Isolated Sacral Extradural Hydatid Cyst with Posterior Paravertebral Extension Presenting as a Cauda Equina Syndrome
Bigyan Bhandari1, Binod Bijukachhe2, Prashant Adhikari3, Yogesh Acharya4
1 Consultant Orthopedic and Spine Surgeon, Department of Orthopedics, Grande International Hospital, Kathmandu, Nepal.
2 Consultant, Department of Orthopedics, Grande International Hospital, Kathmandu, Nepal.
3 Consultant Orthopedic and Spine Surgeon, Department of Orthopedics, Grande International Hospital, Kathmandu, Nepal.
4 Assistant Professor, Department of Epidemiology and Preventive Health, Avalon University School of Medicine, Willemstad, Netherlands.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Yogesh Acharya, Avalon University School of Medicine, Santa Rosaweg 122-124, Willemstad, Curacao, Netherland Antilles., Willemstad, Netherlands.
E-mail: dryogeshach@gmail.com
Hydatid disease is a ubiquitous parasitic zoonotic disease caused by Echinococcus granulosus. Humans are the accidental intermediate host and it primarily affect the liver and lungs. Isolated primary spinal hydatid disease is an uncommon variant of the musculoskeletal echinococcosis. Dorsal and lumbar spines are commonly affected. We present a rare case report of sacral intraspinal, extradural and posterior paravertebral hydatid cyst with soft tissue extension presenting as a cauda equine syndrome. The patient was started with on oral albendazole and surgery planned. Histopathological examination was consistent with hydatid cyst. The patient showed significant improvement in symptoms after the surgery with an uneventful postoperative course. There were no signs of recurrence in an interval Magnetic Resonance Imaging (MRI). Hydatid disease of the spine possesses a diagnostic and therapeutic challenge due to its varied presentation and difficult approach. Despite a significant advancement in diagnostic techniques and available pharmacological and non-pharmacological treatment modalities, it is associated with a high recurrence rate and increased morbidity.
Echinococcosis, Hydatid disease, Rare diseases, Surgery
Case Report
A 27-year-old female patient presented to the emergency department with difficulty passing urine for four weeks, associated with constipation for the last one week. She underwent primary treatment with urinary catheterisation in a local hospital and was referred to the spinal surgery unit after an initial evaluation. While in spinal surgery unit, a thorough examination was performed and investigations planned. Neurological examination revealed numbness over perineal region, lax anal tone, absent bulbocavernosus reflex; however, preserved lower limbs sensory and motor functions.
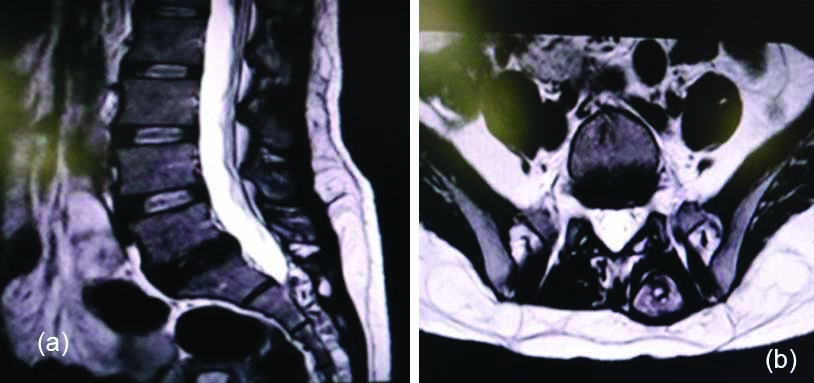
MRI spine and abdomen, X-ray chest and blood test were performed. Blood eosinophil and Immunoglobulin (IgE) levels were within normal limit and MRI of the abdomen and X-ray chest were unremarkable. MRI of the lumbosacral spine showed multiple cystic lesions displaying high signal in T2 with fat-suppressed images, however, low signal in T1 [Table/Fig-1]. These lesions completely filled the sacral spinal canal displacing the thecal sac anterior and right from the lower part of S1 superiorly to S5 inferiorly. There were also multiple cysts of varying sizes within the left para-spinal muscle (largest approximately 80×30×23 mm) extending from the lower part of L5 cranially to S4 caudally. They showed communication with the intra-spinal lesion at the level of left S3 and S4 foramina. Cytological examination of the ultrasound-guided aspiration of the lesion was inconclusive. The provisional diagnosis of “hydatid cyst” in the sacral spinal canal and left para-spinal muscle was made based on the MRI-spine, and the patient admitted for management accordingly.
