Vaccine is an immune-biological substance which helps to provide protection against given disease and also stimulates the production of antibodies [1,2]. Despite the availability of vaccines, it is estimated that, around three million children die every year globally by vaccine preventable diseases. Vaccination coverage is one of the most important strategies adopted by child survival program throughout the world [3].
Various studies showed that, the reasons for immunization dropout were inadequate vaccine supply in the hospitals, lack of mother’s knowledge about immunization benefits, routine immunization schedule, the number of doses required and also have the belief that too many vaccines can be harmful to the child, unawareness on the need for immunization and return for the next dose and lack of faith in immunization among mothers [4,5].
National Family Health Survey-4 (NFHS-4) reveals that among the children aged between 12-23 months, the percentage of children were fully immunized against BCG, Measles and 3 doses each of Polio and DPT in rural India is 61.3%, in Karnataka state 64.8% and in Udupi district (where the study has been conducted) is 64.6% respectively [6]. So the need for this study is to assess the immunization coverage and to identify the perceived maternal barriers for immunization among mothers of under five children in selected rural areas of Udupi district.
Materials and Methods
A quantitative approach with descriptive survey design was used to collect the data. A total of 310 mothers of under five children were enrolled in the study over one-month period from January 2017 to February 2017.
Sample size calculation was done based on the data obtained from Pilot study by using estimation of proportion formula. In the present study, 310 samples were included to fulfill the objectives.
The study was conducted in four PHC’s (Kolalagiri, Mudarangadi, Byndooru and Bylooru) of Udupi district by adopting simple random sampling method. From the PHC’s, 22 villages were selected by using convenient sampling method and participants who met the inclusion criteria (n=310) were recruited by using non-probability purposive sampling technique.
Formal administrative permission was obtained from the Institutional Ethical Clearance Committee, District Health Officer of Udupi District and Medical officers of respective PHC’s and registered in CTRI (Reg No: CTRI/2017/07/009130). A duly explained, written consent, translated by trained personnel in to local language (Kannada) was taken from all the mothers before including them in the study.
Data were collected by using structured questionnaires which includes demographic proforma, common health problems of immunized under five children and five-point Likert scale to assess barriers for immunization and information regarding the immunization status of children was verified against immunization card of respected children to confirm appropriate date of vaccination.
Statistical Analysis
Data analysis was done using SPSS 16.0 version. The analysis was done by using descriptive statistics which includes frequency and percentage, mean, median and standard deviation.
Results
The demographic variables were computed by using Frequency and Percentage for describing the sample characteristics. The data presented in the [Table/Fig-1] shows that, with regard to age, the maximum percentage of the mothers 157 (50.6%) belonged to the age group of 26-30 years. Data on the education of mother showed 108 (34.8%) had secondary school education. Concerning the number of children in the family, data showed 172 (55.5%) mothers had two children and 82 (26.5%) children were less than six months of age, data on type of family showed 174(56%) mothers belonged to joint family, 233(75.2%) mothers were homemakers, 267(86.1%) belonged to Hindu religion, 183(59%) mothers belonged to below poverty level, 307(99%) mothers had taken children for immunization according to the age of the child, 230(74.2%) mothers had taken their child to Primary Health Care center for immunization and 200(64.5%) mothers were not aware on due vaccine of their child according to the age.
Frequency and percentage distribution for describing the sample characteristics.
