Surgery is the backbone for treatment of thyroid malignancy. Total thyroidectomy with or without neck dissection is standard of care. Thereafter adjuvant treatment, usually radioiodine, depends upon risk stratification of patient [1]. Common complications of total thyroidectomy are hypocalcaemia and voice change [2]. The present study aimed to know the incidence and risk factors of major complications like hypocalcaemia, voice change, nerve palsy following thyroid cancer surgery.
Materials and Methods
The present study was a prospective observational study carried out in tertiary cancer care centre. Total of 52 patients, fulfilling preoperative inclusion criteria were recruited from a period of October 2010 to June 2011, however, for data analysis only 50 patients were included. Two patients were excluded, as they had the intraoperative sacrifice of recurrent laryngeal nerve due to tumour encasement, as per exclusion criteria. All 50 patients underwent total thyroidectomy with or without neck dissection. Follow-up of these patients was for a period of one year after surgery.
Inclusion criteria were all patients between the ages of 18 and 65 years, willing to participate in the study; FNAC proved or suspected carcinoma thyroid (BATHESDA IV, V, VI); fit for total thyroidectomy with or without concomitant neck dissection.
Exclusion criteria were patients with history of prior thyroid or neck surgery, patients requiring unilateral lobectomy or completion or revision thyroidectomy; patients with known voice dysfunction preoperatively, or inability to give a voice recording such as hearing impairment, deafness or detected with an asymptomatic vocal cord palsy; with a known hypocalcaemic disorder; intraoperative involvement of laryngeal nerve by tumour.
All patients had a preoperative laryngoscopy to evaluate the vocal cords. All patients had undergone blood test to find preoperative serum albumin, urea, creatinine, magnesium and phosphate levels. Serum calcium levels were adjusted according to abnormal serum albumin level. Corrected values were used for data analysis. All patients underwent preoperative voice recording using the Praat Software version 5.3.23. (Software obtained by free online download) The mean pitch (F0), jitter, shimmer and Noise to Harmonic Ratio (NHR) were recorded. Praat pitch parameters were set at minimum 50 Hz and maximum 250 Hz. Window length was automatically determined by Praat [3]. The patient was comfortably seated on a chair and told to say the sounds //aa//, //ee//, //uu// for a total time of five seconds to record the voice with a microphone 5 cm apart from the lips. Mean Fundamental F0, jitter, shimmer, noise to harmonic ratio were analysed by Praat.
These patients underwent total thyroidectomy with or without neck dissection. An extracapsular dissection technique was followed in all cases. The recurrent laryngeal nerves were identified on both sides in the cases. The parathyroid glands were carefully preserved, and if devascularised, those were implanted into the sternocleidomastoid muscle. Selective neck dissection was performed in patients with clinically positive neck nodes. Central compartment was dissected if there were significant nodes as on preoperative imaging or intraoperative findings. Central compartment neck dissection was done in all cases of medullary carcinoma thyroid. Surgeons operating in these patients are the consultant in tertiary cancer care centre with minimum experience of 10 years in head and neck cancer surgeries including thyroid malignancy.
Serum calcium level of all patients was monitored at 6 hours, 24 hours, 48 hours after surgery and then once daily till discharge. Such a frequent calcium monitoring was done to plot calcium slope for the study. Otherwise, after thyroidectomy serum, calcium levels are measured once every day from postoperative day one, untill discharge. More frequent monitoring is considered only if the patient has hypocalcaemia. Patients were assessed for any sign or symptom of hypocalcaemia or nerve injury in form of voice change. Patients with hypocalcaemia were grouped as symptomatic or biochemical (asymptomatic) hypocalcaemia. Biochemical hypocalcaemia was defined as a corrected serum calcium level of less than 8 mg/dL with no sign or symptom suggestive of the hypocalcaemia [4]. Symptomatic patients were those patients who had signs of hypocalcaemia (including Chvostek’s sign, Trousseau’s sign or tetany) or complained of symptoms like peri-oral tingling sensation or numbness, paresthesia of the hand or feet.
At 6 hours postoperatively, patients with serum calcium less than 8 mg% received 10 mL of 10% (w/v) Calcium gluconate intravenously diluted in 100 mL of normal saline over 20 minutes.
