General Anaesthesia should provide rapid smooth induction, optimal perioperative conditions and rapid recovery on discontinuation with minimal side effects [1]. Emergence from general anaesthesia implies liberation of the patient from the state of anaesthesia or as return of spontaneous breathing, voluntary reflexes and consciousness from the time general anaesthesia is turned off following the surgery [2]. Volatile anaesthetics allows rapid emergence from anaesthesia with clear headedness and this is because of low blood gas solubility and hence makes them more suitable for short and intermediate duration surgical procedures than Total Intravenous Anaesthesia (TIVA). Volatile agents like sevoflurane and desflurane are ideal agents because they have low blood gas partition coefficients 0.69 [3] and 0.42 [4] respectively and minimal effect on vital organs, better maintenance of intraoperative haemodynamics makes them more suitable for both long and short duration surgeries which help in achieving rapid emergence and recovery with clear headedness from anaesthesia.
There are many studies comparing sevoflurane & desflurane on rapid emergence and recovery from ambulatory anaesthesia [5,6] however there are only few studies [1,7-10] with conflicting results on intermediate and long duration surgeries. Our study was aimed to compare recovery profile using MAS [11-13] in immediate postoperative period in PACU following a clinical anaesthetic duration of 90-120 minutes using sevoflurane or desflurane at 1 Minimum Alveolar Concentration (MAC) and haemodynamic stability intraoperatively.
Materials and Methods
This prospective randomised study was conducted after obtaining INSTITUTIONAL ETHICAL COMMITTEE APPROVAL ref no: IEC/14/51. This study was conducted in Department of Anaesthesiology and Critical Care at Pondicherry Institute of Medical Sciences, between October 2014 and April 2016. After explaining the anaesthetic procedure, an informed and written consent was obtained from all patients on day before surgery. Sixty patients of ASA I and II belonging to age groups 18-60 years undergoing elective surgical procedures requiring endotracheal intubation were included in the study. Sample size was calculated based on a previously published clinical trial [6] comparing the effectiveness of sevoflurane and desflurane with regards to eye opening, the calculated sample size was 28 which was rounded off to 30 in each group to detect a mean difference of 5.3 minutes in MAS with 80% power, at 0.05 level of significance.
Patients were randomised by computer generated numbers into 2 groups of 30 each to receive study drug desflurane or sevoflurane accordingly. Exclusion criteria included history of any drug abuse, documented study drug allergy, cardiopulmonary, renal, hepatic, neurological, psychiatric illness, morbidly obese patients, pregnant women. A thorough pre anaesthetic assessment including detailed history, systemic and airway examination was done and routine investigations checked day prior to surgery according to the institutional protocol and all patients were kept NPO for 6 hours prior to surgery and routine aspiration prophylaxis given before the procedure.
On the day of surgery in Operating Room (OR) patients were connected to standard ASA monitors which had the respiratory gas monitoring as well. Preoperative heart rate, blood pressure, oxygen saturation were recorded continuously throughout the surgery at regular intervals along with the MAC values of volatile agents. IV access was obtained using 18 G venflon. All patients were preoxygenated with 100% oxygen till we achieved EndTidal O2 more than 95%, anti-sialagogue inj. glycopyrrolate 0.2mg iv, inj. fentanyl 2mcg/kg iv given and induced with propofol 2mg/kg iv. Once loss of eyelash reflex was observed ventilation assisted with bag and mask. Study drug desflurane 6% or sevoflurane 2% was started according to randomization grouping to all the patients according to protocol. Inj.vecuronium bromide 0.1mg/kg iv given to facilitate the tracheal intubation with appropriate size ET tube.
Anaesthesia was maintained with sevoflurane 2% or desflurane 6% along with 50% Nitrous oxide in Oxygen (3lit : 3lit) to attain 1 MAC. After attaining 1 MAC the fresh gas flows decreased to 1 litre (Oxygen: Nitrous oxide; 0.5lit: 0.5lit), test drug was reduced to lowest concentrations possible to maintain 1 MAC throughout the procedure from the time of induction till the end of last suture to maintain depth of anaesthesia. Intraoperatively muscle relaxants were given at regular time intervals to continue muscle paralysis with one twitch of Train of Four (TOF) monitoring. Any increase in Heart Rate (HR), Systolic Blood Pressure (SBP), Diastolic Blood Pressure (DBP) by more than 20% from the baseline was treated with Inj.fentanyl 25 mcg iv bolus. At the end of the procedure, all patients received inj. paracetamol 1gm iv and inj. ondansetron 0.01mg/kg iv. Test drug and nitrous oxide were stopped once last sutures were applied, 100% oxygen was provided, neuromuscular block was reversed using inj. neostigmine 0.05mg/kg iv and inj.glycopyrrolate 0.01mg/kg iv, when patient starts spontaneous breathing time taken for spontaneous eye opening on verbal commands was noted on operating table from the time study drug was stopped and patients were extubated while fully conscious, obeying commands.