(a) T2 Mid-Sagittal L-S spine; (b) T2 Para-sagittal L-S spine; (c) T2 axial image.

Management and outcome: The patient was started and maintained on oral albendazole (400 mg twice a day) and oral steroid (10 mg twice a day) for a week. A repeat MRI after one week revealed shrinkage of the cyst [Table/Fig-2]. There was some sensory improvement in the perianal region without reversal of the bowel and bladder dysfunction. Surgery was planned and approached through the posterior midline incision. Saline (3%) soaked gauge pads were kept in the operative field, keeping in mind the possibility of spillage of the cyst content around the surrounding tissue intraoperatively. The left para-spinal lesion was removed en bloc along with the cuff of para-spinal muscle and laminectomy of the S1-S4 sacral spine was performed. The cyst was removed in piece meal as there were no definitive planes between the cyst and the sacral roots [Table/Fig-3]. Hypertonic saline was used intraoperatively in the operative field. The patient had an uneventful postoperative period and sutures were removed after two weeks. The histopathological report of the cyst showed acellular and avascular eosinophilic refractile laminated membrane suggestive of echinococcosis and consistent with hydatid disease [Table/Fig-4].
(a) Preoperative Magnetic Resonance Imaging (MRI) scan of the patient after the patient was given oral albendazole for a week; (b) T2 axial image.
(a) Intraoperative sacral spinal canal showing the sacral roots after the cyst excision; (b) Spinal hydatidcyst after the excision.

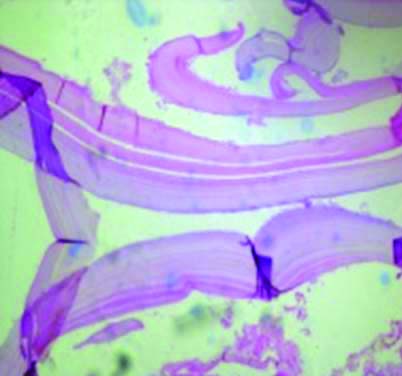
Histopathological image showing echinococcosis with acellulareosinophilicrefractile laminated membrane.
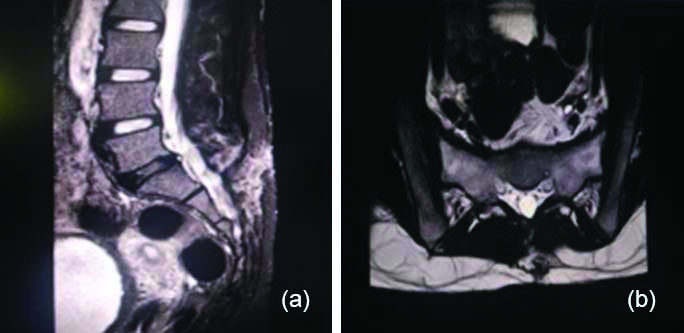
The patient was continued on oral albendazole (400 mg twice a day). Trial removal of the Foley’s catheter was done after two weeks and the patient was able to void on her own (post-void residual urine: 30 mL). The patient was followed up after 6 weeks, 3 months and again at 6 months. A follow-up MRI at 6 months did not show any evidence of recurrence of the disease [Table/Fig-5]. There was post-void residual urine of 200 mL with urinary bladder wall trabeculation in ultrasound abdomen which was managed with Clean Intermittent Catheterisation (CIC) after consultation with the urologist.
Postoperative Magnetic Resonance Imaging (MRI) scans of the patient taken after six months. (a) . Sagittal spine; (b) Axialimage.
