Difficulties in obtaining satisfactory treatment with the standard edgewise technique resulted in the development of brackets with built-in torque in the early 1960s. Ten years later the Straight Wire Appliance (SWA) was introduced, in which the 1st, 2nd, and 3rd order angulation were systematically transferred from wires to brackets. Lately, such preadjusted appliances have been produced based on different prescriptions [1]. However, the principle has always been the same, that bends in all three dimensions of space are replaced by a sophisticated bracket design. Theoretically, with all brackets in an optimal position, a pre-shaped arch wire will bring all teeth into their ideal position [2].
In the past limited studies comparing the accuracy of bracket placement between direct and indirect bonding techniques have been done [3-8]. Digital processing helped in elimination of any manual tracing steps thereby increasing the accuracy. Further, it enabled a more accurate comparison through a lower least count of measurement. It is beneficial to know if there is a difference in the accuracy of bracket placement between direct and indirect bonding techniques, as the less accurate the positioning of brackets, the more poorly they perform. An ideally bonded bracket would conform to the researched and documented orthodontic mechanics and corresponding position of bracket vis-à-vis the tooth [1]. Irrespective of the efficacy of diagnosis and prescription, brackets, if positioned incorrectly can lead to increased time of treatment and may also increase the time and number of arch wire adjustments.
The purpose of the present study has been to evaluate the accuracy of bracket placement by direct and indirect bonding techniques by digital image processing and comparing the accuracy of bracket placement by direct and indirect bonding techniques. The study aims to prove/disapprove the null hypothesis that there is no difference in accuracy of bracket placement using the two bonding techniques.
Materials and Methods
This study was conducted at DAV Dental College, Haryana, India between June 2011 to May 2012. It focused on a patient with Class II division 1 malocclusion and mild crowding. The patient had normal and fully erupted teeth with no consideration to third molars. There was no erosion, fracture or previous restoration on the incisor edge or cusp tip. There was no tooth size discrepancy and the malocclusion did not hinder the ideal positioning of brackets.
Thirteen sets of duplicated stone models (Kaldent, Dental Plaster Class II, Kalabhai, Mumbai) were prepared from one set of selected original pre-treatment orthodontic models using Agar hydrocolloid (Wirogel M, Bego, Germany) & divided into following three groups: 1) one set for predetermined “ideal” bracket placement; 2) six sets for direct bonding; 3) six sets for indirect bonding.
Bonding procedure: Pre-adjusted edgewise orthodontic brackets (.022’’-3M/UNITEKTM Gemini Metal Brackets, Monrovia, California) were bonded from second premolar to second premolar on all the models of three groups. A graphite marker was used to mark the long axis of the crown from midpoint of incisal edge or cusp tip and extending down the facial surface to gingival margin, and vertical height (from center of the bracket slot to the incisal edge/occlusal tip of crown) of bracket was measured with Boone gauge (3M/Unitek Corp, Monrovia, California) at 3.5mm for incisors, 4 mm for canine, and 3.5 mm for premolars [9].
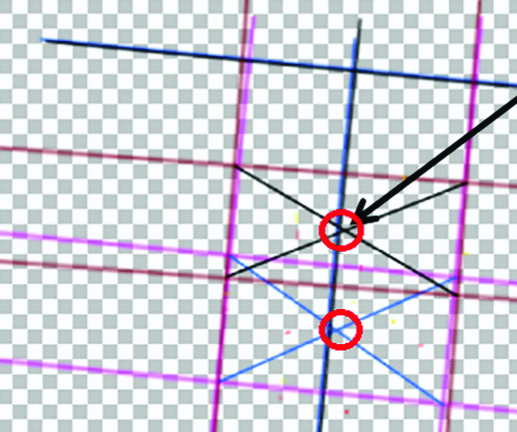
Ideal bracket placement: A bracket which conforms to the researched and documented orthodontic mechanics and corresponding position of bracket vis-à-vis the tooth is deemed to be ideal [1]. Buccal/labial surface of each tooth was prepared by sandblasting. All teeth from second premolar to second premolar were sectioned carefully with a small saw (Dentaurum, Dental Technology) with replaceable blades (Blade No. 180-702-00, Dentaurum) without breaking the contour of crown. This was done to eliminate mild crowding and rotations and then the teeth were reset in wax cautiously [Table/Fig-1]. To ensure ideal bracket placement, it was evaluated by five experienced orthodontists repeatedly until it was approved to be accurate by all of them and then brackets were light cured for 50 seconds on all sides/tooth [3,4].
