Fabrication of Conventional Complete Denture in Resorbed Mandibular Ridge with Deficient Keratinized Mucosa Using Free Gingival Graft
Monika Malik Vigarniya1, Shagun Gulia2, Vidushi Sheokand3, Nupur Dabas4
1 Senior Resident, Department of Dentistry, Shaheed Hasan Khan Mewati, Government Medical College, Gurgaon, Haryana, India
2 Assistant Professor, Department of Prosthodontics, Shree Guru Gobind Singh Tricentenary University, Gurgaon, Haryana, India.
3 Assistant Professor, Department of Periodontics, Shree Guru Gobind Singh Tricentenary University, Gurgaon, Haryana, India.
4 Assistant Professor, Department of Prosthodontics, Shree Guru Gobind Singh Tricentenary University, Gurgaon, Haryana, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Monika Malik Vigarniya, G-27, First Floor, Sushantlok-II, Sector-57 Gurgaon-122002, Haryana, India.
E-mail: drmonika461@gmail.com
Long standing edentulism often results in dimensional changes in the bone as well as in the soft tissue. The severity of these changes depends upon the span of edentulism, systemic and oral well-being of the patient. Complete denture prosthesis rests on the basal seat area that primarily consists of oral mucosa and residual alveolar ridge. The oral mucosa underneath the denture has unique characteristic of being displaceable and compressible. This factor was described by Hanau as ‘resiliency and like effect’, Realeff Effect that plays an important role in all the steps of compete denture fabrication. In a case of extreme bone resorption, the bone and mucosa both diminishes with time. The reduced thickness of keratinized mucosa make denture bearing area more prone to trauma. This article describes a simple pre-prosthetic surgical technique for soft tissue augmentation in rehabilitation of extremely resorbed mandibular ridge with deficient mucosa to improve support for complete denture.
Alveolar ridge augmentation, Free gingival graft, Mandibular ridge resorption, Tissue augmentation
Case Report
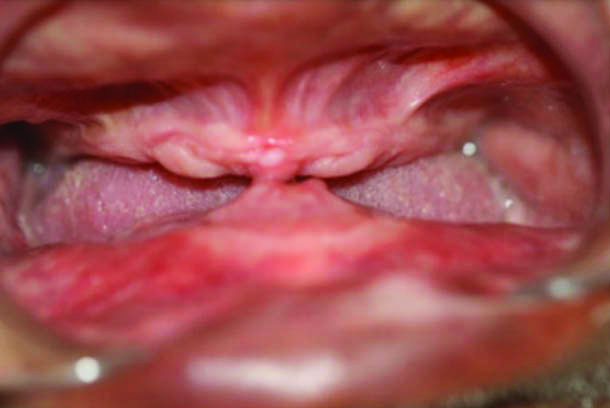
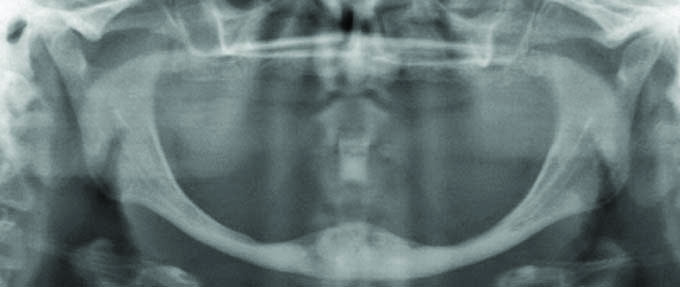
A 53-year-old male patient came to the Department of Prosthodontics, with complaint of impairment of his masticatory function due to unstable mandibular complete denture. The examination revealed that mandibular ridge was compromised with no hypermobile tissue in anterior part [Table/Fig-1]. Radiographically it showed that this is a case class VI mandibular atrophy according to Cawood and Howell classification [Table/Fig-2].
Preoperative intra oral view of Maxillary and Mandibular edentulous ridges.
Digital OPG shows mandibular atrophy class VI (Cawood & Howell classification).
The patient was already a conventional denture wearer and was not ready to undergo an extensive surgically invasive treatment. The main concern of the patient was excessive pressure that he feels on the anterior mandibular region with continuous trauma and ulcers from denture use. The treatment plan opted for this patient was to increase the width of keratinized mucosa at the deficient site using free gingival graft to provide an increased stable basal area for a new conventional denture.
