Encountering a Rare Implant in the Hip-A Case Report
Surendra Umesh Kamath1, Monesh Kengeri Basavaraj2, Shaila Surendra Kamath3
1 Professor and Head, Department of Orthopaedics, Kasturba Medical College, Mangalore, Manipal Academy of Higher Education, Manipal, Karnataka, India.
2 Junior Resident, Department of Orthopaedics, Kasturba Medical College, Mangalore, Manipal Academy of Higher Education, Manipal, Karnataka, India.
3 Professor and Head, Department of Anaesthesiology, Kasturba Medical College, Mangalore, Manipal Academy of Higher Education, Manipal, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Surendra Umesh Kamath, Professor and Head, Department of Orthopaedics, KMC Hospital, Attavar, Mangalore-575001, Karnataka, India.
E-mail: skamath3@hotmail.com
Hip fractures are common injuries in the elderly population. Present day management is stabilisation of these fractures as early as possible. The use of internal fixation devices in the treatment of hip fractures has proved to be a major advancement in modern surgical therapy. Implants used for the fixation of hip fractures have evolved in the last two to three decades. Many complications of internal fixation have been described. Failure or complications following fixation of hip fractures include secondary osteoarthritis or avascular necrosis which may result in great disability and pain. Hip arthroplasty is a helpful reconstructive procedure in these patients who had complications following primary fixation surgery. In addition to technical problems of reconstruction in them, there may be associated difficulties of removal of metal work which has been used for previous surgeries. This is a case report of a patient who had complication following a hip fracture surgery about 33 years ago, now presented with secondary hip arthritis and a rare implant portion in situ.
Hip fractures, Osteoarthritis hip, Smith petersen nail, Total hip replacement
Case Report
A 73-year-old male patient presented to us on a wheel chair with complaints of right hip pain since eight months. Pain was located in the right hip which was insidious in onset gradually progressed over last eight months causing inability to walk.
Pain also disturbed his sleep and aggravated with hip movements. He had sustained a road traffic accident 33 years back and was diagnosed to have a hip fracture, for which he was operated and was mobilised eventually following the fracture fixation. Patient underwent another operation after one year possibly implant removal. There was no significant family and medical history. He was not on any regular medication except regular consumption of different pain killers for the hip pain. General physical and systemic examination was normal with stable vital signs.
On inspection the affected limb was externally rotated and shortened. A linear scar of about six centimetres was noted in right gluteal region healed by primary intention. On palpation there was tenderness over the anterior joint with no local rise of temperature, no swelling or deformity palpable. The greater trochanter was broadened, irregularly thickened and proximally migrated. There was adduction and external rotation deformity with painful restriction of all movements. Also, there was a true shortening of three centimetres.
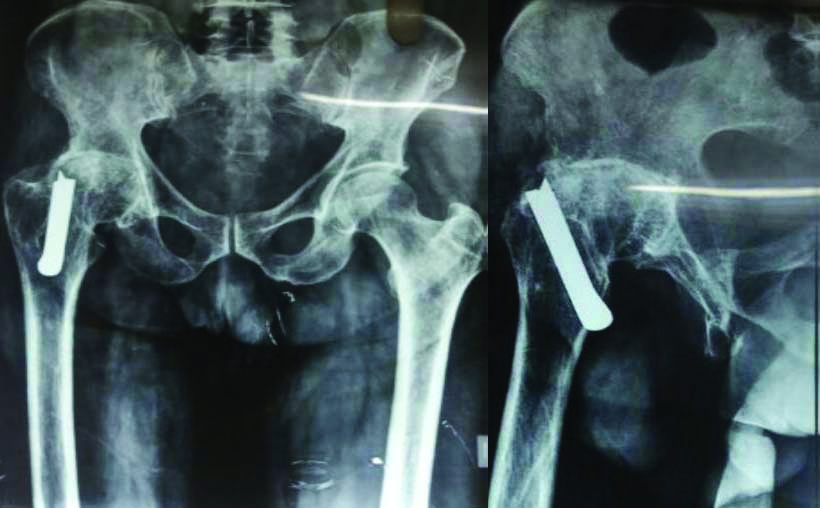
X-ray of the pelvis with bilateral hip –anteroposterior and lateral views of right hip showed reduction in the joint space with articular sclerosis with a central osteophyte with implant in the neck and trochanteric region which was suggestive of secondary osteoarthritis with Smith Peterson nail in the head and neck of femur [Table/Fig-1].
Preoperative X-rays of the pelvis anteroposterior view and lateral view with secondary degenerative osteoarthritis of hip and implant in the proximal femur.
The blood investigations revealed a normal haemogram, blood sugars, renal and hepatic function. Chest X-ray was within normal limits. Electrocardiogram and 2 D Echo was normal.