Patients were shifted to PACU, assessed for immediate recovery with the help of MAS at 0 minute, every minute for the first 5 minutes and every 5 minutes interval thereafter till a median score of 10 was achieved as standard of recovery from anaesthesia. All patients were observed for symptoms like perioperative desaturation, coughing, bronchospasm or laryngospasm during induction or extubation, Postoperative Nausea and Vomiting (PONV) and others if any.
Statistical Analysis
The statistical test used was unpaired student’s t-test for age and weight, qualitative data like ASA grading, sex of the patient were compared using chi-square test, haemodynamic parameters such as mean heart rate, blood pressure both systolic and diastolic, was compared using analysis of variance (ANOVA). Time taken for spontaneous eye opening was analysed using unpaired student’s t-test; MAS was compared using Mann Whitney u-test. All the data was analysed using SPSS package (version 21.0 SPSS INC., Chicago, IL, USA) software for windows, the study parameters were expressed in Mean±SD and Median wherever applicable. In all the parameters, p<0.05 was considered to be significant.
Results
All 60 patients involved in the study completed assessment as of protocol. The demographic profiles were comparable between the groups and were not statistically significant [Table/Fig-1].
| Parameter | Sevoflurane | Desflurane | p-value |
|---|
| Age (Years) | 30.07±8.886 | 34.40±11.581 | 0.110 (NS) |
| Sex (M/F) | 22/8 | 18/12 | 0.273 (NS) |
| Weight (Kgs) | 61.77±10.170 | 59.0±7.961 | 0.246 (NS) |
| ASA grading (I/II) | 29/1 | 29/2 | 1.000 (NS) |
| Type of Surgeries |
| Plastic surgery | 18 | 15 | |
| ENT surgery | 10 | 13 | |
| General surgery | 2 | 2 | |
| Duration of Anaesthesia (Minutes) | 92.67±28.062 | 92.83±25.820 | 0.981 (NS) |
(p-value <0.05 is significant; NS: Non Significant)
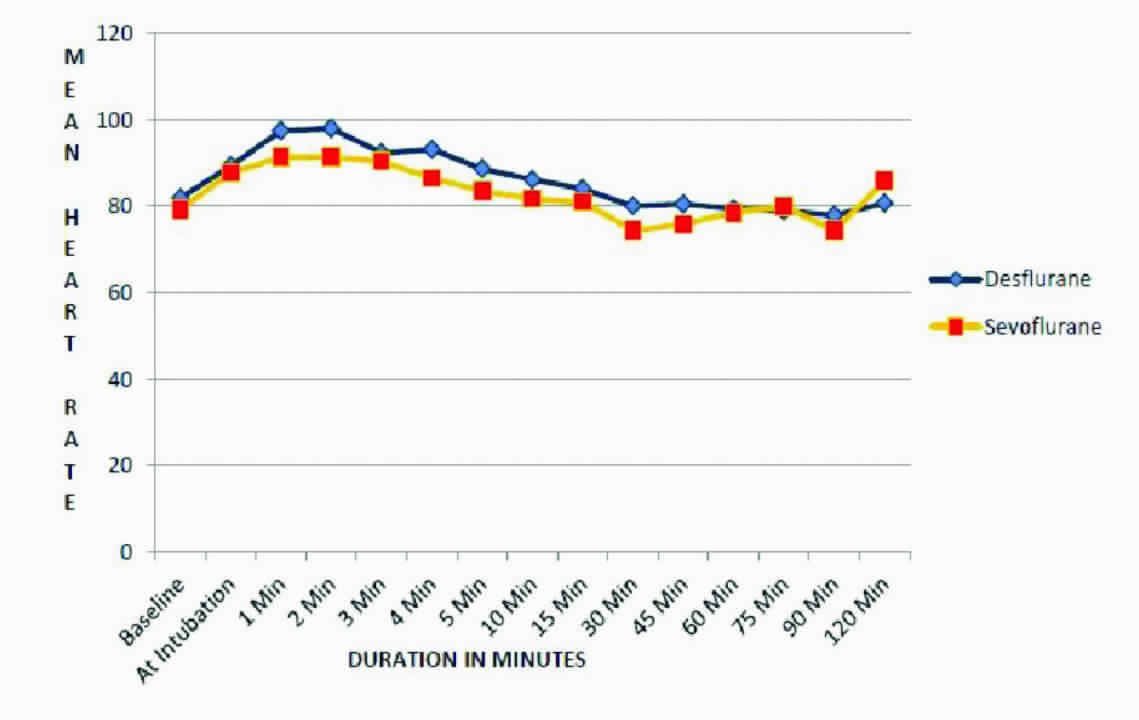
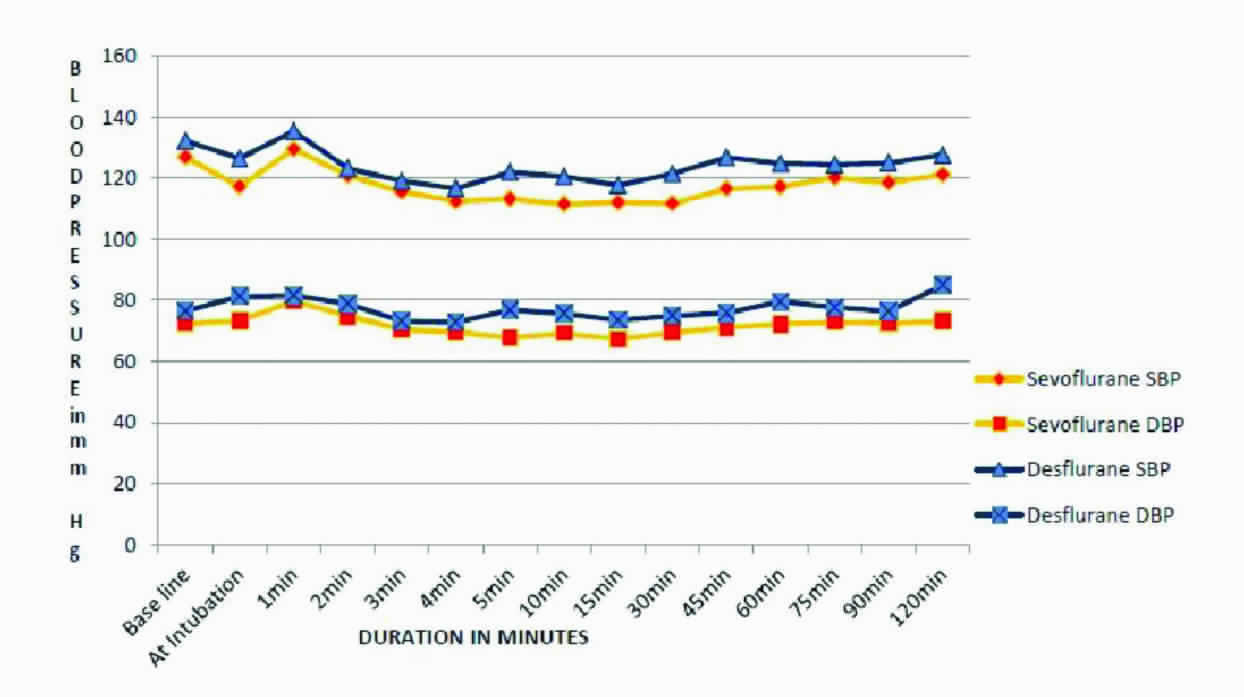
Intraoperative haemodynamic parameters like mean heart rate [Table/Fig-2], systolic blood pressures and diastolic blood pressures did not differ between groups during the procedure apart from the pressor responses during intubation, extubation and were within 20% of baseline values in both groups [Table/Fig-3].
Mean systolic and diastolic blood pressures.
