Comparison of Conjunctival Autograft with Suture Versus Autograft with Patient’s Own Blood (without Suture) in Pterygium Surgery: A Pilot Study
Sucharita Das1, Vijay Pai2, Jayaram Shetty3, Hrishikesh Amin4, Subrahmanya K Bhat5, Vasanthi Kotian6
1 Resident, Department of Ophthalmology, K.S. Hegde Medical Academy, Mangalore, Karnataka, India.
2 Professor, Department of Ophthalmology, K.S. Hegde Medical Academy, Mangalore, Karnataka, India.
3 Professor, Department of Ophthalmology, K.S. Hegde Medical Academy, Mangalore, Karnataka, India.
4 Professor, Department of Ophthalmology, K.S. Hegde Medical Academy, Mangalore, Karnataka, India.
5 Additional Professor, Department of Ophthalmology, K.S. Hegde Medical Academy, Mangalore, Karnataka, India.
6 Additional Professor, Department of Ophthalmology, K.S. Hegde Medical Academy, Mangalore, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sucharita Das, Flat-205, Shradha Block, Swarna Ganga Residency, Virpur Khurd, Rishikesh, Uttarakhand-249203, India.
E-mail: sucharitadas19@hotmail.com
Introduction
Suturing is a conventional method for pterygium surgery. Owing to its several disadvantages newer techniques like autologous fibrin glue have been introduced as an alternative method of graft attachment.
Aim
To compare suture versus patient’s own blood for conjunctival autografting in pterygium surgery.
Materials and Methods
A pilot study was conducted in a Tertiary care hospital from October 2014-June 2016. Seventy-two adult patients with primary progressive pterygium undergoing pterygium surgery with conjunctival autograft were evaluated in this study. Thirty-six patients underwent primary pterygium excision and conjunctival autografting with autologous fibrin glue (glue group) and 36 with 10-0 monofilament polyamide (suture group). Parameters such as mean operating time, presenting complaints like pain, watering, burning and foreign body sensation and graft stability were compared between the two groups on 1st and 5th postoperative days. Categorical data were analysed by Fisher-exact test and continuous data were analysed using Student’s t-test and Wilcoxon signed rank test as applicable.
Results
There was statistically significant difference in the mean operating times between the two groups with results favouring the glue group (p<0.05). The difference in pain (p<0.05 each), watering (p=0.032), burning (p=0.023) and foreign body sensation (p<0.05 each) was found to be statistically significant between the two groups on 1st and 5th postoperative days respectively. The difference in graft stability between the two groups was not statistically significant (p=0.114).
Conclusion
In present study we found that autologous fibrin glue was associated with significantly shorter duration of surgery, lesser postoperative discomfort compared to suturing.
Autologous fibrin glue, Conjunctival autografting, Pterygium
Introduction
Pterygium is a triangular shaped structure occurring in the medial and/or lateral aspect of palpebral aperture in which the bulbar conjunctiva encroaches on to the cornea due to degenerative and hyperplastic processes [1]. The prevalence rate of primary pterygium varies from 0.7-31% in various populations around the world [2]. The number of surgical procedures for the management of pterygia includes various excision techniques like bare scleral excision, primary closure, conjunctival autograft, limbal conjunctival autograft, conjunctival flaps, and amniotic membrane graft, etc., [3]. Of these, limbal conjunctival autografting appears to be the best method with a low recurrence rate and high safety; however, it has the disadvantage of a relatively longer surgery time when compared with the bare sclera technique; also it carries the risk of complications such as granuloma formation and giant papillary conjunctivitis, and significant patient discomfort after surgery [4].
Fibrin glue, on the other hand, as an alternative to suturing, has the advantage of decreased operation time, improved postoperative discomfort, and avoidance of suture-related problems, but fibrin has the major drawback in the form of higher cost and the chance of transmission of infection [3]. There are limited studies on utility of autologous fibrin-glue for the purpose of autografting, especially those comparing the outcome of fibrin glue and suture. