Case Series of Peripheral Nerve Sheath Tumours: Schwannoma
Rajat Kapoor1, Bharat Rajivkumar Saxena2
1 Assistant Professor and Head, Department of Plastic and Reconstructive Surgery, Sir JJ Group of Hospitals and Grant Government Medical College, Mumbai, Maharashtra, India.
2 Senior Resident, Department of Plastic and Reconstructive Surgery, Sir JJ Group of Hospitals and Grant Government Medical College, Mumbai, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Bharat Rajivkumar Saxena, B-301, Ivy Towers, Vasant Valley, Gen A.K. Vaidya Marg, Near Dindoshibus Depot, Malad East, Mumbai, Maharashtra, India.
E-mail: bharat.saxena88@gmail.com
Schwannoma or Neurilemoma is a benign peripheral nerve sheath tumour which can affect any nerve in the body. Painless swelling or paraesthesia over the sensory distribution of the affected nerve are the usual symptoms. Audit of 12 cases operated for solitary schwannoma involving the various nerves in the extremity operated at Sir JJ group of Hospital, Mumbai from January 2013 to July 2017. Out of the 12 cases operated for solitary schwannoma 10 were males and two were females. These cases were in the age group from 28 years to 66 years. Seven cases involved the upper limb and five cases affected the lower limb. Preoperative evaluation with ultrasonography and MRI was done. Nerve preserving enucleation was done in all the cases except one which required nerve grafting. Following nerve grafting there was temporary anaesthesia over the medial thigh which recovered in three months. Postoperated neuropraxia was noted in one case which spontaneously recovered in six weeks. None of the patients had any other local or regional complications on a follow up period of 28 months. Schwannoma can be a challenging tumour because of its proximity to the nerve. At our institute immediate postoperative complication rate was 9% with no long term neurological deficit or recurrence.
Benign nerve tumours, Enucleation, Neurilemomas
Introduction
Schwannoma is a benign peripheral nerve sheath tumour which is also referred as Neurilemomas. It is a relatively rare pathology presenting as a solitary mass and practically involve any nerve in the body. These are slow growing painless swelling; hence at the time of presentation they are significantly larger in size. They may present with pain or paraesthesia in the sensory distribution of the involved nerve. Diagnosis is made with help of Ultrasonography and MRI. These patients did not have any neurological deficit besides some paraesthesia in the territory of the nerve. However, large swellings in tight fascial compartments can lead to motor deficit. Due to proximity of nerve there are significant chances of iatrogenic nerve damage. Hence, these patients can land up with permanent nerve damage which can be a devastating end result. Careful resection and preservation of the nerve is paramount. Here we are presenting an audit of 12 cases that were operated at Sir JJ Group of hospital.
Case Series
All 12 cases of schwannoma operated in our hospital since 2013 were preoperatively evaluated both clinically and radiologically. All of them had a preoperative MRI to comment upon the size and anatomical details of the tumour. MRI also gave information on the location of the nerve involved and its proximity. None of these patients had preoperative biopsy. All cases were operated under general anaesthesia with a tourniquet. Dissection in all cases was done in loupe magnification (4X). In two cases, due to extreme proximity of lesion microscope was also used (15X). Complete excision with preservation of nerve was done in all cases except for one case in which nerve graft was used. Nerve grafting was done under microscope (15X). Histopathology revealed it to be a schwannoma in all the cases. Cases where followed up for a maximum duration of 4 years and a minimum duration of 5 months; Average follow up was of 28 months.
Results
Out of the 12 cases, 10 were males, age group ranging from 28 years to 66 years with average being 38 years. Anatomical distribution of the 12 lesions is mentioned in [Table/Fig-1,2,3,4,5,6 and 7]. All these patients came with the primary complaint of painless swelling in the limb. Six patients (50%) also complained of paraesthesia over the territory of nerve distribution. The duration of symptom was variable and not only depends on the size of lesion but also on the location (sub cutaneous or muscular plane). None of these patients had any motor weakness. Two patients were operated previously in another centre and the procedure was abandoned due to non-familarity with the pathology.