Clinical Procedure: The proposed treatment plan consisted of 3 steps: 1) Surgical part where a free gingival graft harvested from crest of maxillary ridge was grafted on mandibular anterior ridge to increase thickness of keratinized mucosa; 2) Rest period of one month was advised to ensure complete healing of connective tissue; and 3) Fabrication of conventional complete denture using muco-selective impression technique.
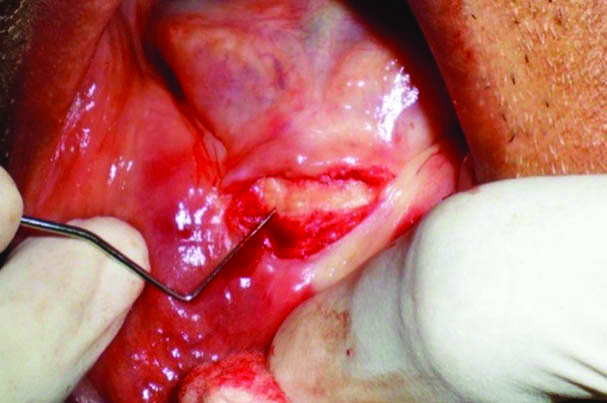
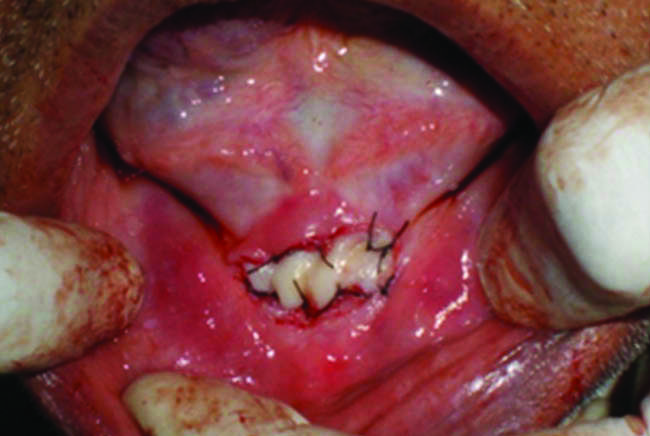
1) Surgical Procedure: The mandibular anterior region with deficient keratinized mucosa was measured using William’s periodontal probe [Table/Fig-3]. The maxillary ridge crest was found with adequate soft tissue thickness with appropriate ridge dimensions thus the palato-lateral slope of right maxillary ridge approximately 2-4 mm below the crest was selected as donor site for connective tissue graft. The patient was anesthetized locally with lignocaine 2% associated with epinephrine in concentration of 1:100,000. A mucoperiosteal incision with adequate antero-posterior extension was given on donor site to raise a partial-thickness flap using Bard-Parker blade no. 15. A free gingival graft was obtained from the donor site with minimal bleeding at the surgical site [Table/Fig-4,5]. The gingival graft was placed over the surgical area and fixed by compression sutures using absorbable thread (Vicryl suture) to remain stable and in close contact with the periosteal bed [Table/Fig-6,7]. The maxillary ridge donor sites were sutured using 4-0 silk threads to promote haemostasis and clot stabilization. Postoperative care included a 0.12% chlorhexidine rinse twice daily for two weeks, 500 mg of amoxicillin three times a day for seven days, 100 mg of Nimesulide two times a day for three days, and 500 mg of paracetamol as needed for pain. The suture removal was done after 14 days where the donor and recipient site presented eventful healing without any postoperative discomfort.
Measuring deficient site with William’s periodontal probe.

Free Gingival graft from Maxillary ridge.

Free gingival tissue graft.

Graft placed at desired site.
Graft sutured at deficient site.
2) Rest phase of healing: The healing was uneventful and a complete month of clinical observation demonstrated a stable healthy connective tissue at the anterior part of mandible.
3) Denture fabrication: After healing the conventional complete denture fabrication was done using selective pressure technique. The patient was highly satisfied with aesthetics as well as function of new complete denture prosthesis [Table/Fig-8].
Extra oral post-treatment.

Discussion
A fact considering the residual ridge resorption states that, resorption is a phenomenon occurring at faster rate post-extraction whereas continues for the rest of patient’s life [1]. In mandible the resorption rate is four times more than maxilla leading to non-retentive mandibular denture, often associated with pain and discomfort [2-3]. Inadequate keratinized tissue leads to the pain and discomfort during function of the prosthesis and causes mucosal inflammation. This can be attributed to decreased thickness of underlying keratinized mucosa providing less resilient and less tolerant denture foundation [4].