Discussion
Hydatid disease is a ubiquitous parasitic zoonosis, attributed to the larval stage of the Echinococcus granulosus [1]. Humans are the accidental intermediate host and usually acquire these parasites through the ingestion of contaminated food and water with dog faeces [2].
The lesions are mostly cystic and are confined to the liver and lungs (80-90%) with infrequent bony involvement (0.5% to 4%), mostly confined to the spine (50%) and in particular thoracic and lumbar [3]. Spinal involvement is comparable to the malignant bone cancer (‘le cancer blanc’) due to its complicated sequelae, high morbidity, greater disability, and increased mortality [4].
Hydatid disease of the spine is classified into five different types by Braithwaite PA and Lees RF,: Type I (intramedullary); Type II (intradural, extramedullary); Type III (extradural, intraspinal); Type IV (vertebral); and Type V (paravertebral) [5]. The first three groups are rare, however, the last two groups are considered relatively common. The case we presented had cystic lesions in the extradural intra-spinal location of the sacral spinal canal along with left paravertebral involvement and does not fall under the Braithwaite PA and Lee RF classification. The posterior paravertebral muscle involvement in hydatid disease is a rare finding and concomitant involvement of the spinal canal along with the posterior paravertebral muscle has not been mentioned in the literature [6,7].
Ultrasonography can establish a presumptive diagnosis, whereas CT/MRI remains the mainstay of investigation used to determine the extent of the disease. MRI is considered to be superior to CT scan for hydatid disease [8,9]. The final diagnosis can be confirmed by histopathological examination of the cystic lesion. MRI of the abdomen and X-ray chest, although considered to be the commonest primary site of the infection, did not show any evidence of involvement of the liver and lungs in present case. Similarly, the primary involvement of the spinal canal in the sacral spine as seen in present patient is a rare finding [10,11].
Treatment of spinal hydatid disease should involve the combination of medical and surgical approach. Although questionable, albendazole is the only effective drug available for the treatment and as an adjunct to surgery in symptomatic patients [12]. Preoperative albendazole also acts as scolicidal agent, decreasing the risk of systemic dissemination [13]. As of now, there is no recommended guideline regarding the dose and duration of albendazole in musculoskeletal hydatid disease. The dose recommended by World Health Organization (WHO) for visceral echinococcosis is still the preferred choice. Cure of the residual cyst can be achieved through at least one year course of oral albendazole [14]. The recommended surgical treatment is laminectomy and excision of the lesion; however, complete cure is not possible if there is an involvement of the vertebral body [3]. Intraoperative use of agents like the hypertonic saline solution has been practiced but no significant difference in terms of recurrence rate has been observed [15].
Hydatid disease of the spine possesses a diagnostic and therapeutic challenge to the physicians because of its varied presentation, difficult approach and murky management protocol. It is associated with high recurrence rate as it is not always possible to remove all the cysts intraoperatively. This is complicated by an added risk of intraoperative cyst rupture, leading to dissemination of the Echinococcus at times [12]. Therefore, it is necessary that we diagnose the spinal hydatid disease early in the course to prevent complications and related co-morbidities.
Conclusion
Intra-spinal, extradural hydatid cyst with posterior paravertebral extension is a rare variant of the spinal hydatid disease and has not been reported in the literature yet. Isolated spinal echinococcosis without hepatic and pulmonary involvement can obscure the initial diagnostic clue leading to increased morbidity and mortality. It is imperative that we have a high index of suspicion to prevent the functional disabilities.