In view of his disability and symptoms we decided to treat the patient with cemented total hip arthroplasty. One of the difficulty we expected was to remove the nail in the proximal femur. We had kept all the necessary tools ready for the removal of this nail.
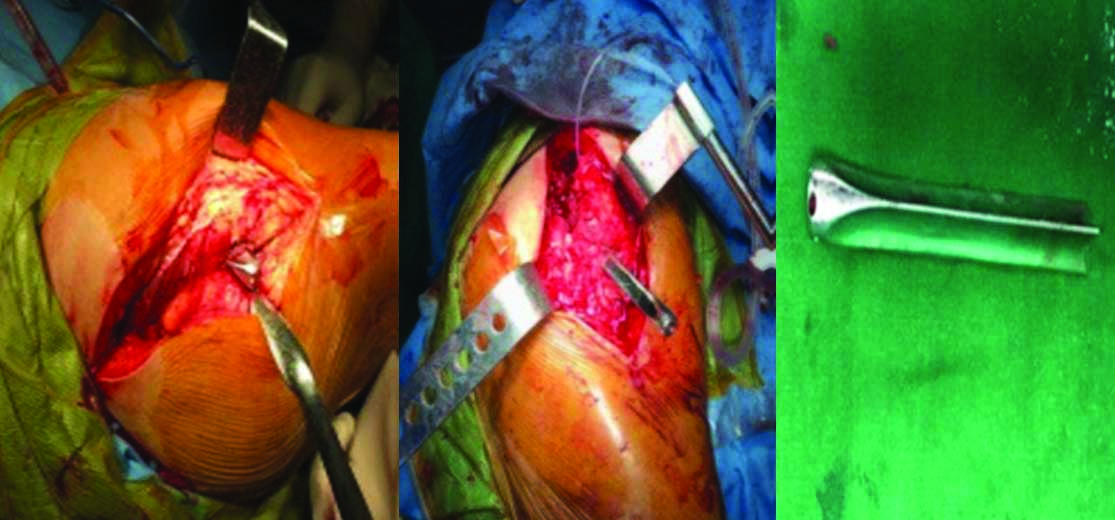
The patient was given epidural and spinal anaesthesia for the surgery. The patient was operated in the lateral position with a posterior approach [Table/Fig-2]. The nail was seen at the lateral cortex of the greater trochanter stuck inside. It was carefully separated using fine gouges and using sharp instruments. Once the implant was removed hip was dislocated posteriorly after doing a posterior capsulotomy and cutting off gemelli and pyriformis muscles. Then a cemented acetabular component was fixed. Femoral neck osteotomy was performed and cemented femoral stem was placed. Hip was reduced and found stable with good range of movements. Wound was closed in layers over a drain with absorbable sutures for muscles and fascia. Skin was closed with staples.
Showing intraoperative images of the posterior approach of hip joint and the broken part of Smith-Petersen nail.
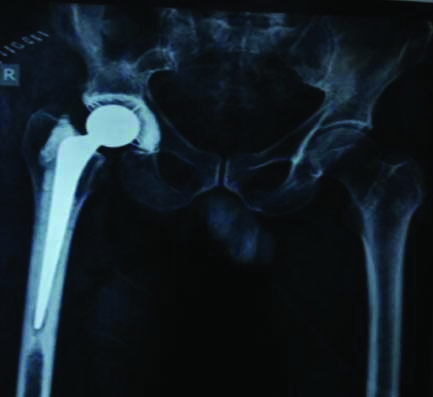
Compression dressing was applied. Postoperative period was uneventful and wound healed well. Postoperative X-rays showed well aligned acetabular and femoral components [Table/Fig-3]. Patient started full weight bearing with the help of walker comfortably on the second postoperative day. Patient got discharged on fifth postoperative day. Skin staples were removed on tenth postoperative day. Patient was followed up regularly with clinical and radiographic examination. After six weeks patient started mobilising with a walking stick. The last follow up was 18 months after the surgery.
Postoperative X-ray of the right hip anteroposterior view, showing a cemented total hip prosthesis.
Discussion
In the review of literature, many complications of internal fixation of hip fractures have been described. Functional disability and pain are the common complications following failed fixation of trochanteric fractures. Complications may be due to failure of the implant (3-12%); implant penetration (2% and 12%), nonunion (2-5%) and malunion with varus deformity (5-11%).
Failure rates as high as 56% are described in association with certain unstable fractures [1-6]. Revision surgery for the failed internal fixation of trochanteric fractures with nonunion has good results in younger patients having good bone stock [6-10]. Reconstruction with total hip arthroplasty is a good salvage procedure for elderly patients, those with poor bone stock and avascular necrosis, and those with damaged articular cartilage [7]. Many technical difficulties encountered during hip arthroplasty such as removal of implants, deformities of bone, boneloss, poor bone quality and trochanteric nonunion [11-13]. Implant removal from a united intertrochanteric fracture is not a regular procedure. It may be necessary to remove an implant in young patients or loose or painful hardware, allergy to metal, or infection. It can be a great challenge to remove the implants despite modern tools and techniques. One should anticipate great difficulties and keep all necessary tools when a secondary reconstructive procedure required in a patient with long retained metallic implants. Also, other challenges include identifying the bony landmarks due to associated deformities and addressing the bone loss.