Anatomical distribution of the lesions.
| Upper Limb Nerves | Lower Limb Nerves |
|---|
| Median Nerve - 2 | Sciatic Nerve - 1 |
| Ulnar Nerve - 2 | Femoral Nerve - 2 |
| Radial Nerve - 1 | Tibial Nerve - 1 |
| Superficial Radial Nerve - 2 | Saphenous Nerve - 1 |
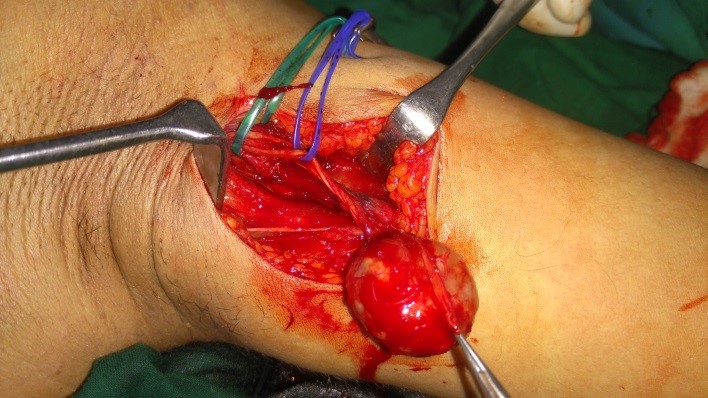
Superficial radial nerve schwannoma.

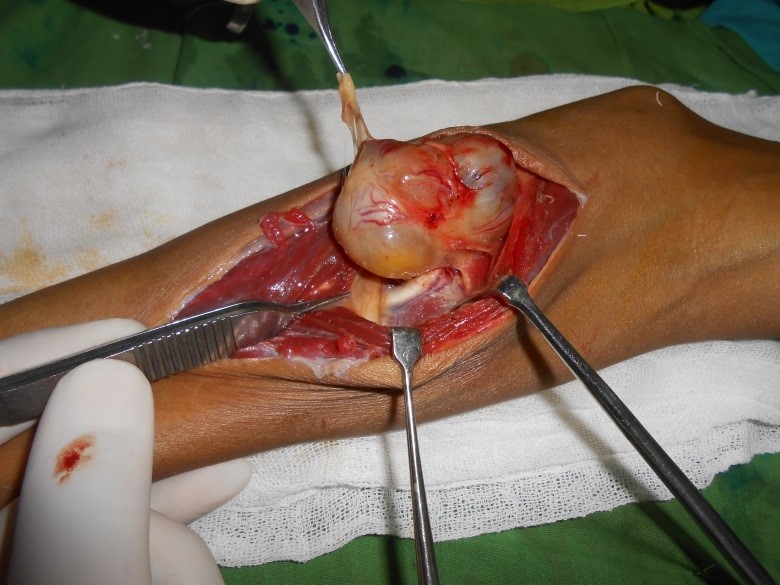

Femoral nerve schwannoma.
