Efficacy of Antibiotic-loaded Poly (Methyl Methacrylate) Beads in Orthopaedic Infections
Kaushik Bhowmick1, Chandrasekeran Gunasekaran2, Viju Daniel Varghese3, Abel Livingston4, Thilak Samuel Jepegnanam5, Alfred Job Daniel6, PRJVC Boopalan7
1 Assistant Professor, Department of Orthopaedics, Christian Medical College and Hospital, Vellore, Tamil Nadu, India.
2 Assistant Professor, Department of Orthopaedics, Christian Medical College and Hospital, Vellore, Tamil Nadu, India.
3 Associate Professor, Department of Orthopaedics, Christian Medical College and Hospital, Vellore, Tamil Nadu, India.
4 Assistant Professor, Department of Orthopaedics, Christian Medical College and Hospital, Vellore, Tamil Nadu, India.
5 Professor, Department of Orthopaedics, Christian Medical College and Hospital, Vellore, Tamil Nadu, India.
6 Professor, Department of Orthopaedics, Christian Medical College and Hospital, Vellore, Tamil Nadu, India.
7 Professor, Department of Orthopaedics, Christian Medical College and Hospital, Vellore, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Kaushik Bhowmick, Assistant Professor, Department of Orthopaedics, Christian Medical College and Hospital, Vellore-632004, Tamil Nadu, India.
E-mail: kaushikbhowmick97@yahoo.co.in
Introduction
Bone infections are associated with morbidity and mortality. Infection control is achieved by surgical debridement and microbial-specific antibiotic administration. Antibiotic Loaded Bone Cement (ALBC) has been accepted as a mode of treatment since systemic antibiotics alone are associated with higher recurrence and reoperation rates.
Aim
To assess the efficacy of ALBC in the treatment of orthopaedic infections.
Materials and Methods
A retrospective case series of 59 patients, treated for chronic musculoskeletal infections between January 2007 to December 2013, were included. They were divided into five groups; 1) Open fractures (21 patients); 2) Closed fractures (5 patients); 3) Infected nonunion (26 patients); 4) Infected implants (6 patients); and 5) Chronic osteomyelitis (1 patient).
Results
The median age at presentation was 34.8 years (range, 18.0-58.0). Five patients were lost to follow-up. In the 54 patients analysed, infection was controlled in all patients (100%) with debridement/implant exit and antibiotic beads. 31 patients (57%) united or were infection free with the primary procedure. This included all the patients in Group 4 and 5, six patients in Group 1 and 18 patients in Group 3. 23 patients (43%) underwent additional procedures to achieve bony union after the infection control. Gram-Negative Organisms (GNB) were isolated in 36% (21 cases), whereas Methicillin Resistant Staphylococcus Aureus (MRSA) was found in 12% (7 cases). The average healing time for GNB and MRSA infections was 19.4 months and eight months respectively.
Conclusion
The ALBC is effective in controlling infection. Infections caused by gram-negative bacteria are becoming common and they resolve later than MRSA infections.
Antibiotic bone cement, Chronic osteomyelitis, Gram negative bacteria, Infected non-union, Open fractures
Introduction
Infected nonunion and chronic osteomyelitis often occurs concurrently and pose a serious challenge to orthopaedic surgeons worldwide. Treatment strategies consume hospital and patient resources and therapies are long lasting with mediocre results. It has been estimated that the average treatment for infected nonunion of long bone costs as much as three times as treatment of a fresh fracture [1]. In India, where most patients do not have loss of employment and disability benefits from the government, there is a huge social and economic marginalisation [1-3].
Bone infections are associated with severe morbidity and mortality [4,5]. Drug resistance of pathogenic organisms and the relative avascularity at the fracture site secondary to scarring prevents systemic antibiotic concentration at the infection site [6]. Therefore, eradication of infection in nonunion and chronic osteomyelitis is a critical part of the treatment protocol. Infection control is achieved by surgical debridement and microbial-specific antibiotic administration.
Chronic osteomyelitis or infected nonunion treated with systemic antibiotics alone, without using local antibiotic delivery systems are associated with higher recurrence and reoperation rates [7]. Along with systemic antibiotics, local antibiotic delivery to the site of infection or nonunion has been accepted as a mode of treatment since the 70’s [8]. There are various local antibiotic delivery systems such as acrylic bone cement, Plaster of Paris, calcium sulfate, fibrin clots, synthetic polymers and composite biomaterials such as hydroxyapatite. Through, these delivery systems, we can achieve extremely high levels of local concentration of antibiotics without increasing their systemic toxicity. Currently, ALBC is used extensively, since it can adjust to various shapes and volumes, penetrate local cortical bone and avascular area, provide a structural function, cheap and provides a depot vehicle [9-17].
Many antimicrobial agents have been successfully incorporated into Polymethylmethacrylate (PMMA) cement for local delivery. Aminoglycosides and Vancomycin are common choices for prophylactic antibiotic delivery because of their broad spectrum of activity, heat stability and low allergenicity. With increasing gram-negative bacterial infections it is recommended to add a Carbapenem such as Meropenem to Vancomycin [11,18]. With the regular prophylactic and therapeutic use of PMMA loaded antibiotics, there has been an improvement in the outcome of open fractures and orthopaedic infections.
The present retrospective study was undertaken to assess the efficacy of antibiotic PMMA beads in the treatment of orthopaedic infections.
Materials and Methods
A retrospective case series of 59 patients with musculoskeletal infections, who were treated at a tertiary care referral Centre (Christian Medical College and Hospital, Vellore, India) between the years 2007-2013 were included in the study. All patients had undergone at least one surgical procedure at presentation prior to implantation of antibiotic-loaded PMMA beads. Patient and hospital consent was taken before conducting the study.
