram/l) [Table/Fig-5]. Hence, 6 out of 8 diagnostic criteria laid down by HLH society were positive. Thus a diagnosis of HLH was made [1].
Haemophagocytosis by macrophage in the bone marrow smear (Wright stain, x400).
Iron reserves in bone marrow slide (Pearl stain, x400).
Rickettsial serology test was done at the National institute of Communicable Diseases and was reported as positive for Scrub typhus by IgM ELISA. On meticulous examination no characteristic eschar of scrub typhus was found on the body.
Initially, patient was given injectable piperacillin/tazobactam and amikacin. Injectable Ceftazidime and Vancomycin along with artesunate were added when the child was not improving. Till all the investigation reports were received, empirical treatment for tuberculosis and oseltamivir was started. Patient was also given doxycycline and meropenem. There was no improvement in the patient’s health. Following diagnosis of HLH, respiratory distress worsened [Table/Fig-2]. The patient was shifted to ICU due to worsening respiratory distress, intercostal drain was added as patient developed pneumothorax. Steroids and treatment for HLH including etoposide and cyclosporine A was started.
The patient’s condition did not improve. She developed shock and despite full ionotropic support shock could not be controlled. Thereafter, she got cardiac arrest and ultimately died within 4 days of ICU admission.
Discussion
Haemophagocytic lymphohistiocytosis is a fatal, hyperinflammatory syndrome that may complicate the clinical course of scrub typhus [2].
Scrub typhus is a mite-borne disease caused by Orientiatsutsugamushi. Humans are the accidental hosts which are infected while feeding by the chiggers. These mites proliferate at the site of bite leading to formation of the characteristic eschar [3]. The chigger exposure is believed to occur in children during outdoor activity.
Unless there is a high level of suspicion, diagnosis of scrub typhus can be missed as the clinical features are non-specific. Our patient had a progressive clinical course. Along with delay in recognition other factors might trigger an activation of the immune system. Since vasculitis is the main mechanism behind the pathogenesis, many organs might be involved. But once the cytokine storm associated with the immune response against O. tsutsugamushi is triggered, it can become a life threatening infection [4].
The diagnosis of scrub typhus in our case was made through IgM ELISA which is the mainstay in diagnosis. Although the gold standard for diagnosis is indirect immunoflorescence assay, other tests like Weil Felix and immunoperoxidase are also used [5]. Old age, alcoholism, diabetes mellitus, liver diseases, respiratory diseases and G6PD deficiency are associated with a more severe scrub typhus infection [6].
Haemophagocytic lymphohistiocytosis is characterised by excessive unbalanced cytokine release [6]. It can occur as both familial (primary) and acquired (secondary) disease [7].
The HLH society criteria for diagnosis of HLH were established in 2004 by Henter J et al., and include either molecular diagnosis of HLH or establishing five out of eight following criteria [1]:
1. Fever; 2. Splenomegaly; 3. Cytopenias affecting at least 2 lineages in peripheral blood-Hb <9 g/dL, ANC <1.0×109/L, Platelet <100x 109/L, 4. Fasting triglycerides ≥265 mg/dL and/or fibrinogen ≤1.5 g/L, 5. Documented haemophagocytosis in bone marrow, spleen or lymph nodes, 6. Low or absent Natural Killer (NK) cell activity, 7. Ferritin ≥500 microgram/L, 8. Soluble CD25 (i.e., soluble IL-2R) ≥2400 U/mL.
Scrub typhus complicated by HLH is a very rare phenomenon. There have been a few case reports from India demonstrating the association between the two [2,8,9]. Flow cytometric findings in relation to the same have rarely been discussed in literature. An occasional article describes the association of HLH and EBV with increased CD8+ T-cells as compared to CD4+ T-cells [10]. Altered CD4/CD8 ratio has been studied as a marker of active disease process in paediatric patients by Miettunen P [11]. CD4/CD8 ratio has been reported to be altered in cytomegalovirus infection, tuberculosis and ageing [12-14]. Similar findings are being observed in our case with the reversal in CD4/CD8 ratio-normal is 2:1 and thus, reversal being 1:2 in our patient. Hence, we suggest that if flow cytometry reveals CD4/CD8 ratio reversal, the patient is having an impaired immune system. Treatment upgradation and suspicion of HLH should be kept in mind.
WHO says ‘Scrub typhus is probably one of the most underdiagnosed and underreported febrile illnesses requiring hospitalisation’ [15].
Scrub typhus associated with HLH is associated with a complicated course [4]. For HLH the 2004 treatment protocol initiated at the second international meeting of Histiocyte society recommends 8 week induction therapy with corticosteroids, etoposide and cyclosporine A [1].
Instead, Rajagopala S et al., have given a protocol for rapid evaluation of HLH and initiation of therapy. They propose that HLH secondary to infections can recover with early antimicrobial therapy and steroids alone. But early diagnosis and start of treatment is very essential for the resolution. If it does not resolve IVIG may be initiated followed by HLH treatment protocol in such cases. Follow-up by ferritin or sCD25 is recommended [16].
Conclusion
Prompt diagnosis and treatment of Scrub typhus should be done at the beginning of observing the signs and symptoms. Any case of scrub typhus not responding to treatment and showing pancytopenia, deranged coagulation profile and liver function tests should be investigated for HLH and treatment should be started. HLH is a medical emergency in any age or clinical situation, because the presentation is not very specific, the diagnosis takes time, thus leading to the increase in patient’s morbidity. Whenever possible, mutation analysis for primary HLH should be done so as to diagnose familial HLH. Further studies on the flow cytometry are required to better understand the pathogenesis and exact mechanism of association between these two conditions.