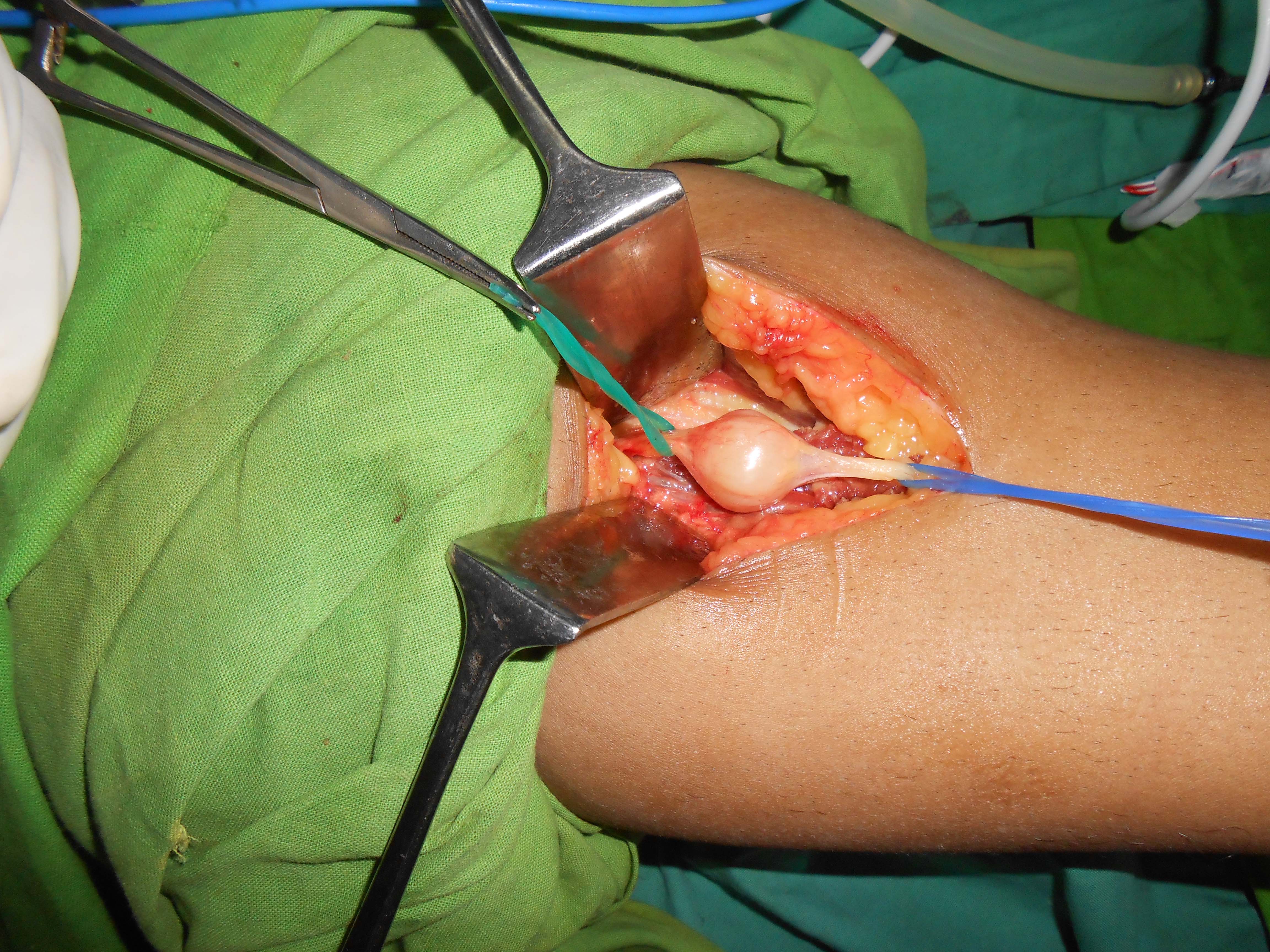

Average size of the lesion was 5.1 cm. Seven lesions were above 5 cm with largest being 8 cm (Sciatic nerve) and smallest was of 1.5cm (Superficial radial nerve) [Table/Fig-8]. The nerve was identified in the region proximal to the lesion and then traced downwards for better control. The tumour was very well encapsulated and it was possible to find a plane of dissection between the lesion and nerve. Dissection was done carefully separating the lesion from the nerve fascicle. In 11 cases it was possible to completely enucleate the tumour without excising any part of the nerve. However, in one case which involved the femoral nerve a segment of the nerve had to be excised along with the lesion and free sural nerve graft was used. Complete histopathological examination was performed in all the cases. Besides the general features of a benign tumour they showed characteristic Antony A and Antony B cells. This was clearly suggestive of Schwannoma. Postoperatively neuropraxia developed in one patient with median nerve schwanomma. However, there was complete recovery after six weeks. There was no long-term complication of recurrence of neurological deficit on follow up of 28 months. The patient with excision of lower segment of femoral nerve initially had anaesthesia of the medial thigh and leg which recovered over three months.