The diagnosis of infection was based on the presence of elevated serum markers of infection (ESR, CRP) or discharging sinus or preoperative radiographs suggestive of bone infection, implant osteolysis or both and peroperative findings of pus, dead bone and tissue. All the other blood parameters were checked before taking up the patients for surgery.
These patients were divided into five groups; 1) Open fractures (21 patients); 2) Closed fractures (5 patients); 3) Infected non-union (26 patients); 4) Infected implants (6 patients); and 5) Chronic osteomyelitis (1 patient). The details of the above five groups are mentioned in [Table/Fig-1].
Patient demographics based on the five different categories.
| Open fracture | Closed fractures | Infected non-unions | Infected implants | Chronic osteomyelitis |
|---|
| Total patients | 21 | 5 | 26 | 6 | 1 |
| Bones involved |
| Femur | 18 | 3 | 18 | 4 | Nil |
| Tibia | 1 | Nil | Nil | 1 | Nil |
| Forearm | 2 | 1 | 6 | Nil | Nil |
| Humerus | Nil | 1 | 2 | 1 | Nil |
| Ilium | Nil | Nil | Nil | Nil | 1 |
| Gustilo Anderson classification | | NA | NA | NA | NA |
| 1 | 1 | | | | |
| 2 | 1 | | | | |
| 3A | 5 | | | | |
| 3B | 14 | | | | |
| Fixation type | | | | | NA |
| Internal | 17 | 5 | 24 | 6 | |
| External | 4 | Nil | 2 | Nil | |
| Organism Isolated |
| MSSA | 1 | Nil | 6 | 1 | 1 |
| MRSA | 2 | Nil | 3 | 2 | Nil |
| Multiorganism | 1 | Nil | 4 | 1 | Nil |
| No growth | 5 | 2 | 2 | 1 | Nil |
| GNB | 9 | 1 | 9 | 1 | Nil |
| Others (Strep, Entrococci, coagulase negative staph) | 3 | 2 | 2 | Nil | Nil |
| Follow-up | 20 | 4 | 23 | 6 | 1 |
Operative Procedure
All patients underwent debridement, intraoperative cultures and antibiotic bead insertion. The wound was explored through the pre-existing scar. If the sinus tract was not through the previous scar, it was curetted separately. All unhealthy granulation tissue were removed. The cavities were decompressed, curetted, and thoroughly lavaged with copious quantities of normal saline. The implant was retained or exchanged based on peroperative findings. The antibiotic cement bead was prepared by adding the liquid monomer to the methyl methacrylate powder in an inert bowl. The appropriate antibiotic powders are added to this mixture in the early dough phase and mixed with a spatula to obtain a homogenous compound [12,19]. The choice of the antibiotic was determined by the culture report when available. Two antibiotics were chosen in the presence of mixed infections. When preoperative culture reports were unavailable, a broad-spectrum gram-positive and negative coverage was combined. We used 2 gm each of Meropenem and Vancomycin for a 40 gm batch of bone cement in such situations (total antibiotic concentration: 10%). The antibiotic loaded cement was made into spheres of 8-10 mm by rolling the cement between two palms and strung to a braided stainless steel wire. It was made sure that the beads were not in contact with each other so as to increase the surface area [19, 20]. The beads were placed in a close proximity to the infected tissue or bone. The wound was closed meticulously in layers over a suction drain. These beads were kept in vivo for a period of 6 to 8 weeks.
Postoperative Protocol
The suction drain was opened intermittently every 6 to 8 hours for 15 minutes to allow periodic drainage of the wound [19]. In addition, intravenous Cefazolin and Ciprofloxacin were given during the immediate postoperative period until the intraoperative culture results were obtained. In general, the sensitive antibiotics were administered for six weeks or more until there was a reduction in the levels of inflammatory markers such as C-Reactive Protein (CRP).
All patients were followed up every third day till wound healing and then every six weeks using radiographs whether fracture healed or not.
Results
Five patients were lost to follow-up out of the 59 patients. One patient was lost in the open fracture group (Group 1), one patient in the closed fracture group (Group 2) and three patients were lost in the infected nonunion group (Group 3) as shown in [Table/Fig-1]. The median age at presentation was 34.8 years (range, 18.0-58.0 years). In the 54 patients analysed, the infection was controlled in all patients (100%) with debridement/implant exit and antibiotic beads. The bones involved were femur-43, forearm-9, humerus-4, tibia-2 and ilium in one patient as shown in [Table/Fig-2]. The organisms identified and the combinations of antibiotics loaded in cement are shown in [Table/Fig-3,4] respectively. Out of 54 patients, 31 patients (57%) united or were infection free with the primary procedure. This included all the patients in the chronic osteomyelitis (Group 5) and the infected united fracture group (Group 4), six patients in the open fracture group (Group 1) and 18 patients in the infected nonunion group (Group 3). Twenty three patients (43%) underwent additional procedures to achieve bony union after the infection control [Table/Fig-5].