| Sample characteristics | Frequency (%) |
|---|
| Age of the mother21-2526-3031-3536-4041-45 | 24 (7.7%)157(50.6%)91(29.4%)31(10%)7(2.3%) |
| Education of the motherPrimarySecondaryHigher secondaryPUCGraduatePost graduate | 106(34.2%)108(34.8%)39(12.6%)14(4.5%)39(12.6%)4(1.3%) |
| Number of Children1234 | 128(41.3%)172(55.5%)9(2.9%)1(0.3%) |
| Type of familyJointnuclear | 174(56%)136(44%) |
| Age of the child (in months)0-67-1213-1819-2425-3637-4849-60 | 82(26.5%)43(13.8%)13(4.2%)15(4.8%)58(18.7%)68(21.9%)32(10.1%) |
| Status of the EmploymentHome makersSkilled workersUnskilled workers | 233(75.2%)38(12.2%)39(12.6%) |
| ReligionHinduMuslimChristian | 267(86.1%)26(8.4%)17(5.5%) |
| Socioeconomic Status (based on the colour of ration card of the mothers)Above poverty level(APL card)Below poverty level(BPL card) | 127(41%)183(59%) |
| Given immunization according the age of the childYesno | 307(99%)3(1%) |
| Setting of ImmunizationAnganwadiSub centerPrimary health centerCommunity health centerGovernment hospitalPrivate hospital | 14(4.5%)5(1.6%)230(74.2%)13(4.2%)21(6.8%)27(8.7%) |
| Awareness on due vaccine of the childAware about the due vaccineNot aware about the due vaccine | 110(35.5%)200(64.5%) |
The data presented in [Table/Fig-2] show that among 310 children, 309 (99.7%) children had received OPV at birth, 309 (99.7%) had received BCG vaccine within one month after birth, 279 (90.0%), had received Hepatitis B vaccine within 24 hours of birth on scheduled date. Data also shows that among 310 children 305 (98.4%) children had received Penta vaccine (DPT, Hepatitis B, Hib) (first dose) and 305 (98.4%) had received OPV (first dose) at six weeks on scheduled date. Data presents that, among 286 children, 282 (98.6%) children had received Penta vaccine (DPT, Hepatitis B, Hib) (second dose) and 282 (98.6%) had received OPV (second dose) at ten weeks on scheduled date. As per the data, among 249 children 242 (97.2%) children had received Penta (DPT, Hepatitis B, Hib) (third dose), 242 (97.2%) had received OPV (third dose) and among 93 children 82 (88.2%) had received IPV at 14 weeks on scheduled date. Among 218 children 210 (96.3%) children had received measles and 210 (96.3%) had received Vitamin A (first dose) at nine months on scheduled date.
Frequency and percentage distribution of immunization compliance of zero to one-year age group children based on national immunization schedule in selected rural areas of Udupi district.
| Name of thevaccine | Age of the child | Given on scheduled date | Not given on scheduled date | Not given |
|---|
| Frequency (%) | Frequency (%) | Frequency |
|---|
| OPV(0dose)(n=310) | Within 15 days after birth | 309 (99.7%) | 1 (0.3%) | - |
| BCG(n=310) | Within 1 month after birth | 309 (99.7%) | 1 (0.3%) | - |
| Hep B(n=310) | Within 24 hours after birth | 279 (90.0%) | 31 (10.0%) | - |
| Penta (1) (DPT, Hep B, Hib)(n=310) | 6 weeks | 305 (98.4%) | 5 (1.6%) | - |
| OPV (1)(n=310) | 6 weeks | 305 (98.4%) | 5 (1.6%) | - |
| Penta (2)(DPT Hep B, Hib)(n=286) | 10 weeks | 282 (98.6%) | 4 (1.4%) | - |
| OPV (2)(n=286) | 10 weeks | 282 (98.6%) | 4 (1.4%) | - |
| Penta (3)DPT,Hep B, Hib(n=249) | 14 weeks | 242 (97.2%) | 6 (2.4%) | 1 (0.4%) |
| OPV (3)(n=249) | 14 weeks | 242 (97.2%) | 6 (2.4%) | 1 (0.4%) |
| IPV(n=93) | 14 weeks | 82 (88.2%) | 10 (10.8%) | 1 (1.1%) |
| Measles(n=218) | 9 months | 210 (96.3%) | 7 (3.2%) | 1 (0.5%) |
| Vitamin A (1)(n=218) | 9 months | 210 (96.3%) | 7 (3.2%) | 1 (0.5%) |
The data in [Table/Fig-3] shows that, among 162 children 146 (90.1%) had received measles (second dose) at 16-24 months on scheduled date. Data showed that among 175 children 169 (96.6%) had received DPT booster (first dose), among 161 children 153 (95.0%) had received OPV booster and 169 (98.2%) children had received vitamin A (second dose) at 16-24 months on scheduled date. Data presents that among 11 children, six (54.5%) had not taken DPT booster at five years. The reasons for dropout of measles (second dose) and DPT boosters were illness of children, lack of awareness and knowledge on due vaccine by mothers.