On postoperative day one onwards, patients with serum calcium levels between 7-8 mg/dL were started on oral calcium carbonate at 2 gm per day in divided dosage. If calcium level was <7 mg/dL, oral calcitriol 0.25 micrograms to 1 mg/day was added to 2 gm of calcium carbonate. A 10 mL of 10% (w/v) calcium gluconate was given intravenously over 20 minutes diluted in 100 mL of normal saline if patients had carpopedal spasm or severe tingling/numbness of hand or feet. Dosages were repeated twice a day untill abatement of symptoms. Serum magnesium level was checked in patients with hypocalcaemia persisting after 48 hours. If serum magnesium was <1.2 mg/dL, parenteral magnesium 2 gm was given intravenously as a single dose infusion drip.
All patients were assessed at 10 days, six weeks, six months and 12 months after surgery. Serum calcium level was checked at all follow-up. Patients with hypocalcaemia were followed up at monthly intervals. These patients were on 2 gm of calcium supplementation every day in four divided dosages. Once their serum calcium level was normalised, the dose was tapered by 500 mg daily at every consecutive week and stopped. After that, these patient followed follow-up protocol as other normocalcaemic patients.
At six weeks follow-up, patients were evaluated for voice dysfunction symptoms including inability to raise the pitch, sing, loss of projection, voice fatigue. All patients underwent flexible laryngoscopy and voice analysis at six weeks. When abnormal findings were seen on laryngoscopy or if patients had voice dysfunction, they were referred for Laryngeal Electromyogram (LEMG).
At subsequent follow-up, laryngoscopy was repeated on all patients with previous abnormal finding to assess the status of the vocal cord palsy. These patient’s voice symptoms with regards to hoarseness, fatigue, loss of projection were also recorded. LEMG was planned on seven patients with voice dysfunction; however, four patients showed rapid improvement in symptoms and clinically did not warrant LEMG. Hence only three patients underwent procedure. Repeat LEMG assessment at one year was planned in patients with evidence of superior laryngeal nerve palsy, but none were eligible.
Statistical Analysis
The obtained data were analysed using the SPSS software version 17.0. All patients underwent preoperative voice recording using the Praat Software version 5.3.23. (Software obtained by free online download) The mean pitch (F0), jitter, shimmer and NHR were recorded. Praat pitch parameters were set at minimum 50 Hz and maximum 250 Hz. Window length was automatically determined by Praat.
Analytic methods included descriptive statistics, chi-square test, Student’s t-test to compare between two continuous variables, Correlation matrix and coefficient of correlation using Pearson’s method (p-value=level of significance, p>0.05=non-significant, p<0.05=significant, p<0.001=highly significant). Pattern of change was observed and compared to his/her own preoperative reading.
Results
The present study included a total of 50 patients for assessment of postoperative complications. Out of 50 patients, one was lost to follow up due to death, eight months after surgery. This patient died of myocardial infarction. Major complications studied were hypocalcaemia (symptomatic and/or biochemical), voice change (perceptual and/or acoustical).
In the study 68% of patients were female and 32% male, reflecting higher incidence of thyroid malignancy in females. In this study for 11 patients (22%), voice was important for their profession (teacher, singer, priest) [Table/Fig-1].
Showing demographic detail, procedure, postoperative symptoms, pathology report.
| Total number of patients | 50 |
| Male | 16 (32%) |
| Female | 34 (68%) |
| Age (Range) | 19 years to 65-year-old |
| Mean age | 42.14 years |
| Professional voice user | 11 (22%) |
| Total thyroidectomy (TT) only | 41 (82%) | Total- 50 patients |
| Total thyroidectomy with neck dissection | 9 (18%) |
| TT+ posterolateral neck dissection (PLND) only | 2 (4%) | Total 9 patients, who have undergone thyroidectomy with neck dissection. |
| TT+ central compartment neck dissection (CCND) only | 4 (8%) |
| TT+PLND+CCND | 3 (6%) |
| Voice change | 14 | |
| Fatigue | 11 | |
| Loss of projection | 4 | |
| Temporary unilateral vocal cord palsy | 1 (2%) | |
| Papillary carcinoma | 43 (86%) | Histopathology report of 50 patients. |
| No malignancy in final pathology | 6 (12%) |
| Medullary carcinoma | 1 (2%) |
Hypocalcaemia: The incidence of hypocalcaemia was 48% in this study at a cut-off of 8 mg/dL. The patients who were symptomatic (either symptoms or clinically elicited signs) accounted for 10%. Although, the incidence of hypocalcaemia was 48%, 42% of patients had temporary and only 6% had permanent hypocalcaemia.
In the study patients requiring calcium supplementation for more than six months were considered permanent hypocalcaemic [4, 5].