Ideal bracket placement group models with bonded brackets.

Direct bonding: Each set of model of this group was mounted on mannequin to simulate a realistic clinical situation and brackets were bonded with light cure adhesive on all teeth of the mounted models from second premolar to second premolar at their correct position and light cured for 50 seconds on all sides/tooth. Same procedure was repeated for remaining five sets of models of this group by five experienced orthodontists.
Indirect bonding: Separating medium (DPI Heat cure Coldmold seal) was painted on the buccal/labial surface of each tooth of one set of models from this group. Brackets were placed on each tooth at their correct position with a water soluble temporary adhesive (Aleene’s original Tacky glue, Buelton, CA) [10,11]. A transfer tray was formed using Soft Bioplast sheet (2mm thick) (Scheu dental, Germany) on a mini STAR high vacuum former (Scheu dental, Germany).
The models with transfer tray were soaked in water for few minutes to allow dissolution of water soluble temporary adhesive from the bracket bases. Transfer tray was removed from the model and trimmed with scissors close to the gingival edges of each tooth. Buccal/labial surface of each tooth of this set of models was prepared by sandblasting. Each tooth was primed and then a thin layer of light cure adhesive was applied on each of the bracket bases.
Each bracket was light cured for 50 seconds on all sides/tooth. Same procedure was repeated for remaining five sets of models of this group by five experienced orthodontists.
To enable digital superimposition between the images of the three bonding groups, two reference marks were required. So the preserved models of all the three groups were taken and their long axis already marked, if any, were cleaned with absolute alcohol and two reference marks were scribed along the long axis of each tooth by the same person who performed the bonding of ideal bracket placement group.
Tooth sectioning: Each bonded tooth of the two experimental groups were sectioned carefully with a small saw without breaking the contour of the crown and labelled and preserved group wise.
Image capture and processing: Image was captured using a digital SLR camera (Nikon D3000) under consistent lighting and background setting. The camera was set to a consistent magnification (f=55mm) for all the captures. A customised jig was designed to engage the sectioned tooth at a fixed distance of 110mm from the camera lens as measured with a Vernier Caliper (Mitutoyo-JAPAN) with a least count of 0.01 mm.
Images were then imported to a computer and bracket outlines were marked out [Table/Fig-2]. Paint.Net v3.5.8 software with support for multiple layers was used for image processing.
Steps of image processing.

“Tooth and Bracket Skeleton” was separated from tooth in background by switching off the background layer. Skeletons from Direct and Indirect bonding were superimposed on those from Ideal bonding. Difference between the bracket position was thus measurable in pixels while angulation could be measured in degrees [Table/Fig-3a,b]. This process was repeated for processing the images of all sectioned teeth [10,12].
Creating the Tooth and Bracket Skeleton.

The error was converted from pixels to mm using a reference line.
Data collection: Two linear and one angular differential between the ideal group and experimental groups were measured.
Bracket height: Centre point of the ideal bracket was set as zero. If bracket of either of the two groups was placed occlusal to ideal, the value was ‘+’, and ‘–’ meant the bracket was gingival to ideal.
Bracket height on lower left premolar (LL4), mesiodistal position on upper right first molar (UR3) and LL4, and angular placement on lower right first premolar (LR4) and upper right first premolar (UR4).
Mesiodistal position: Centre point of the ideal bracket was set as zero. If bracket of either of the two groups was placed mesial to ideal, the value was ‘+’, and ‘–’meant the bracket was distal to ideal.
Angulation: Angulation was determined by the angle between bracket top marking of the experimental groups and ideal group. With ideal as a base, if experimental group was positioned clockwise, value was ‘–’, otherwise it was recorded as ‘+’.
Reproducibility testing: Measurements for selected teeth were repeated three times and correlation between repeated measurements was used to establish repeatability of the process. Pearson correlation coefficient close to unity (p<.01) confirms the reproducibility of the digital processing method.
Statistical Analysis
For mean and standard deviation of differentials between the ideal group and the experimental groups, absolute values were used for all the measurements. Kolmogorov-Smirnov test showed normal distribution of data. A student’s t-test was used to determine whether statistically significant differences (p≤0.05) existed among ideal and experimental groups. Statistical analysis was done using SPSS (Statistical Package for Social Sciences –v15.0) software.