Frequency and percentage distribution of immunization compliance of children aged between 2 to 5 years based on national immunization schedule in selected rural areas of Udupi district.
| Name of the vaccine | Age of the child | Given on scheduled date | Not given on scheduled date | Not given |
|---|
| Frequency(%) | Frequency(%) | Frequency(%) |
|---|
| Measles (2)(n=162) | 16-24 months | 146 (90.1%) | 3 (1.9%) | 13 (8.0%) |
| DPT booster (1)(n=175) | 16-24 months | 169 (96.6%) | 4 (2.3%) | 2 (1.1%) |
| OPV booster(n=161) | 16-24 months | 153 (95.0%) | 5 (3.1%) | 3 (1.9%) |
| Vitamin A (2)(n=169) | 16-24 months | 166 (98.2%) | 3 (1.8%) | - |
| DPT booster (2)(n=11) | 5 to 6 years | 5 (45.5%) | - | 6 (54.5%) |
Data in [Table/Fig-4] represents the barriers for immunization among mothers of under five children. The perceived barriers for immunization were classified into three i.e., Personal barriers, barriers related to knowledge and barriers related to organization. The Mean score of personal barriers was 28.24%, barriers related to knowledge was 34.34% and barriers related to an organization was 21.07% which indicates that noncompliance of childhood immunization depends upon knowledge of the mothers and organizational factors. The barriers related to knowledge includes: lack of awareness on vaccine preventable diseases, lack of awareness on the importance of vaccines, lack of awareness on immunization schedule as per the age of the child etc. Barriers associated with organization includes: long distance to the clinic, shortage of vaccine supply, and lack of information on when to return for the next dose. Data also showed that Median score on perceived maternal barriers was obtained to the participants were 88 with the standard deviation of 9.76.