Patients with severely atrophic ridges due to long span edentulism, wearing a non-physiological denture from long time, maxillofacial injury or previous excision of an oral tumour usually are in a compromised condition for prosthetic rehabilitation by conventional denture or dental implants [5]. However, compromised soft tissue condition at atrophic ridges makes the rehabilitation more challenging. The adequate thickness of keratinized gingival mucosa is mandatory for a successful prosthetic rehabilitation both with conventional as well as implant supported prosthesisas this can offer more resistance to the forces of mastication and frictional contact that occur during function providing a prosthetic favorable environment [6]. The connective tissue layer over the ridge serves as a protective base for mucosa to denture loads and function [7].
Many technical and surgical treatment modalities are available to manage extremely resorbed mandibular ridges including special dentures, ridge augmentation and surgical corrections [8]. Materials including autografts, allografts, xenografts and alloplasts were introduced to augment the deficient keratinized mucosa. Connective tissue graft introduced first by Edel in 1974, was proved to be a highly predictable surgical procedure which is indicated to increase keratinized tissue in deficient sites [9].
The present article describes a technique to rehabilitate a severely resorbed mandible using a free gingival graft harvested from maxillary ridge and grafted on anterior part of mandible to increase the thickness of connective tissue under that denture.
Limitation
One limitation of this technique is that it involves two surgical sites, causing morbidity in both. However, with adequate medication, and a good follow-up during the first 15 days of healing, we can minimize this limitation [10]. All the available knowledge on this issue including the approaches described in this paper is based on very limited literature support and, thus, should be addressed with caution. These concerns should encourage long-term good clinical trials for better assessment of atrophic mandibular ridges.
Conclusion
The article presents a simple and minimally invasive technique to rehabilitate the lost thickness of keratinized mucosa on anterior region of mandibular ridge that is subjected to trauma from denture more frequently. The financial constraints and old age of the patient were the factors to select this technique. Though the effect of described treatment is short lived but the patient has shown quick acceptance to new denture and responded with great degree of comfort and confidence.
[1]. Cawood JI, Howell RA, A classification of the edentulous jawsInt J Oral Maxillofac Surg 1988 17:232-36.10.1016/S0901-5027(88)80047-X [Google Scholar] [CrossRef]
[2]. Studer S, Naef R, Scharer P, Adjustment of localized alveolar ridge defect by soft tissue transplantation to improve mucogingival esthetics: A proposal for clinical classification and an evaluation of proceduresQuintessence Int 1997 28:785-805. [Google Scholar]
[3]. Stratigos GT, Cassara A, Birnbaum M, Reverse visor osteotomy for augmentation of the atrophic edentulous mandibleJ Oral Maxillofac Surg 1982 40:231-33.10.1016/0278-2391(82)90318-4 [Google Scholar] [CrossRef]
[4]. Worthington P, Rubenstein JE, Problems associated with the atrophic mandibleDent Clin North Am 1998 42:129-60. [Google Scholar]
[5]. Güven O, Rehabilitation of severely atrophied mandible using free iliac crest bone grafts and dental implants: report of two casesJ Oral Implant 2007 33:122-26.10.1563/0.844.117674677 [Google Scholar] [CrossRef] [PubMed]
[6]. Van Scotter Boucher, The nature of supporting tissues for completed dentureJ Prosthet Dent 1965 15(2):285-94.10.1016/0022-3913(65)90099-5 [Google Scholar] [CrossRef]
[7]. Uccellani EL, Evaluating the mucous membranes of the edentulous mouthJ Prosthet Dent 1965 15(2):295-303.10.1016/0022-3913(65)90100-9 [Google Scholar] [CrossRef]
[8]. Turuck D, A Histologic comparison of the edentulous denture and non-denture bearing tissuesJ Prosthet Dent 1965 15(3):419-34.10.1016/S0022-3913(65)80010-5 [Google Scholar] [CrossRef]
[9]. Kydd WL, Daly CH, The biologic and mechanical effects of stress on oral mucosaJ Prosthet Dent 1982 47(3):317-29.10.1016/0022-3913(82)90162-7 [Google Scholar] [CrossRef]
[10]. Markov NJ, Cytologic study of keratinization under complete denturesJ Prosthet Dent 1968 20(1):8-13.10.1016/0022-3913(68)90207-2 [Google Scholar] [CrossRef]