Results
Bracket height: [Table/Fig-4a,b] shows error in bracket height between ideal group and the direct/indirect bonding groups. Average error in bracket height for direct and indirect bonding was 0.431 mm and 0.395 mm respectively.
Distribution of bracket height measurements.
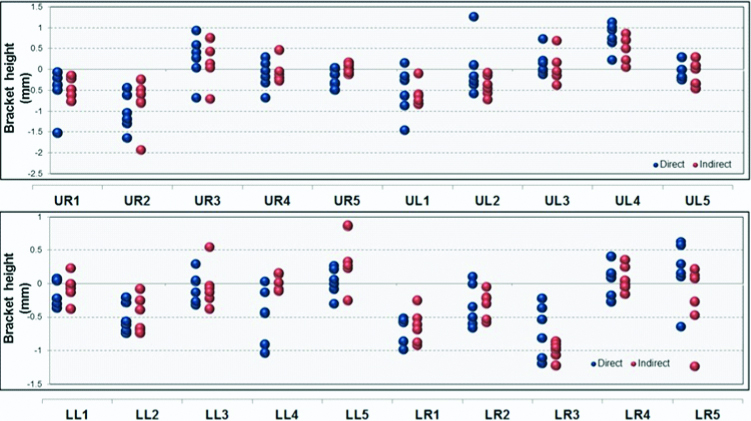
Comparison of bracket height measurements.
| Bracket height (Unpaired t-test) |
|---|
| Direct | Indirect | Difference of mean | Statistical significance |
|---|
| Mean | Stdev | Mean | Stdev | | t value | p-value |
|---|
| LL1 | 0.177 | 0.134 | 0.136 | 0.145 | 0.042 | 0.517 | 0.62 |
| LL2 | 0.516 | 0.222 | 0.467 | 0.269 | 0.050 | 0.348 | 0.74 |
| LL3 | 0.180 | 0.128 | 0.227 | 0.200 | -0.047 | -0.484 | 0.64 |
| LL4 | 0.493 | 0.405 | 0.110 | 0.055 | 0.383 | 2.295 | 0.05 |
| LL5 | 0.154 | 0.123 | 0.469 | 0.311 | -0.315 | -2.314 | 0.06 |
| LR1 | 0.675 | 0.197 | 0.644 | 0.247 | 0.031 | 0.242 | 0.81 |
| LR2 | 0.368 | 0.266 | 0.313 | 0.205 | 0.055 | 0.399 | 0.7 |
| LR3 | 0.704 | 0.399 | 0.998 | 0.129 | -0.295 | -1.721 | 0.12 |
| LR4 | 0.206 | 0.113 | 0.146 | 0.137 | 0.060 | 0.827 | 0.43 |
| LR5 | 0.401 | 0.243 | 0.399 | 0.432 | 0.003 | 0.013 | 0.99 |
| UL1 | 0.584 | 0.512 | 0.618 | 0.274 | -0.034 | -0.143 | 0.89 |
| UL2 | 0.459 | 0.429 | 0.386 | 0.246 | 0.073 | 0.361 | 0.73 |
| UL3 | 0.211 | 0.268 | 0.261 | 0.236 | -0.050 | -0.34 | 0.74 |
| UL4 | 0.792 | 0.325 | 0.511 | 0.308 | 0.282 | 1.539 | 0.16 |
| UL5 | 0.180 | 0.099 | 0.255 | 0.166 | -0.076 | -0.957 | 0.36 |
| UR1 | 0.500 | 0.519 | 0.396 | 0.259 | 0.104 | 0.44 | 0.67 |
| UR2 | 1.035 | 0.447 | 0.798 | 0.589 | 0.237 | 0.786 | 0.45 |
| UR3 | 0.493 | 0.313 | 0.474 | 0.319 | 0.018 | 0.1 | 0.92 |
| UR4 | 0.271 | 0.223 | 0.216 | 0.147 | 0.055 | 0.503 | 0.63 |
| UR5 | 0.219 | 0.189 | 0.083 | 0.061 | 0.136 | 1.675 | 0.15 |
| Overall | 0.431 | 0.368 | 0.395 | 0.337 | 0.036 | 0.790 | 0.430 |
Mesiodistal positioning: [Table/Fig-5a,b] shows the error in mesiodistal positioning. Average error in mesiodistal for direct and indirect bonding was 0.284 mm and 0.252 mm respectively.