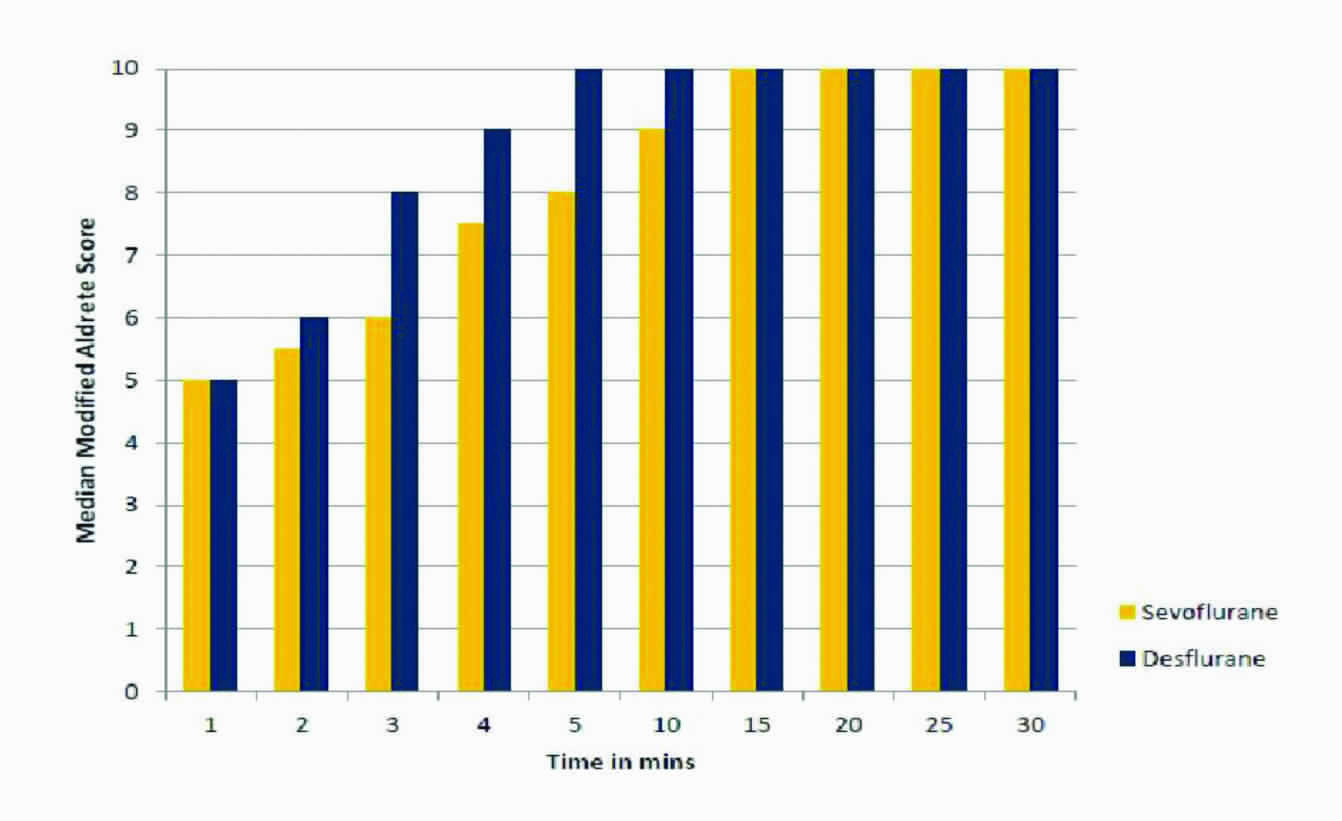
Once last sutures were applied, volatile anaesthetic was stopped, mean duration for spontaneous eye opening time on verbal commands was 8.96±1.58 minutes for sevoflurane, 5.17±1.48 minutes for desflurane with a mean difference of 3.79±0.1minutes, between the study groups and it was significant in desflurane group both clinically and statistically p<0.001 with 95% Confidence interval 3.7 (2.703 to 4.953) [Table/Fig-4]. Immediate recovery was assessed by MAS after shifting the patients to PACU where median score 10 was taken as end point of recovery. At 1 minute it was statistically insignificant (p>0.05) between the groups [Table/Fig-4], a median score of 10 was attained at 5 minutes by desflurane, 15 minutes in sevoflurane groups and it was statistically significant p<0.001 [Table/Fig-5].
| Sevoflurane | Desflurane | p-value |
|---|
| Spontaneous eye opening (in mins) | 8.96±1.58 | 5.17±1.48 | <0.001† |
| Modified Aldrete Score |
| At Arrival in PACU | 5.00 | 5.00 | 0.640 |
| After 5 minutes | 8.00 | 10.00 | 0.000* |
| After 10 minutes | 9.00 | 10.00 | 0.000* |
| After 15 minutes | 10.00 | 10.00 | 0.005* |
(†p<0.001 is strongly significant; *p<0.05was taken significant)
Median modified aldrete score.