Barriers for immunization among mothers of under five children.
| Barriers | Maximum Possible Score | Mean | Median | IQR | SD |
|---|
| Personal Barriers | 30 | 28.24 | 88.00 | 85-88 | 9.76 |
| Barriers related to Knowledge | 40 | 34.34 |
| Barriers related to organization | 30 | 21.07 |
| Total | 100 | 83.65 |
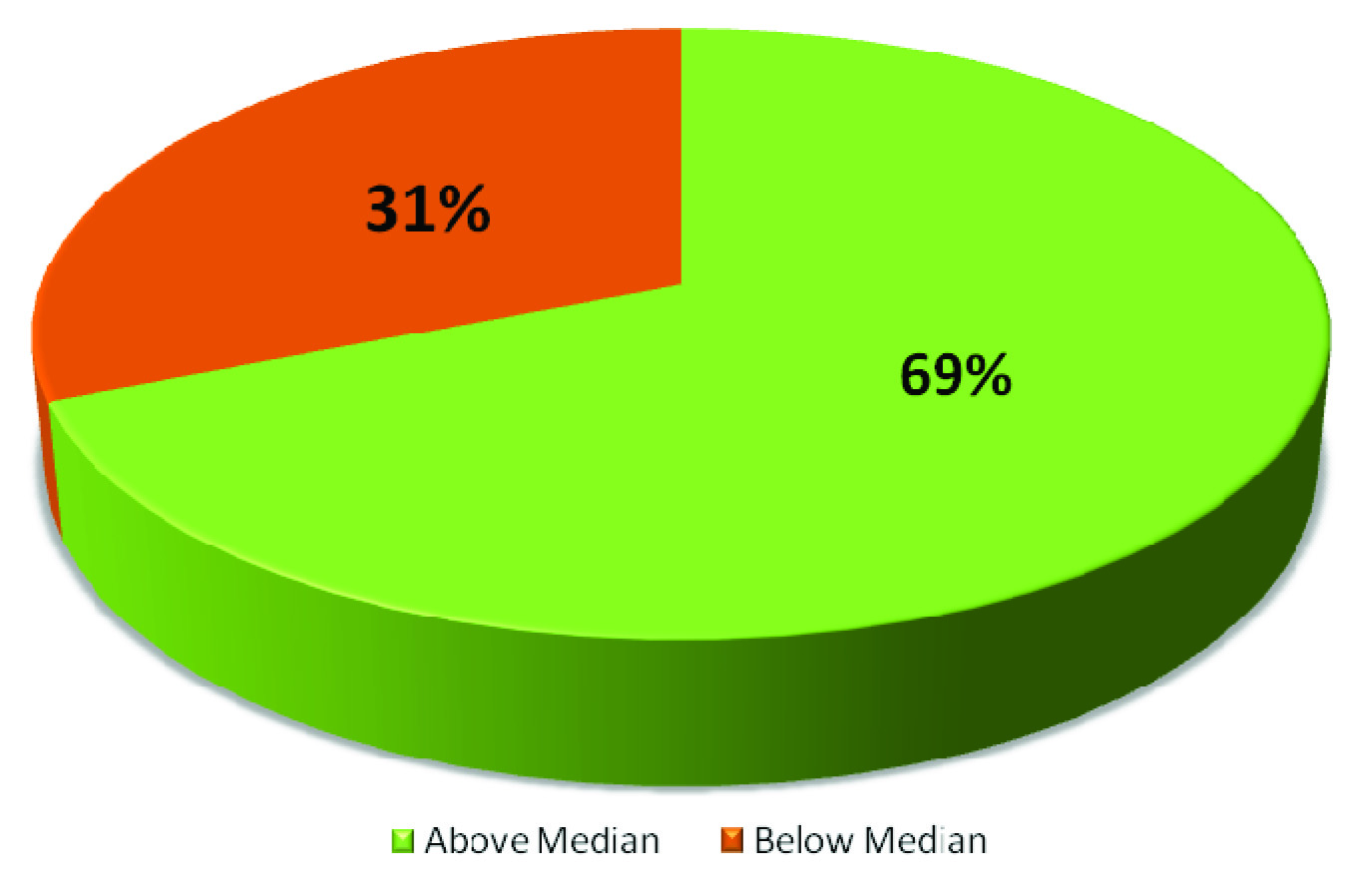
According to the data: above the median lesser the barriers. As per the data, maximum 214(69%) mothers were not having any barriers and 96(31%) were having barriers for immunization including Personal Barriers, Barriers related to knowledge and barriers related to organization for immunization [Table/Fig-5].
Pie diagram showing percentage distribution of mothers based on median scores on maternal barriers for immunization.
Discussion
Sample Characteristics
The study results showed that, with regard to religion, around 267(86.1%) mothers were Hindus and 307 (99%) mothers reported that they had taken children for immunization according to the age of the child. One similar study was done in Mysore to assess the immunization compliance of under five children. The result of the study with respect to sample characteristics shows that, 78% of parents were Hindus and 29.1% of mothers reported complete vaccination of their children [7]. The study findings were supported by a survey conducted in Udupi district Karnataka by Susan C et al., to compare the awareness on Vitamin A supplementation among 200 mothers residing in Urban and rural areas of study setting. Ten urban and rural areas were selected by using simple random sampling technique [8]. The result showed that awareness on Vitamin A prophylaxis was found more among mothers residing in the rural area (52.66%) than in the urban area (46%).