Distribution of mesiodistal measurements.
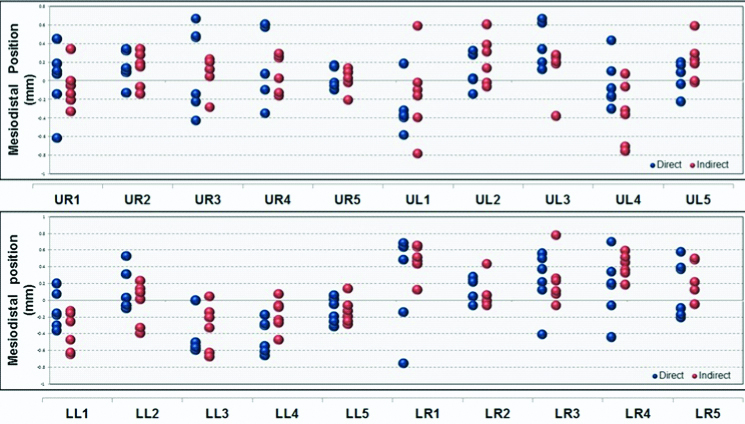
Comparison of mesiodistal position measurements.
| Mesiodistal positioning (Unpaired t-test) |
|---|
| Direct | Indirect | Difference of mean | Statistical significance |
|---|
| Mean | SD | Mean | SD | | t value | p-value |
|---|
| LL1 | 0.211 | 0.102 | 0.378 | 0.232 | -0.167 | -1.615 | 0.151 |
| LL2 | 0.182 | 0.199 | 0.201 | 0.143 | -0.018 | -0.182 | 0.859 |
| LL3 | 0.464 | 0.230 | 0.336 | 0.259 | 0.128 | 0.903 | 0.388 |
| LL4 | 0.427 | 0.202 | 0.198 | 0.159 | 0.229 | 2.186 | 0.054 |
| LL5 | 0.146 | 0.122 | 0.175 | 0.082 | -0.029 | -0.479 | 0.642 |
| LR1 | 0.558 | 0.222 | 0.474 | 0.193 | 0.083 | 0.694 | 0.504 |
| LR2 | 0.151 | 0.110 | 0.107 | 0.164 | 0.044 | 0.548 | 0.596 |
| LR3 | 0.365 | 0.166 | 0.255 | 0.271 | 0.109 | 0.843 | 0.419 |
| LR4 | 0.323 | 0.228 | 0.407 | 0.145 | -0.083 | -0.756 | 0.467 |
| LR5 | 0.302 | 0.179 | 0.237 | 0.208 | 0.065 | 0.582 | 0.573 |
| UL1 | 0.368 | 0.127 | 0.339 | 0.304 | 0.029 | 0.213 | 0.835 |
| UL2 | 0.138 | 0.138 | 0.255 | 0.226 | -0.117 | -1.086 | 0.303 |
| UL3 | 0.349 | 0.246 | 0.261 | 0.067 | 0.089 | 0.851 | 0.429 |
| UL4 | 0.209 | 0.135 | 0.378 | 0.296 | -0.169 | -1.274 | 0.231 |
| UL5 | 0.136 | 0.074 | 0.222 | 0.218 | -0.086 | -0.916 | 0.381 |
| UR1 | 0.263 | 0.217 | 0.177 | 0.142 | 0.086 | 0.813 | 0.435 |
| UR2 | 0.190 | 0.114 | 0.195 | 0.102 | -0.005 | -0.083 | 0.935 |
| UR3 | 0.401 | 0.193 | 0.169 | 0.086 | 0.232 | 2.687 | 0.023* |
| UR4 | 0.386 | 0.253 | 0.188 | 0.101 | 0.198 | 1.782 | 0.105 |
| UR5 | 0.107 | 0.065 | 0.096 | 0.070 | 0.010 | 0.268 | 0.794 |
| Overall | 0.284 | 0.204 | 0.252 | 0.200 | 0.031 | 1.227 | 0.221 |
Angular positioning: [Table/Fig-6a,b] shows the error in angular positioning. Average error in angular positioning for direct and indirect bonding was 2.884 degrees and 3.099 mm respectively.