Size of schwannoma in upper limb and lower limb.
| Upper limb | Lower Limb |
|---|
| Largest – Median Nerve (6.5cm) | Largest – Sciatic Nerve (8cm) |
| Smallest – Superficial Radial Nerve (1.5cm) | Smallest – Saphenous Nerve (1.5cm) |
| Average – 4.7 cm | Average – 5.7 cm |
Discussion
Schwannoma is a benign, well-defined, and solitary nerve sheath tumour and accounts for 5% of all soft tissue tumours [1]. It is not only a very rare tumour, but it is often misdiagnosed due to lack of awareness and often confused with other common lesions like lipoma, fibroma of ganglion. Peripheral nerve sheath tumours comprise a spectrum of neoplastic potential ranging from benign neurofibroma and schwannoma to high-grade peripheral nerve sheath tumours. Benign nerve sheath tumours can be either neurofibroma which is associated with Von Recklinghausen disease or could be a schwannoma which are mostly solitary [2-4]. Neurofibromas are multiple, lack tumour capsule and mostly originate from terminal nerve ends. However, schwannomas are well circumscribed, encapsulated, eccentrically located and usually involving the proximal nerves [3-5]. Schwannoma tend to displace the nerve, however neurofibroma tend to grow within the nerve causing fusiform dilatation [6]. Although malignant transformation of a schwannoma is exceedingly rare, in a review by Ziadi 10 out of 32 cases might have originated from a schwannoma. However, all these 10 cases were Malignant Nerve Sheath Tumours (MNST) of cranial nerves. He thus raised the hypothesis that intracranial MNSTs might be more associated to schwannoma than their peripheral counterpart [7].
Schwannoma can practically occur in any part of the body and any peripheral nerve. We have however, demonstrated its presence in peripheral nerves of upper and lower limbs. According to Stull MA et al., schwannoma is usually found on the anterior aspect of upper limb and posterior aspect of the lower limb [8]. In our study also all lower limb schwannomas were located on the posterior aspect and in the upper limb six out of seven were located in the anterior compartment. Schwannoma usually present as slow growing painless tumour of variable size ranging from 2 cm to 20 cm [9]. However in our study the largest schwannoma was 8 cm. Schwannoma usually occurs between 20-50 years [10]. In our study the findings were somewhat similar ranging from 28 to 66 years.
Most of these tumours are ignored by the patient until they become significantly large in size or when they start compressing the nerve trunks. As the size increases the tumour can compress over the primary nerve trunk and hence causing variable symptoms. In case of extremities, painless swelling and paraesthesia were the most common symptom in our study (50%). Preoperative clinical diagnosis in these cases is difficult with differential diagnosis of fibroma, ganglioma, lipoma and xanthoma [11]. Diagnosis purely on clinical assessment can be misleading and inaccurate. Collaborating with this fact, Phalen reported accurate diagnosis of schwannoma only in 31% of upper extremity schwannoma cases [12]. Similarly, White accurately reported schwannoma in only 5 of 32 cases [13]. Preoperative sonography and MRI can be supportive for a definitive diagnosis [4]. It provides information about the size, anatomical location, relationship with other structures and malignant infiltration. In our study preoperative MRI was done in all cases with 100% accuracy. Although, preoperative imaging is not essential in every soft tissue swelling of extremity, it should be performed whenever in doubt.
Depending on the nerve of origin either they can be very superficial and easily accessible or can be deep in the intermuscular plane. Planning of the incision should be done in such a way that it is directly overlying the tumour and extending on to the uninvolved segment of the nerve. Tracing the nerve down from the virgin territory makes it possible to identify the summit between the mass and the nerve trunk. This is the point of injury in most of the cases. It is a must to operate all these cases under tourniquet because intraoperative bleeding can completely obscure the field of vision and making it almost impossible to identify the plane of dissection. We also propose use of magnification, either with help of microscope or a surgical loupe. Sometimes it may be very difficult to distinguish between the tumour and the nerve tissue. Once the right plane is identified it is possible to completely enucleate the tumour without damaging the nerve fascicles which can also be confirmed with intraoperative nerve stimulation. Schwannoma is a very well encapsulated tumour and rarely infiltrate the adjacent nerve. Hence, there is very little chances to leave behind any tumour tissue which would cause recurrence. The only case where we had to excise a nerve segment and reconstruct using a nerve graft was in a 35-year-old male having a femoral nerve schwannoma. This patient has postoperative anaesthesia over the medial thigh which recovered in three months. Postoperative neuropraxia was noted in one case involving the median nerve which recovered spontaneously in six weeks.