[1]. Schnepper GD, Johnson WD, Recurrent spinal hydatidosis in North America. Case report and review of the literatureNeurosurg Focus 2004 17(6):E810.3171/foc.2004.17.6.8 [Google Scholar] [CrossRef]
[2]. Moharamzad Y, Kharazi HH, Shobeiri E, Farzanegan G, Hashemi F, Namavari A, Disseminated intraspinal hydatid diseaseJ Neurosurg Spine 2008 8(5):490-93.10.3171/SPI/2008/8/5/49018447699 [Google Scholar] [CrossRef] [PubMed]
[3]. Ozdemir HM, Ogün TC, Tasbas B, A lasting solution is hard to achieve in primary hydatid disease of the spine: long-term results and an overviewSpine 2004 29(8):932-37.10.1097/00007632-200404150-0002215082999 [Google Scholar] [CrossRef] [PubMed]
[4]. Pedrosa I, Saíz A, Arrazola J, Ferreirós J, Pedrosa CS, Hydatid disease: radiologic and pathologic features and complicationsRadiogr Rev Publ Radiol Soc N Am Inc 2000 20(3):795-817.10.1148/radiographics.20.3.g00ma0679510835129 [Google Scholar] [CrossRef] [PubMed]
[5]. Braithwaite PA, Lees RF, Vertebral hydatid disease: radiological assessmentRadiology 1981 140(3):763-66.10.1148/radiology.140.3.72802477280247 [Google Scholar] [CrossRef] [PubMed]
[6]. Gourgiotis S, Stratopoulos C, Moustafellos P, Dimopoulos N, Papaxoinis G, Vougas V, Surgical techniques and treatment for hepatic hydatid cystsSurg Today 2007 37(5):389-95.10.1007/s00595-006-3398-z17468820 [Google Scholar] [CrossRef] [PubMed]
[7]. Iuliano L, Gurgo A, Polettini E, Gualdi G, De Marzio P, Musculoskeletal and adipose tissue hydatidosis based on the iatrogenic spreading of cystic fluid during surgery: report of a caseSurg Today 2000 30(10):947-49.10.1007/s00595007005211059740 [Google Scholar] [CrossRef] [PubMed]
[8]. Safioleas M, Nikiteas N, Stamatakos M, Safioleas C, Manti CH, Revenas C, Echinococcal cyst of the subcutaneous tissue: a rare case reportParasitol Int 2008 57(2):236-38.10.1016/j.parint.2007.11.00218203655 [Google Scholar] [CrossRef] [PubMed]
[9]. Doganay S, Kantarci M, Role of Conventional and diffusion-weighted magnetic resonance imaging of spinal treatment protocol for hydatid diseaseThe Journal of Spinal Cord Medicine 2009 32(5):574-77.10.1080/10790268.2009.1175456320025154 [Google Scholar] [CrossRef] [PubMed]
[10]. Joshi N, Hernandez-Martinez A, Seijas-Vazquez R, Primary sacral hydatid cyst. A case reportActa Orthop Belg 2007 73:674-77. [Google Scholar]
[11]. Abdelhakim K, Khalil A, Haroune B, Oubaid M, Mondher M, A case of sacral hydatid cystInternational Journal of Surgery Case Reports 2014 5(7):434-36.10.1016/j.ijscr.2014.03.02524912110 [Google Scholar] [CrossRef] [PubMed]
[12]. Prabhakar MM, Acharya AJ, Modi DR, Jadav B, Spinal hydatid disease: a case seriesThe Journal of Spinal Cord Medicine 2005 28(5):426-31.10.1080/10790268.2005.1175384316869090 [Google Scholar] [CrossRef] [PubMed]
[13]. Brunetti E, Kern P, Vuitton DA, Writing Panel for the WHO-IWGE. Expert consensus for the diagnosis and treatment of cystic and alveolar echinococcosis in humansActa Trop 2010 114(1):1-16.10.1016/j.actatropica.2009.11.00119931502 [Google Scholar] [CrossRef] [PubMed]
[14]. Baykaner MK, Doğulu F, Oztürk G, Edali N, Tali T, A viable residual spinal hydatid cyst cured with albendazole. Case reportJ Neurosurg 2000 93(1 Suppl):142-44.10.3171/spi.2000.93.1.014210879772 [Google Scholar] [CrossRef] [PubMed]
[15]. Lotfinia I, Sayyahmelli S, Mahdkhah A, Shoja MM, Intradural extramedullary primary hydatid cyst of the spine: a case report and review of literatureEuropean Spine Journal 2013 22(Suppl 3):329-36.10.1007/s00586-012-2373-122706667 [Google Scholar] [CrossRef] [PubMed]