Distribution of angular measurements.
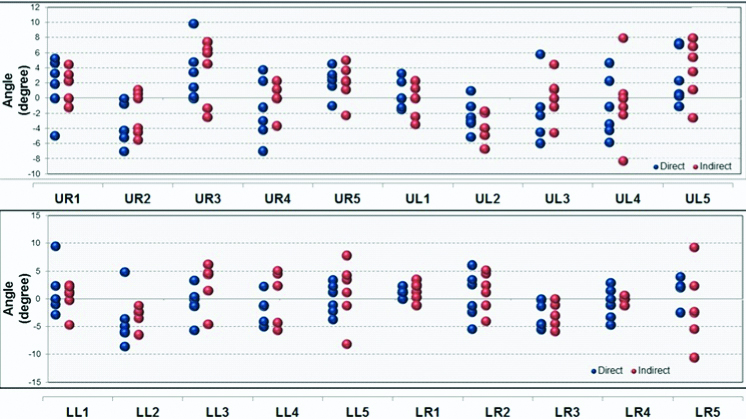
Comparison of angular measurements.
| Angulation (Unpaired t-test) |
|---|
| Direct | Indirect | Difference of mean | Statistical significance |
|---|
| Mean | SD | Mean | SD | | t value | p-value |
|---|
| LL1 | 2.602 | 3.556 | 1.965 | 1.541 | 0.637 | 0.402 | 0.696 |
| LL2 | 5.632 | 1.696 | 3.042 | 1.824 | 2.590 | 2.547 | 0.029* |
| LL3 | 1.943 | 2.127 | 4.302 | 1.534 | -2.358 | -2.203 | 0.052 |
| LL4 | 2.487 | 1.654 | 4.023 | 1.382 | -1.537 | -1.746 | 0.111 |
| LL5 | 2.308 | 1.074 | 4.338 | 3.073 | -2.030 | -1.626 | 0.135 |
| LR1 | 1.222 | 0.759 | 1.842 | 1.150 | -0.620 | -1.102 | 0.296 |
| LR2 | 3.507 | 1.867 | 3.083 | 1.754 | 0.423 | 0.405 | 0.694 |
| LR3 | 2.688 | 2.457 | 2.402 | 2.443 | 0.287 | 0.203 | 0.843 |
| LR4 | 2.227 | 1.683 | 0.303 | 0.509 | 1.923 | 2.679 | 0.037* |
| LR5 | 2.513 | 0.745 | 5.390 | 3.717 | -2.877 | -1.859 | 0.118 |
| UL1 | 1.355 | 1.275 | 1.577 | 1.396 | -0.222 | -0.287 | 0.780 |
| UL2 | 2.650 | 1.523 | 3.488 | 2.047 | -0.838 | -0.805 | 0.440 |
| UL3 | 3.475 | 2.227 | 2.102 | 1.933 | 1.373 | 1.141 | 0.281 |
| UL4 | 3.592 | 1.699 | 3.373 | 3.760 | 0.218 | 0.130 | 0.901 |
| UL5 | 3.117 | 3.244 | 4.585 | 2.607 | -1.468 | -0.864 | 0.408 |
| UR1 | 3.352 | 2.068 | 2.228 | 1.544 | 1.123 | 1.066 | 0.311 |
| UR2 | 3.593 | 2.677 | 2.608 | 2.317 | 0.985 | 0.681 | 0.511 |
| UR3 | 3.280 | 3.715 | 4.703 | 2.394 | -1.423 | -0.789 | 0.448 |
| UR4 | 3.560 | 1.982 | 1.188 | 1.517 | 2.372 | 2.327 | 0.042* |
| UR5 | 2.577 | 1.244 | 2.772 | 1.350 | -0.195 | -0.260 | 0.800 |
| Overall | 2.884 | 2.164 | 3.099 | 2.477 | -0.215 | 0.716 | 0.475 |
Coefficient of variation: [Table/Fig-7] depicts the overall coefficient of variation for each of the three measurements. It can be used to compare dispersion across measurements in different units.