Conclusion
Schwannoma is a benign peripheral nerve sheath tumour which can originate from any nerve in the body. It is in close anatomical proximity to the nerve trunk without actually involving it. Use of preoperative MRI, magnification and good surgical technique will help to enucleate the tumour completely without any collateral damage or recurrence.
[1]. Kransdorf MJ, Benign soft-tissue tumors in a large referral population: distribution of specific diagnosis by age, sex, and locationAJR Am J Roentgenol 1995 164:395-402.10.2214/ajr.164.2.78399777839977 [Google Scholar] [CrossRef] [PubMed]
[2]. Lin J, Martel W, Cross-sectional imaging of peripheral nerve sheath tumors: characteristic signs on CT, MR imaging, and sonographyAJR Am J Roentgenol 2001 176:75-82.10.2214/ajr.176.1.176007511133542 [Google Scholar] [CrossRef] [PubMed]
[3]. Lee JA, Boles CA, Peripheral schwannoma lacking enhancement on MRIAJR Am J Roentgenol 2004 182:534-35.10.2214/ajr.182.2.182053414736701 [Google Scholar] [CrossRef] [PubMed]
[4]. Maraziotis T, Panagiotopoulos E, Panagiotopoulos V, Panagiotopoulos K, Neurilemoma of the popliteal fossa: report of two cases with long subclinical course and misleading presentationActa Orthop Belg 2005 71(4):496-99. [Google Scholar]
[5]. Ozdemir O, Ozsoy MH, Kurt C, Coskunol E, Calli I, Schwannomas of the hand and wrist: long-term results and review of the literatureJ Orthop Surg 2005 13:267-72.10.1177/23094990050130030916365490 [Google Scholar] [CrossRef] [PubMed]
[6]. Pino C, Ghazle H, Bhatt S, Dogra V, Schwannoma of tibial nerveJournal of Diagnostic Medical Sonography 2010 26(4):205-08.10.1177/8756479310374360 [Google Scholar] [CrossRef]
[7]. Ziadi A, Saliba I, Malignant peripheral nerve sheath tumours of intracranial nerves: A cases series reviewAuris Nasus Larynx 2010 37(5):539-45.10.1016/j.anl.2010.02.00920399579 [Google Scholar] [CrossRef] [PubMed]
[8]. Stull MA, Moser RP, Kransdorf MJ, Bogumill GP, Nelson MC, Magnetic resonance appearance of peripheral nerve sheath tumorsSkeletal Radiol 1991 20:9-14.10.1007/BF002437141900374 [Google Scholar] [CrossRef] [PubMed]
[9]. Maleux G, Byrs P, Samson I, Sciot R, Baert AL, Giant schwannoma of the lower legEur Radiol 1997 7:1031-34.10.1007/s0033000502479265669 [Google Scholar] [CrossRef] [PubMed]
[10]. Schreuder HWB, Veth RPH, Lemmens JAM, Larhooven EW, Intraosseous schwannoma (neurilemoma) of the cervical spineSarcoma 2001 5:101-03.10.1155/S1357714X0100019618521311 [Google Scholar] [CrossRef] [PubMed]
[11]. Kang HJ, Shin SJ, Kang ES, Schwannomas of the upper extremityJ Hand Surg Br 2000 25:604-07.10.1054/jhsb.2000.047211106529 [Google Scholar] [CrossRef] [PubMed]
[12]. Phalen GS, Neurilemomas of the forearm and handClin Orthop Relat Res 1976 114:219-22.10.1097/00003086-197601000-00024 [Google Scholar] [CrossRef]
[13]. White NB, Neurilemomas of the extremitiesJ Bone Joint Surg Am 1967 49:1605-10.10.2106/00004623-196749080-00013 [Google Scholar] [CrossRef]