None of the patients had adverse effects like perioperative desaturation, PONV, coughing, bronchospasm or laryngospasm during induction or extubation and there was also no requirement of additional fentanyl intraoperatively in both the groups.
Discussion
The complete return of complex physiological functions after general anaesthesia within a short duration with reliable recovery has become more important for conduct of anaesthesia. Volatile agents are preferable in any age group for surgical anaesthesia compared to Total Intravenous Anaesthesia (TIVA), they are ideal for maintenance of anaesthesia because they are effective, reliable, safe, easy to deliver, stable, without any major end-organ sequelae. Both sevoflurane and desflurane have a pharmacokinetic profile that results in relatively rapid emergence from anaesthesia because of relatively low blood: gas and fat: blood partition coefficients [14,15]. There are studies carried out in wide variety of population, that demonstrated early recovery with desflurane [7] compared to sevoflurane [8,9] in adult patients undergoing ambulatory surgeries, recovery endpoints such as time to eye opening on verbal commands and regaining orientation were found to be significantly faster with desflurane [6].
In present study, we compared the time taken for spontaneous eye opening on verbal commands and quality of immediate recovery from anaesthesia in PACU by using MAS following general anaesthesia with sevoflurane or desflurane for a mean intermediate duration of 92.75±26.941minutes. The time taken for spontaneous eye opening was 5.17±1.48 minutes after desflurane and 8.96±1.58 minutes after sevoflurane anaesthesia respectively. Recovery from anaesthesia was faster in desflurane group and statistically significant, which is comparable to a study conducted by Jindal R et al., in the case of gynaecological surgeries and reported that time to spontaneous eye opening on verbal commands was shorter in patients who received desflurane (4.18±1.548 minutes) than sevoflurane (6.80±2.259 minutes) with mean duration of anaesthesia 53.16±12.016 minutes [16].
MAS scoring system [11-13] is commonly used as a guide to determine discharge of the patients from the PACU to either postsurgical ward or in case of ambulatory surgeries, for discharge to home. Dupont J et al., used MAS to assess the recovery and reported that desflurane group has significantly faster recovery compared to sevoflurane group [17]. Similarly, Song D et al., recorded wake-up times and the MAS, when patients were anaesthetised with propofol, desflurane, and sevoflurane, in patients undergoing ambulatory anaesthesia and they found desflurane achieved MAS of 8 faster than other study drugs [5]. Similarly in our study though the initial MAS was similar in both the study groups, median score of 10 was achieved by desflurane in 5 minutes whereas it took 15 minutes for sevoflurane in PACU [Table/Fig-5]. This prolonged effect of sevoflurane was considered probably due to hexafluoroisopropanol from sevoflurane accounting to slower recovery as described by Dupont J et al., [17]. In addition it could also be due to sevoflurane degradation to compound-A and irreversible binding to body proteins reporting the delayed awakening after sevoflurane anaesthesia compared to desflurane Eger et al., study supports this finding [10].
In this study, there was no change in systolic and diastolic blood pressures and it was within 20% of baseline, however mean HR was relatively higher in desflurane group than sevoflurane but within ±20% of baseline throughout the intraoperative period and there was no requirement of additional fentanyl intraoperatively. This is comparable to the study conducted by Kaur A et al., in laparoscopic bariatric surgeries, comparing sevoflurane and desflurane on haemodynamic variables and emergence characteristics; they observed SBP, DBP, MAP and HR did not differ between the two groups and emergence was faster in desflurane [18]. The increase in HR in desflurane group in our study could probably be due to β-adrenergic activation induced by desflurane which is mediated by release of plasma adrenaline and noradrenaline as described by Weiskopf RB et al., [19].
There were no incidences of perioperative desaturation, coughing, bronchospasm or laryngospasm during induction or extubation and PONV in both the groups. Wallenborn J et al., showed that incidence of PONV is roughly around 10% for inhalational agents but none of the patients showed PONV which could probably be because of propofol which is used as an induction agent and inj.ondansetron given iv to all patients before extubation [20].
Conclusion
It was concluded that desflurane had significant faster emergence and early recovery with clear headedness when compared to sevoflurane, in intermediate duration surgeries lasting less than 120 minutes. Both desflurane and sevoflurane had similar kind of haemodynamic profile, without any adverse effects during perioperative period while using these volatiles as primary anaesthetics for maintenance of anaesthesia.
(p-value <0.05 is significant; NS: Non Significant)
(†p<0.001 is strongly significant; *p<0.05was taken significant)