Overall coefficient of variation.
| Mesiodistal positioning (Coefficient of variation) | Bracket height (Coefficient of variation) | Angulation (Coefficient of variation) |
|---|
| Direct | Indirect | | Direct | Indirect | | Direct | Indirect |
|---|
| LL1 | 0.482 | 0.513 | LL1 | 0.754 | 1.072 | LL1 | 1.367 | 0.784 |
| LL2 | 1.092 | 0.397 | LL2 | 0.431 | 0.576 | LL2 | 0.301 | 0.600 |
| LL3 | 0.495 | 0.492 | LL3 | 0.710 | 0.883 | LL3 | 1.095 | 0.356 |
| LL4 | 0.472 | 0.672 | LL4 | 0.821 | 0.501 | LL4 | 0.665 | 0.344 |
| LL5 | 0.835 | 0.393 | LL5 | 0.797 | 0.662 | LL5 | 0.465 | 0.708 |
| LR1 | 0.399 | 0.633 | LR1 | 0.292 | 0.384 | LR1 | 0.621 | 0.625 |
| LR2 | 0.731 | 1.077 | LR2 | 0.725 | 0.656 | LR2 | 0.532 | 0.569 |
| LR3 | 0.456 | 0.779 | LR3 | 0.567 | 0.129 | LR3 | 0.914 | 1.017 |
| LR4 | 0.704 | 0.315 | LR4 | 0.551 | 0.936 | LR4 | 0.756 | 1.679 |
| LR5 | 0.591 | 0.531 | LR5 | 0.605 | 1.083 | LR5 | 0.296 | 0.690 |
| UL1 | 0.345 | 0.553 | UL1 | 0.878 | 0.444 | UL1 | 0.941 | 0.885 |
| UL2 | 0.996 | 0.476 | UL2 | 0.936 | 0.638 | UL2 | 0.575 | 0.587 |
| UL3 | 0.704 | 0.517 | UL3 | 1.270 | 0.905 | UL3 | 0.641 | 0.920 |
| UL4 | 0.648 | 0.484 | UL4 | 0.411 | 0.603 | UL4 | 0.473 | 1.115 |
| UL5 | 0.544 | 0.484 | UL5 | 0.552 | 0.650 | UL5 | 1.041 | 0.569 |
| UR1 | 0.824 | 0.464 | UR1 | 1.038 | 0.653 | UR1 | 0.617 | 0.693 |
| UR2 | 0.600 | 0.483 | UR2 | 0.432 | 0.739 | UR2 | 0.745 | 0.888 |
| UR3 | 0.481 | 0.483 | UR3 | 0.635 | 0.673 | UR3 | 1.133 | 0.509 |
| UR4 | 0.655 | 0.567 | UR4 | 0.821 | 0.677 | UR4 | 0.557 | 1.277 |
| UR5 | 0.610 | 0.445 | UR5 | 0.862 | 0.728 | UR5 | 0.483 | 0.487 |
| Overall | 0.719 | 0.445 | | 0.855 | 0.853 | | 0.750 | 0.799 |
Overall mean of the bracket height differentials showed that indirect bonding (0.395 mm) was closer to ideal than direct bonding (0.431 mm). The differential between the techniques was statistically insignificant [Table/Fig-4a,b]. Further, indirect bonding was better on 14 out of 20 teeth (70%), though the difference was statistically insignificant for most of the teeth. When analysed on individual tooth basis bracket height measurements were significantly better with indirect bonding on LL4 (p<0.05).
Overall mean of the mesiodistal measurement differential was 0.284 mm and 0.252 mm for direct and indirect bonding group respectively [Table/Fig-5a,b]. Further, indirect bonding was better on 12 out of 20 teeth (60%), though the difference in accuracy was statistically insignificant for most of the teeth. On individual tooth basis it was found that UR3 and LL4 was more accurate in indirect bonding group than direct bonding group (p<0.05) for mesiodistal measurement.
For angular measurement, the mean difference between the direct bonding (2.884°) and indirect bonding (3.099°) was statistically insignificant [Table/Fig-6a,b]. Indirect bonding was better on 10 out of 20 teeth (50%), though difference in accuracy was statistically insignificant for most of the teeth. However, the difference was found to be statistically significant for LR4 and UR4 (p<0.05) with indirect bonding group being better.
Coefficient of variation was found to be higher for bracket height measurements (0.855 for direct and 0.853 for indirect group) followed by angulation (0.750 for direct and 0.799 for indirect bonding group) and mesiodistal position of brackets (0.719 for direct and 0.445 for indirect bonding group) [Table/Fig-7].