[1]. Henter J, Horne A, Aricó M, Egeler R, Filipovich A, Imashuku S, HLH-2004: Diagnostic and therapeutic guidelines for haemophagocytic lymphohistiocytosisPediatric Blood & Cancer 2007 48(2):124-31.10.1002/pbc.2103916937360 [Google Scholar] [CrossRef] [PubMed]
[2]. Sankhyan N, Saptharishi L, Sasidaran K, Kanga A, Singhi S, Clinical profile of scrub typhus in children and its association with haemophagocytic lymphohistiocytosisIndian Pediatrics 2014 51(8):651-53.10.1007/s13312-014-0470-425129000 [Google Scholar] [CrossRef] [PubMed]
[3]. MohanKaushik R, Kaushik R, Bhargava A, Multiple Eschars in Scrub TyphusTropical Medicine and Health 2014 42(2):65-66.10.2149/tmh.2013-3325237282 [Google Scholar] [CrossRef] [PubMed]
[4]. Jin Y, Huang L, Fan H, Lu G, Xu Y, Wu Z, Scrub typhus associated with haemophagocytic lymphohistiocytosis: A report of six pediatric patientsExperimental and Therapeutic Medicine 2016 12(4):2729-34.10.3892/etm.2016.366827698778 [Google Scholar] [CrossRef] [PubMed]
[5]. Blacksell S, Bryant N, Paris D, Doust J, Sakoda Y, Day N, Scrub typhus serologic testing with the indirect Immunofluorescence Method as a Diagnostic Gold Standard: A Lack of Consensus Leads to a Lot of ConfusionClinical Infectious Diseases 2007 44(3):391-401.10.1086/51058517205447 [Google Scholar] [CrossRef] [PubMed]
[6]. Cascio A, Giordano S, Dones P, Venezia S, Iaria C, Ziino O, Haemophagocytic syndrome and rickettsial diseasesJournal of Medical Microbiology 2010 60(4):537-542.10.1099/jmm.0.025833-021163825 [Google Scholar] [CrossRef] [PubMed]
[7]. Rosado F, Kim A, Hemophagocytic lymphohistiocytosisAmerican Journal of Clinical Pathology 2013 139(6):713-27.10.1309/AJCP4ZDKJ4ICOUAT23690113 [Google Scholar] [CrossRef] [PubMed]
[8]. Basheer A, Padhi S, Boopathy V, Mallick S, Nair S, Varghese R, Hemophagocytic lymphohistiocytosis: an unusual complication in Orientiatsutsugamushi disease (scrub typhus)Mediterranean Journal of Hematology and Infectious Diseases 2014 7(1):201500810.4084/mjhid.2015.00825574367 [Google Scholar] [CrossRef] [PubMed]
[9]. Diwan AG, Shewale R, Iyer S, Nisal A, Agrawa P, Triple trouble--macrophage activation syndrome in a case of severe leptospirosis and scrub typhus co-infectionJ Assoc Physicians India 2014 62(1):58-61. [Google Scholar]
[10]. Yang C, Zhu X, Zhang T, Ye Q, EBV-HLH children with reductions in CD4+ T cells and excessive activation of CD8+ T cellsPediatric Research 2017 Jul 24 10.1038/pr.2017.17828738028 [Google Scholar] [CrossRef] [PubMed]
[11]. Miettunen P, Reversal of CD4: CD8 Ratio in Pediatric Patients with Macrophage Activation Syndrome/Reactive Hemophagocytic Lymphohistiocytosis (MAS/HLH): A Potential Marker for Active Disease ProcessClinical Immunology 2007 123:S97-98.10.1016/j.clim.2007.03.457 [Google Scholar] [CrossRef]
[12]. Hadrup SR, Strindhall J, Køllgaard T, Seremet T, Johansson B, Pawelec G, Longitudinal studies of clonally expanded CD8 T cells reveal a repertoire shrinkage predicting mortality and an increased number of dysfunctional cytomegalovirus-specific T cells in the very elderlyThe Journal of Immunology 2006 176(4):2645-53.10.4049/jimmunol.176.4.264516456027 [Google Scholar] [CrossRef] [PubMed]
[13]. Yongmei YI, Jie QI, Yaping DA, Fanwei ZE, Hao PE, Jun WA, The CD4+/CD8+ ratio in pulmonary tuberculosis: Systematic and meta-analysis articleIranian Journal of Public Health 2015 44(2):185 [Google Scholar]
[14]. Serrano-Villar S, Moreno S, Fuentes-Ferrer M, Sánchez-Marcos C, Avila M, Sainz T, The CD4: CD8 ratio is associated with markers of age-associated disease in virally suppressed HIV-infected patients with immunological recoveryHIV Medicine 2014 15(1):40-49.10.1111/hiv.1208124007533 [Google Scholar] [CrossRef] [PubMed]
[15]. World Health Organization. WHO recommended surveillance standards. 1999 [Google Scholar]
[16]. Rajagopala S, Singh N, Diagnosing and treating hemophagocytic lymphohistiocytosis in the tropics: systematic review from the Indian subcontinentActamedicaacademica 2012 41(2):161-74.10.5644/ama2006-124.4923331391 [Google Scholar] [CrossRef] [PubMed]