Conclusion
Following a failure or complication of implant surgery done for hip fracture, a total hip arthroplasty is a good salvage solution for early mobilisation. There are many challenges encountered while undertaking this salvage surgery. However, one of the important challenge may be removing the metallic implants from the previous surgery before performing the total hip arthroplasty. The difficulty is more when the implants were put in decades ago, especially first generation of fixation devices for the hip like Smith Peterson nail. We present such a case with a damaged Smith Peterson nail which was implanted in the hip of a patient about 33 years ago, with secondary degenerative osteoarthritis of hip requiring a total hip arthroplasty.
[1]. Haidukewych GJ, Berry DJ, Hiparthroplasty for salvage of failed treatment of intertrochanteric hip fracturesJ BoneJoint Surg Am 2003 85-85:899-904.10.2106/00004623-200305000-0001912728042 [Google Scholar] [CrossRef] [PubMed]
[2]. Gotfried Y, Cohen B, Rotem A, Biomechanical evaluation of the percutaneous compression plating system for hipfracturesJ Orthop Trauma 2002 16:644-50.10.1097/00005131-200210000-0000612368645 [Google Scholar] [CrossRef] [PubMed]
[3]. Pachore JA, Shah VI, Sheth AN, Shah KP, Marothi DP, Puri R, Hip arthroplasty in failed intertrochanteric fractures inelderlyIndian J Orthop 2013 47:572-77.10.4103/0019-5413.12158124379462 [Google Scholar] [CrossRef] [PubMed]
[4]. Ruecker AH, Rupprecht M, Gruber M, Gebauer M, Barvencik F, Briem D, The treatment ofintertrochanteric fractures:results using an intramedullary nail with integrated cephalocervical screws and linear compressionJ OrthopTrauma 2009 23(1):22-30.10.1097/BOT.0b013e31819211b219104300 [Google Scholar] [CrossRef] [PubMed]
[5]. Noor SS, Zamir M, Najjad MKR, Total hip arthroplasty in failed hip fractures: a case seriesReconstructive Review 2015 4(4)10.15438/rr.4.4.88 [Google Scholar] [CrossRef]
[6]. Wu CC, Shih CH, Chen WJ, Tai CL, Treatment of cutout of a lag screw of a dynamic hip screw in anintertrochanteric fractureArch Orthop Trauma Surg 1998 117:193-96.10.1007/s0040200502289581243 [Google Scholar] [CrossRef] [PubMed]
[7]. Alvarez DB, Aparicio JP, Fernández EL, Múgica IG, Batalla DN, Jiménez JP, Implant breakage, a rare complication withthe Gamma nail. A review of 843 fractures of the proximal femur treated with a Gamma nailActa Orthop Belg 2004 70:435-43. [Google Scholar]
[8]. Anglen JO, Intertrochanteric osteotomy for failed internal fixation of femoral neck fractureClin Orthop Relat Res 1997 :175-82.10.1097/00003086-199708000-00027 [Google Scholar] [CrossRef]
[9]. Haentjens P, Casteleyn PP, Opdecam P, Hip arthroplasty for failed internal fixation of intertrochanteric1 and subtrochanteric fractures in the elderly patientArch Orthop Trauma Surg 1994 113:22222710.1007/BF004418377917717 [Google Scholar] [CrossRef] [PubMed]
[10]. Said GZ, Farouk O, El-Sayed A, Said HG, Salvage of failed dynamic hip screw fixation of intertrochanteric fracturesInjury 2006 37:194-202.10.1016/j.injury.2005.09.01116378609 [Google Scholar] [CrossRef] [PubMed]
[11]. Goldstein WM, Branson JJ, Modular femoral component for conversion of previous hip surgery in total hiparthroplastyOrthopedics 2005 28:1079-84. [Google Scholar]
[12]. Laffosse JM, Molinier F, Tricoire JL, Bonnevialle N, Chiron P, Puget J, Cementless modular hip arthroplasty as asalvage operation for failed internal fixation of trochanteric fractures in elderly patientsActa Orthop Belg 2007 73:729-36. [Google Scholar]
[13]. Mears DC, Durbhakula SM, Velyvis JH, Reconstructive total hip replacement after proximal femoral injuries. In: Browner BD, Jupiter JB, Levine AM, Trafton PG (Eds)Skeletal Trauma 2003 Philadelphia, PASaunders:1817 [Google Scholar]