Distribution of bones involvement.
| Bones involved | Number of patients |
|---|
| Femur | 43 |
| Forearm | 9 |
| Humerus | 4 |
| Tibia | 2 |
| Ilium | 1 |
Distribution of organisms isolated.
| Isolated organisms | Total |
|---|
| Mixed organisms | 6 |
| Gram positive bacteria |
| MSSA Staphylococcus aureus | 8 |
| Methicillin-resistant Staphylococcus aureus | 7 |
| Beta hemolytic Streptococci | 2 |
| Coagulase negative Staphylococci | 1 |
| Enterococcus | 4 |
| Gram negative bacteria |
| Pseudomonas | 2 |
| Enterobacter | 5 |
| Escherichia coli | 6 |
| Proteus | 3 |
| Klebsiella | 3 |
| Citrobacter | 1 |
| Salmonella | 1 |
| No growth | 10 |
Antibiotic combinations and the various doses used in bone cement.
| Antibiotic combinations | |
|---|
| Vancomycin 2 gm+Meropenem 2 gm | 37 |
| Vancomycin 1 gm+Meropenem 1 gm | 11 |
| Vancomycin 2 gm | 7 |
| Meropenem 2 gm | 3 |
| Targocid (Teicoplanin) 4 gm | 1 |
Additional procedures required for bone union. Total numbers given in parenthesis.
| Procedures (23) | Open fracture (14) | Closed fractures (4) | Infected non-union (5) |