Immunization Compliance
The present study revealed that, among 218 children, 210(96.3%) children had received measles vaccine and 210(96.3%) had received Vitamin A prophylaxis (first dose) at nine months on scheduled date. As per the data among 162 children 146(90.1%) had received measles vaccine (second dose) at 16-24 months on scheduled date. Among 129 children 100% of them had received Vitamin A (third dose) at 30 months on scheduled date. Similar to that of present study findings a study was conducted by Karinagannanavar A et al., in Bellary district [9]. In their study, out of 1007 children, 69.4% were vaccinated and 30.6% were unvaccinated against measles and 53.6% children receive where as 46.4% did not receive Vitamin A Prophylaxis.
The present study showed that, among 310 children, 99 (31.9%) had fever, 16 (5.2%) children had swelling, 24 (7.7%) had ear pain and two (0.6%) of them had pain after the administration of Penta Vaccine. A similar study was conducted by Carvajal A et al., to assess the adverse events followed by the administration of influenza vaccine. The result showed that, out of 507 vaccinated subjects 103 (20.3%) had developed some complications like reaction at the site of injection, cough, respiratory disorder, fever and joint pain [10]. Results of the study was supported by a study conducted by Habibullah & Ashraf with the aim to assess vaccination coverage of Hepatitis B vaccine (Pentavalent vaccine) among under five children, who were attending the public sector hospitals Karachi, India for health visits. The study comprised of 969 children, among them 97% received BCG vaccine at birth. The children who had received first dose of Hepatitis B were 48% and the children who received all the doses of Hepatitis B were 65% and 50% of them had received measles vaccine first dose. As per the obtained data, reasons for non-compliance were family objection (18%), illness of the children (15%) and lack of knowledge and long distance to the hospital (6%). The study concluded that, public education to remove the misconception about vaccination helps to improve vaccine coverage among children [11].
Perceived Maternal Barriers
The present study shows that majority 69%(214) of the mothers were not having any barriers including personal Barriers, barriers related to knowledge and barriers related to organization for immunization and 31%(96) were having barriers for immunization. The reasons for incomplete immunization in the study region were mainly associated with mother’s knowledge on vaccines and immunization. Similar to that a study was conducted in Karachi, to assess the current status of immunization of children aged between 12-23 months and factors affecting it. As per the data, dropout rate was highest among measles (30%) and third dose of DPT vaccine (27%) were more common. The reasons for vaccine dropout were; illness of children, lack of information about the actual date of immunization, and benefits of vaccine, which are reported by the mothers [12]. The result of the present study was supported by a cross-sectional survey conducted in Mangalore city, Karnataka to assess the knowledge, attitude and perception of mothers of under five children about vaccination who were attending to urban health center. The study recruited 74 participants from urban setup and 126 from rural area. The results revealed that knowledge on immunization were significantly higher in urban mothers (75.6%) compared to rural mothers (62.69%). The data also showed that 89.2% of mothers of urban and 55.6% mothers from rural area had favorable attitude towards childhood immunization [13].
Limitation
The study was limited to under five children who were belonging to the selected rural areas of Udupi district. So, the generalization of the study can be done only to the similar kind of population.
Conclusion
Vaccination against childhood communicable diseases through expanded immunization programme is one of the best cost effective public interventions available in India. The district Health care workers of Udupi District, functioning effectively in implementing childhood immunization programme and also rural community are reinforced for the effective implementation of immunization programme. The immunization compliance of all the vaccines was above 90% according to the study results.
The reason for incomplete childhood immunization were identified mainly associated with maternal knowledge on immunization which includes; lack of information about all vaccines, adverse events of vaccines, lack of knowledge on due vaccine, issues of child’s safety, lack of knowledge on immunization day etc. The result also showed that, there is a need for enforcing maternal knowledge on immunization. Thus, the present study concluded that as maternal knowledge on immunization has an influence on childhood vaccination, therefore a positive reinforcement and timely health education regarding vaccines are important by health care professionals to reduce immunization dropout of children.