Discussion
The bonding of orthodontic attachments directly to the enamel is now an established procedure. The procedure can be performed in two ways with the brackets being bonded to the tooth by a direct or indirect technique.
This study aimed to improve the comparison through use of more precise measurement tools and introduce some of the latest materials and methods into the bonding process.
The present study involved multiple (five) experienced orthodontists to have a more representative sample and to reduce the systematic bias attributable to personal skill in bonding procedure unlike the study by Aguirre MJ et al., in which a single examiner performed the bonding procedure on eleven patients. Further no patient’s cooperation was needed when placing brackets on the mannequin directly in the direct bonding group [3].
Further, the study introduced some of the latest materials such as transparent tray, water soluble Glue, digital processing tools and methods into the bonding process. A transparent transfer tray ensured, the operator could visualise the brackets and ensure proper seating of tray. Use of a water soluble adhesive helped in multiple ways. As it is water soluble, so no further preparation of the brackets was needed, either in the laboratory or at chair side prior to bonding. Further, the operator could reposition any misplaced brackets with a small amount of fresh Tacky Glue.
Use of digital processing tools helped remove the manual tracing and comparing the accuracy with increase precision (lower least count). This is unlike the past studies which leverage manual tracing using a projector [4].
The study was aimed at comparing the accuracy on three dimensions – bracket height, mesiodistal placement and angular placement.
Neither of the bonding technique was significantly better (statistically significant) on any of the dimension indicating a high degree of variability across the technique.
When analysed on individual tooth basis bracket height measurements were significantly better on lower left first premolar (p<0.05) for indirect bonding group than the direct bonding group. This is in contrast to the study by Aguirre MJ et al., which showed that the direct-bonded brackets were placed closer to the ideal in the lower arch on second premolars than the indirect bonding group [3]. This can be attributed to use of transparent transfer trays providing better visibility. Additionally, the spread across five different orthodontists did help to remove the systemic bias in placement.
For Mesiodistal measurement, it was found that upper right canine and lower left first premolar was more accurate in the indirect bonding group than the direct bonding group (p<0.05). This might be due to better access and visibility offered by indirect bonding technique over the direct bonding technique. Some of the older studies did not consider the mesiodistal errors [3,13], thereby impeding any comparison. More recent studies [4], which include mesiodistal measurement found similar results with Indirect bonding resulting in better accuracy on selected teeth.
Errors in angle of placement were found to be statistically significant for lower right first premolar and upper right first premolar (p<0.05) with indirect bonding group better than the direct bonding group for the same. This might be due to better access and visibility in the indirect bonding group than direct bonding group. The above observation is in consensus with the study by Aguirre MJ et al., and Koo BC et al., which showed greater variability in angular placement of the brackets and in contrast to the study by Hodge TM et al., which found that the errors in angular placement of brackets was small [3-6].
The marginal advantage of indirect bonding over direct bonding in terms of accuracy could be a decisive factor as some studies have indicated that the difference between the two techniques in terms of bond strength, number of appointments and total treatment time is statistically insignificant [13-16].
Limitation
While an in-vitro setup helped in comparing the accuracy across the entire arch, it may not reflect the actual clinical setting; different results may be obtained with chemical-cured adhesive which has less working time, or with noncompliant patients. A more extensive randomised controlled trial covering the entire arch would help get more insights into the subject.
While it is encouraged that future studies carry the concepts of digital processing and other improvements like use of transparent tray and water-soluble glue, further studies can also benefit from a bigger sample size to reduce the standard error in the calculations.
A better measuring device and a more comprehensive research is warranted for either direct or indirect bonding technique which may also take into account the anatomic variations, overcorrections and mechanical deficiencies of the pre-adjusted orthodontic appliances.
Conclusion
Even though, at overall level indirect bonding was marginally better, statistical insignificance of the result indicates that variability was too high and the advantage wasn’t consistent. Hence the null hypothesis could not be rejected.
At the same time, on selected teeth indirect bonding did bring better results. This validates the idea the indirect bonding does offer better access to the entire arch. Choice of a bonding technique should also consider parameters like bond strength, number of appointments and total treatment time. A better measuring device and a more comprehensive research are warranted for either direct or indirect bonding technique which may also take into account the anatomic variations, overcorrections and mechanical deficiencies of the pre-adjusted orthodontic appliances.