|---|
| Plate fixation | Femur-6 | Forearm-1 | Femur-1 |
| IM Nail | Femur-2 | | |
| External Fixation | Femur-3Tibia-1 | Femur-1 | Femur-1 |
| Bone grafting | Femur-2 | Femur-1 | Forearm-1 |
| Screw exchange | | Humerus-1 | |
| Soft tissue flaps | | | Lateral gastrocnemius-1 |
| Arthrodesis | | | Knee-1 |
In this study, GNB was isolated in 36% (21) cases, whereas MRSA was found in 12% (seven cases) of the cases. The average healing time for GNB and mixed infections and MRSA infections was 19.4 months and eight months.
Discussion
Musculoskeletal infection happens when microorganisms colonise the bone or orthopaedic implants, by haematogenous seeding or by direct inoculation. In the beginning, microorganisms are planktonic, later, on attachment to the implants; they become sessile, reduce their metabolic rate, and become covered by biofilm. Biofilm protects the microorganism from antimicrobials, opsonisation, and phagocytosis. To effectively eliminate bacteria in a biofilm, local antibiotic concentrations achieved must be 10 to 100.
Buchholz HW et al., used ALBC to treat infected arthroplasties [21]. Based on their work, ALBC was adapted to treat chronic bone infections and non-union. The various techniques include gentamycin impregnated cement beads, bead pouch technique and antibiotic impregnated cement in nails [8,9,22-25]. ALBC had become an established way to deliver high concentrations of the drug locally. Between beads and spacer blocks, elution characteristics are better observed with the former [11,19,20,26].
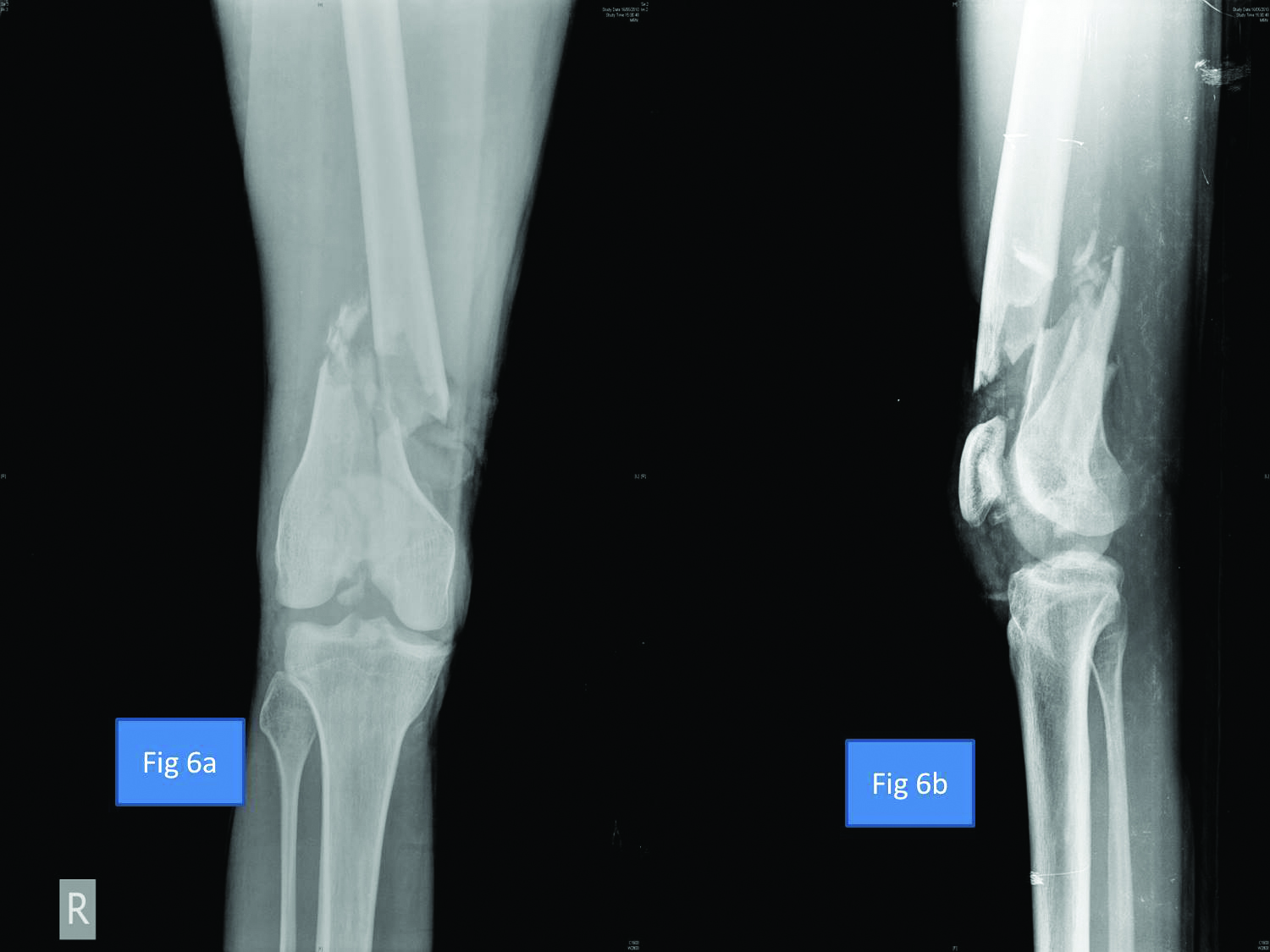
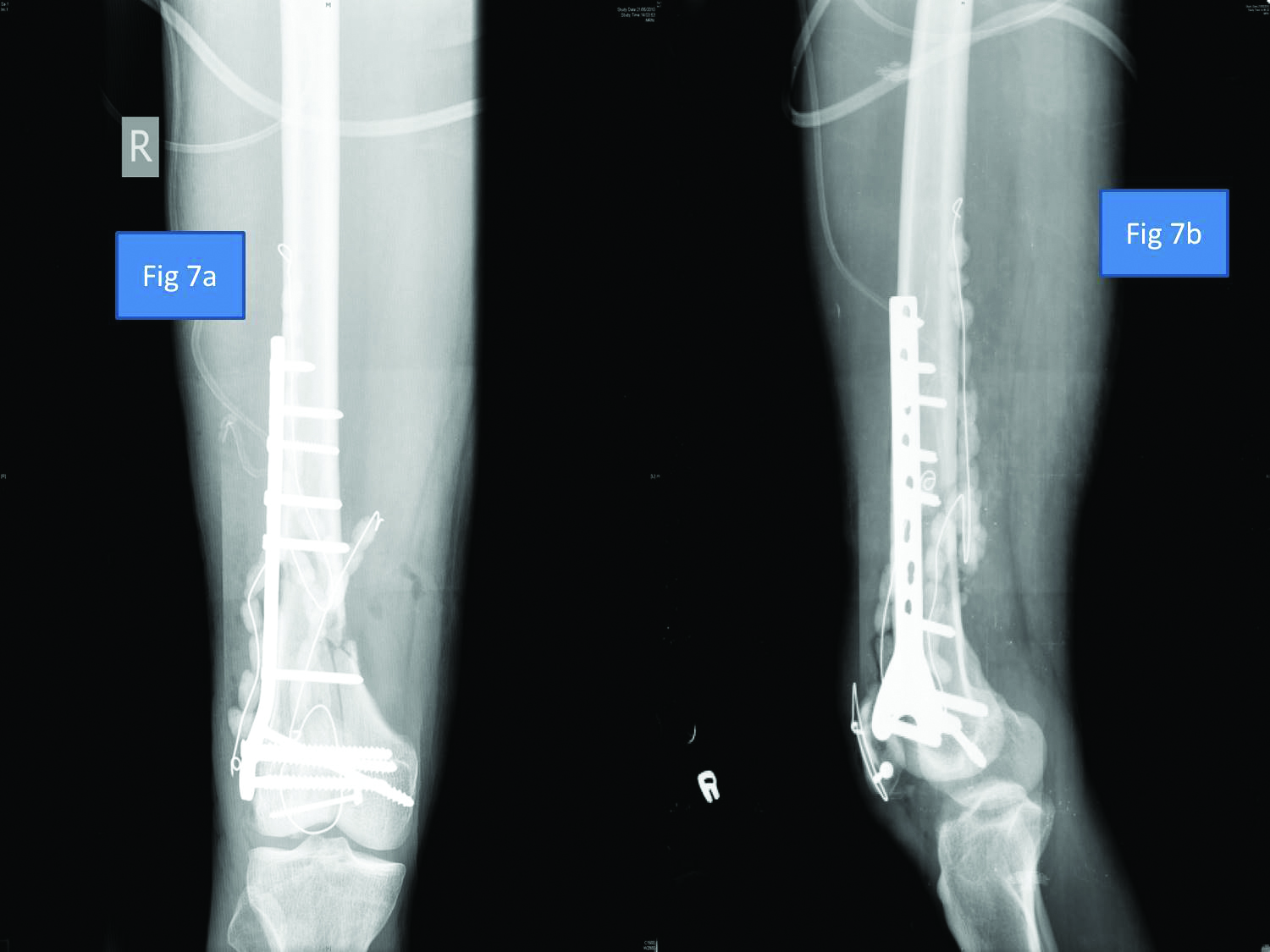
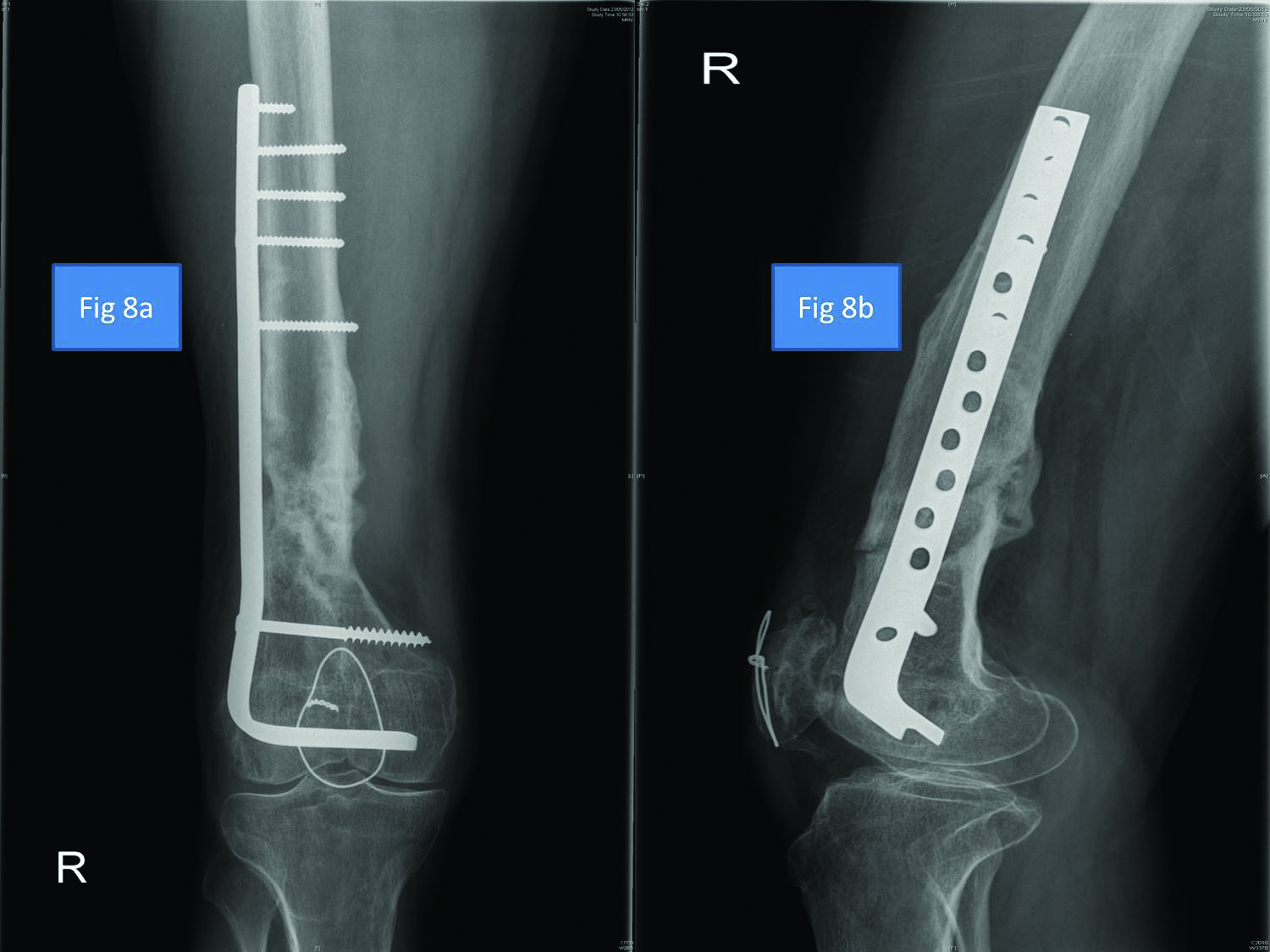
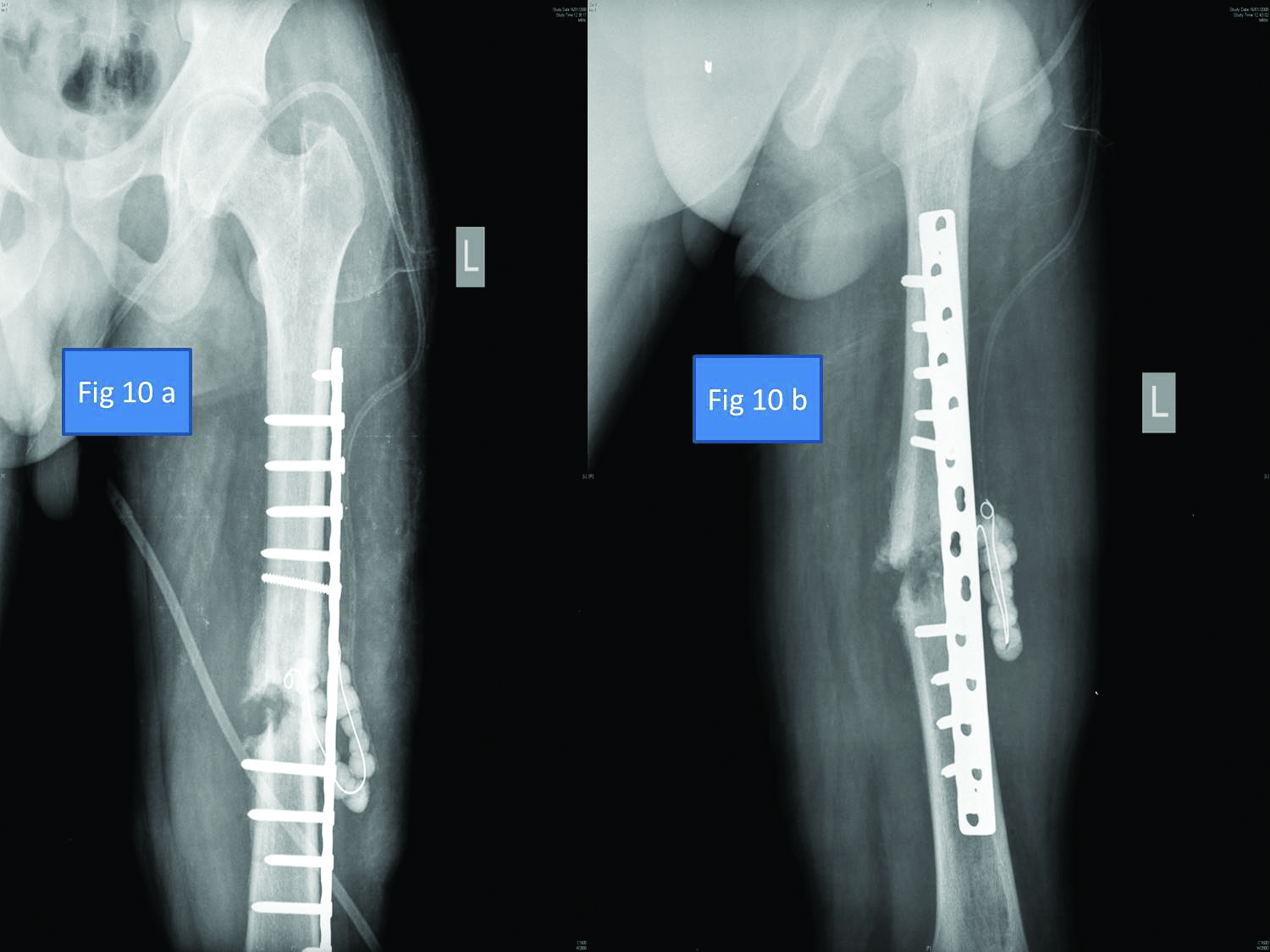
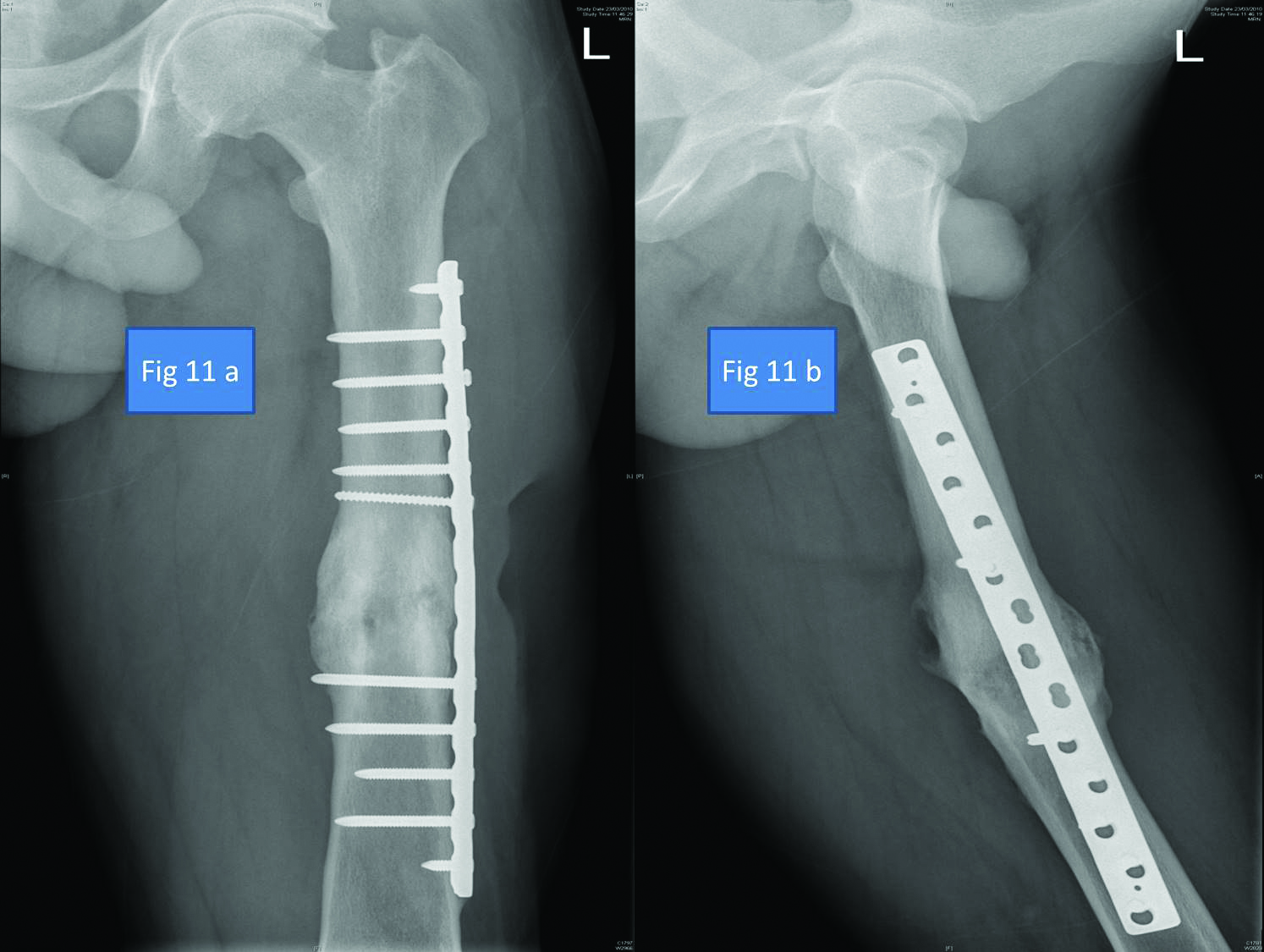
The optimum dosing of antibiotics in bone cement with regards to safety and efficacy has yet to be determined. The recommended antibiotic proportion is around 3% to 6% and a ratio of at least 3.6 grams of antibiotic per 40 grams of acrylic cement for effective elution and to maintain sustained therapeutic levels [5,8]. It is recommended to use higher doses of antibiotics in the cement when used as beads, as the antibiotic increases the cement porosity and elution characteristics. This retrospective study was undertaken to assess the efficacy of antibiotic PMMA beads in the treatment of orthopaedic infections. Prior studies on the use of ALBC have been either prophylactic use in open fractures or in infected fractures. In the study, we were able to achieve 100% infection control with the use of PMMA beads. The results of the current study are comparable to Klemm K and Mohanty SP et al., where infection control, in cases of chronic osteomyelitis has been achieved in more than 90% of cases [9,23]. The highlight of the present study is that it includes different groups of patients with established musculoskeletal infection ranging from osteomyelitis, open fractures as shown in [Table/Fig-6,7 and 8], infected implants to infected non-unions as shown in [Table/Fig-9,10 and 11] showing the efficacy of the PMMA beads in all types of clinical scenarios. Even in the patients, who required an additional procedure for the bone union, the infection was completely eradicated as shown in [Table/Fig-5].