Age, gender and tumour size were not significantly associated with incidence of hypocalcaemia. Central compartment neck dissection was seen to be a significant factor for temporary hypocalcaemia (p=0.03). In the present study a total of seven patients had undergone CCND, of which six developed temporary hypocalcaemia.
Calcium trends and calcium slope: Much research has been done on the possibility of prediction of hypocalcaemia in patients undergoing thyroid surgery. Calcium slopes (day 0-day 1 calcium measurement) has been reported to be sensitive to predict hypocalcaemia [6].
In this study, the calcium slope (calcium at six hours-calcium at 24 hours) showed a statistically significant difference between hypocalcaemic and normocalcaemic groups.
On comparing the calcium trend, patients in the hypocalcaemic group had a lower measurement at six hours, 24 hours and at 48 hours. By 48 hours, this measurement was not reflective of hypocalcaemia as patients were on calcium supplements. The difference in calcium trend was statistically significant (p<0.05).
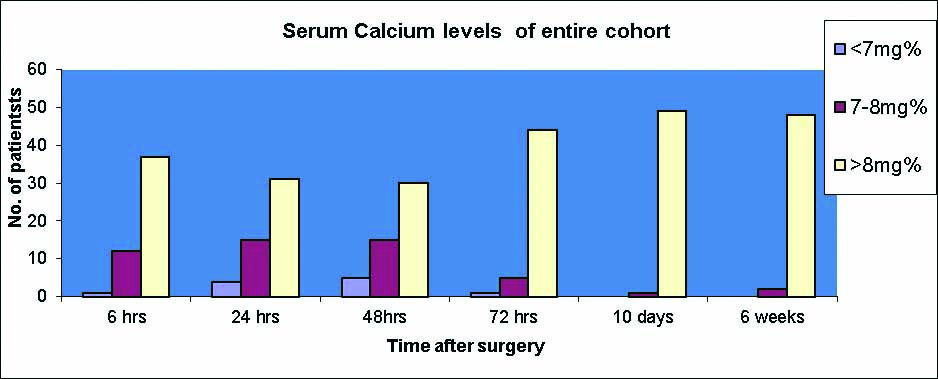
The calcium trend was useful in predicting which patients may require calcium supplementation albeit temporarily [Table/Fig-2].
Serum Calcium levels of entire cohort.
The patients, who had permanent hypocalcaemia also had immediate postoperative hypocalcaemia although the absolute measurements were not significantly different from the normocalcaemic group. For patients with permanent hypocalcaemia, calcium trend did not show a statistically significant difference (p=0.85). This is probably due to the very small number of permanent hypocalcaemia patients (n=3).
Neck dissection and hypocalcaemia: Central compartment neck dissection was seen to be a significant factor for temporary hypocalcaemia (p=0.03). In the study total seven patients had undergone CCND, of which six developed temporary hypocalcaemia. There was no significant association of neck dissection and permanent hypocalcaemia. In the study, three patients developed permanent hypocalcaemia but only one had undergone neck dissection, other two had not.
Voice dysfunction: Patients were evaluated at six weeks after surgery for voice dysfunction. This was not done earlier to exclude the postoperative transient changes caused by intubation trauma, immediate effects of surgery like inflammation, oedema etc. Patients were evaluated with perceptual voice dysfunction, laryngoscopy, voice analysis and LEMG. Videostroboscopy was not preferred as it was realistically difficult with need for specific instruments and extra costs.
Fourteen patients complained of perceptual voice dysfunction even after six weeks of surgery. Of these 14 patients, 11 also complained of fatigue. However, at the end of one year, all except one patient in the voice dysfunction group had normal voices.
Nerve palsy: In this study, the incidence of unilateral Recurrent Laryngeal Nerve (RLN) palsy was 10%, with 2% transient unilateral RLN palsy and 8% permanent unilateral RLN palsy. There was only one patient (2%) with transient external branch of superior laryngeal nerve palsy, which could not be confirmed on LEMG. The patient’s symptoms of inability to raise pitch and loss of singing voice, had resolved at 8-10 weeks and repeat laryngoscopy showed resolution of the previous changes seen. There was no significant association of age, gender, tumour size and neck dissection with the risk of nerve injury. Tumour size need not predispose to nerve injury as large tumours may be well encapsulated whereas small tumours located close to the tracheoesophageal groove predisposes to nerve injury during dissection.