Preoperative AP and Lateral radiograph of patient with open fracture of right distal femur.
Fixation of distal femur with plate and PMMA antibiotic beads for controlling infection.
Redo plating distal femur after infection control.
Infected nonunion left femur shaft with intra-medullary nail in situ.

Infection control with PMMA beads, nail exit and plating left femur shaft.
United left femur shaft after infection control with plate in situ.
The MRSA has been a major cause of infection in orthopaedics and bacterial resistance to aminoglycosides, especially in arthroplasties in the past two decades. This study shows the changing trend towards GNB in recent years. There was resolution of infection in two-thirds of cases (31 out of 54 cases), with the initial treatment. In 48% of patients, a second surgery was required for patients who grew GNB in the culture. With the emergence of GNB as a cause of implant-associated infections, changes have been made in the antibiotic regimens. The current recommendation is to add Vancomycin with a Carbapenem such as Meropenem prophylactically [27-30]. We have achieved control of infection and bone healing in 100% of present patients; although, the average healing time has been high in cases of GNB infections (average 19.4 months).
Limitation
The limitation of the study is its retrospective nature.
Conclusion
ALBC is effective in controlling infection. There is a changing trend towards predominant GNB and prophylactic antibiotic regimes should include GNB cover. GNB infections resolve later than MRSA infections. Finally, it is imperative to follow sound surgical principles to manage these difficulties, yet common orthopaedic conditions and use standardised antibiotic regimens as a guide to prevent microbial resistance.
[1]. Kanakaris NK, Giannoudis PV, The health economics of the treatment of long-bone non-unionsInjury 2007 38:S77-84.10.1016/S0020-1383(07)80012-X [Google Scholar] [CrossRef]
[2]. Patil S, Montgomery R, Management of complex tibial and femoral nonunion using the Ilizarov technique, and its cost implicationsJ Bone Joint Surg Br 2006 887:928-32.10.1302/0301-620X.88B7.1763916798998 [Google Scholar] [CrossRef] [PubMed]
[3]. Lavernia C, Lee DJ, Hernandez VH, The increasing financial burden of knee revision surgery in the United StatesClin Orthop Relat Res 2006 446:221-26.10.1097/01.blo.0000214424.67453.9a16672891 [Google Scholar] [CrossRef] [PubMed]
[4]. Zalavras CG, Patzakis MJ, Holtom P, Local antibiotic therapy in the treatment of open fractures and osteomyelitisClin Orthop Relat Res 2004 427:86-93.10.1097/01.blo.0000143571.18892.8d15552142 [Google Scholar] [CrossRef] [PubMed]
[5]. Hanssen AD, Spangehl MJ, Practical applications of antibiotic-loaded bone cement for treatment of infected joint replacementsClinical Orthopaedics and Related Research 2004 27:79-85.10.1097/01.blo.0000143806.72379.7d15552141 [Google Scholar] [CrossRef] [PubMed]
[6]. Holtom PD, Patzakis MJ, Newer methods of antimicrobial delivery for bone and joint infectionsInstr Course Lect 2003 52:745-49. [Google Scholar]
[7]. Castaneda P, McLaren A, Tavaziva G, Overstreet D, Biofilm antimicrobial susceptibility increases with antimicrobial exposure timeClin Orthop Relat Res 2016 4747:1659-64.10.1007/s11999-016-4700-z26797908 [Google Scholar] [CrossRef] [PubMed]
[8]. Hanssen AD, Local antibiotic delivery vehicles in the treatment of musculoskeletal infectionClin Orthop Relat Res 2005 437:91-96.10.1097/01.blo.0000175713.30506.7716056032 [Google Scholar] [CrossRef] [PubMed]
[9]. Klemm K, The use of antibiotic-containing bead chains in the treatment of chronic bone infectionsClin Microbiol Infect 2001 71:28-31.10.1046/j.1469-0691.2001.00186.x11284941 [Google Scholar] [CrossRef] [PubMed]
[10]. Joseph TN, Chen AL, Di Cesare PE, Use of antibiotic-impregnated cement in total joint arthroplastyJ Am Acad Orthop Surg 2003 111:38-47.10.5435/00124635-200301000-00006 [Google Scholar] [CrossRef]
[11]. Samuel S, Mathew BS, Veeraraghavan B, Fleming DH, Chittaranjan SB, Prakash JA, In vitro study of elution kinetics and bio-activity of meropenem-loaded acrylic bone cementJ Orthop133:131-36.10.1007/s10195-012-0191-122461001 [Google Scholar] [CrossRef] [PubMed]
[12]. Anagnostakos K, Hitzler P, Pape D, Kohn D, Kelm J, Persistence of bacterial growth on antibiotic-loaded beads: is it actually a problem?Acta Orthop 2008 792:302-07.10.1080/1745367071001512018484259 [Google Scholar] [CrossRef] [PubMed]
[13]. Patzakis MJ, Zalavras CG, Chronic posttraumatic osteomyelitis and infected nonunion of the tibia: current management conceptsJ Am Acad Orthop Surg 2005 136:417-27.10.5435/00124635-200510000-0000616224114 [Google Scholar] [CrossRef] [PubMed]
[14]. Decoster TA, Bozorgnia S, Antibiotic beadsJ Am Acad Orthop Surg 2008 1611:674-78.10.5435/00124635-200811000-0000818978290 [Google Scholar] [CrossRef] [PubMed]
[15]. Torbert JT, Joshi M, Moraff A, Matuszewski PE, Holmes A, Pollak AN, Current bacterial speciation and antibiotic resistance in deep infections after operative fixation of fracturesJ Orthop Trauma 2015 291:7-17.10.1097/BOT.000000000000015824854665 [Google Scholar] [CrossRef] [PubMed]
[16]. Beals RK, Bryant RE, The treatment of chronic open osteomyelitis of the tibia in adultsClin Orthop Relat Res 2005 433:212-17.10.1097/01.blo.0000150462.41498.fe15805960 [Google Scholar] [CrossRef] [PubMed]
[17]. Goyal N, Miller A, Tripathi M, Parvizi J, Methicillin-resistant Staphylococcus aureus (MRSA): colonisation and pre-operative screeningThe bone & Joint Journal 2013 95-B1:4-9.10.1302/0301-620X.95B1.2797323307666 [Google Scholar] [CrossRef] [PubMed]
[18]. Cui Q, Mihalko WM, Shields JS, Ries M, Saleh KJ, Antibiotic-impregnated cement spacers for the treatment of infection associated with total hip or knee arthroplastyJ Bone Joint Surg Am 2007 894:871-82.10.2106/00004623-200704000-00026 [Google Scholar] [CrossRef]
[19]. Samuel S, Ismavel R, Boopalan PR, Matthai T, Practical considerations in the making and use of high-dose antibiotic-loaded bone cementActa Orthopaedica Belgica 2010 764:543-45. [Google Scholar]
[20]. Anagnostakos K, Wilmes P, Schmitt E, Kelm J, Elution of gentamicin and vancomycin from polymethylmethacrylate beads and hip spacers in vivoActa Orthop 2009 802:193-97.10.3109/1745367090288470019404802 [Google Scholar] [CrossRef] [PubMed]
[21]. Buchholz HW, Elson RA, Engelbrecht E, Lodenkamper H, Rottger J, Siegel A, Management of deep infection of total hip replacementJournal of Bone and Joint Surgery 1981 63B:342-53.10.1302/0301-620X.63B3.7021561 [Google Scholar] [CrossRef]
[22]. Nelson CL, The current status of material used for depot delivery of drugsClin Orthop Relat Res 2004 427:72-78.10.1097/01.blo.0000143741.92384.1815552140 [Google Scholar] [CrossRef] [PubMed]
[23]. Mohanty SP, Kumar MN, Murthy NS, Use of antibiotic-loaded polymethyl methacrylate beads in the management of musculoskeletal sepsis--a retrospective studyJ Orthop Surg (Hong Kong) 2003 111:73-79.10.1177/23094990030110011512810976 [Google Scholar] [CrossRef] [PubMed]
[24]. Baleani M, Persson C, Zolezzi C, Andollina A, Borrelli AM, Tigani D, Biological and biomechanical effects of vancomycin and meropenem in acrylic bone cementJ Arthroplasty 2008 238:1232-38.10.1016/j.arth.2007.10.01018534473 [Google Scholar] [CrossRef] [PubMed]
[25]. Rasyid HN, van der Mei HC, Frijlink HW, Soegijoko S, van Horn JR, Busscher HJ, Concepts for increasing gentamicin release from handmade bone cement beadsActa Orthop 2009 805:508-13.10.3109/1745367090338978219916680 [Google Scholar] [CrossRef] [PubMed]
[26]. Hetrick EM, Schoenfisch MH, Reducing implant-related infections: active release strategiesChemical Society Reviews 2006 359:78010.1039/b515219b16936926 [Google Scholar] [CrossRef] [PubMed]
[27]. Taggart T, Kerry RM, Norman P, Stockley I, The use of vancomycin-impregnated cement beads in the management of infection of prosthetic jointsJ Bone Joint Surg Br 2002 841:70-72.10.1302/0301-620X.84B1.0840070 [Google Scholar] [CrossRef]
[28]. Thonse R, Conway JD, Antibiotic cement-coated nails for the treatment of infected nonunions and segmental bone defectsJ Bone Joint Surg Am 2008 90(Suppl 4):163-74.10.2106/JBJS.H.0075318984728 [Google Scholar] [CrossRef] [PubMed]
[29]. Fan C-Y, Hsieh M-S, Chen W-M, Chen C-F, Successful management of infected intramedullary nailing with reaming, lavage, and insertion of antibiotic-impregnated cement rodsJournal of Experimental & Clinical Medicine 2011 33:137-41.10.1016/j.jecm.2011.04.002 [Google Scholar] [CrossRef]
[30]. Galfat D, Agnihotri A, Bansal A, Management of infected non union of long bones with antibiotic impregnated cement nailNational Journal of Medical and Dental Research 2013 12:14 [Google Scholar]