Discussion
The aim of the study was to know the incidence of major complications like hypocalcaemia, voice change, nerve palsy following thyroid cancer surgery. Most of the studies in the literature on thyroidectomy complications include a heterogeneous mix of partial lobectomy, total lobectomy and revision surgery cases as the patient cohort. This leads to varied results in the incidence of complications, as they are less likely in partial thyroidectomy as compared to a revision of thyroid surgery where the incidence of complications is maximum. Most of the literature also includes benign and malignant conditions of the thyroid together, however again the incidence of complications in these two groups varies widely.
This study focuses only on patients with proven or suspicious thyroid cancer and hence has a more homogenous group with respect to risk factors.
The incidence of hypocalcaemia varies according to the cut-off value applied whether at 7.5 mg% or 8 mg%. Biochemical hypocalcaemia presents early, but this is largely transient. Symptomatic hypocalcaemia is seen in only a minority and does not manifest until after 24-48 hours after surgery. The calcium slope (the difference between serum calcium six hours after surgery and postoperative day 1) may help predict which patient may develop symptomatic hypocalcaemia [5-7]. In the present study, the calcium slope (calcium at 6 hours-calcium at 24 hours) showed a statistically significant difference between hypocalcaemic and normocalcaemic groups.
The temporary hypocalcaemia lasts up to six months. Patients who are dependent on calcium supplementation after six weeks may be permanently hypocalcaemic [4]. Thyroid cancer surgery for malignant cause is itself a significant risk factor for hypocalcaemia when compared to surgery for benign aetiologies. Age, sex, tumour size, concomitant neck dissection were examined as variables affecting hypocalcaemia. Age, gender and tumour size were not significantly associated with hypocalcaemia. Central compartment neck dissection was seen to be a significant risk factor for temporary hypocalcaemia [8]. Central compartment dissection increases the risk of injury to parathyroid by de-vascularising them or by direct injury [9,10].
Voice dysfunction after thyroid surgery is a common problem and occurs with and without nerve palsy as reported in previous studies [11].
Other than nerve injury there are various other reasons for voice dysfunction like damage to extralaryngeal muscles, an effect of postoperative healing and fibrosis, intubation injury [10-12]. Various authors have used different methods like stroboscopy and intra- and extralaryngeal electromyography, estimation of maximum phonation time and phonation frequency range, to identify the causes and possible ways to identify them [13-15], however, none of these methods are standardised and most need a voice pathologist or surgeons with considerable experience with voice disorders to identify and interpret them. The subjective perception of voice changes itself, varies widely. The average patient is not as bothered as the professional with the change in pitch in his/her voice. In this study, voice fatigue was common symptom in all patients with voice dysfunction. Inability to talk as long as earlier (preoperatively), need to rest their voices in between conversations, were the symptoms common to this group.
After total thyroidectomy, most of the voice changes are temporary provided intraoperative, there was no nerve damage. These changes may be limited to selected perceptual changes such as decrease in pitch and increase in breathiness or increased strain. Vocal fatigue was the most common symptom in patients with voice dysfunction. Subjective voice dysfunction is largely unnoticed by patients unless they are professional voice users or there is recurrent laryngeal nerve palsy.
Unilateral RLN palsy causes severe voice dysfunction and occasional aspiration symptoms. The symptoms rapidly improve in transient nerve palsy in 6-8 months. In permanent nerve palsy, it may take more than a year [16]. In the literature, the figures quoted for permanent RLN palsy varies from 0 to 14% with the highest quoted for malignancy of the thyroid or reoperations of the thyroid [17]. In the present study, the incidence of unilateral RLN palsy was 10%, with 2% transient unilateral RLN palsy and 8% permanent unilateral RLN palsy. There was no significant association of age, sex, tumour size and neck dissection with risk of nerve injury. Tumour size need not predispose to nerve injury as large tumours may be well encapsulated whereas small tumours located close to the tracheoesophageal groove predisposes to nerve injury during dissection.
Limitation
Most studies in the literature regarding complications of thyroidectomy include both benign and malignant cases. The present study includes all patients with proven or suspicious of malignancy, in an attempt to have a homogenous group with regard to aetiology. One of the important issues with the study is of a smaller sample size. A similar study with larger sample size may give the statistically stronger result.
Conclusion
Hypocalcaemia and voice change are troubling complications for both patient and surgeon. Risk, after surgery, is more in malignant and recurrent cases. In the present study, central compartment neck dissection was strongly associated with risk of hypocalcaemia. A similar study with a larger number may give us the idea about other factors like tumour size, location and their statistical correlation with complications.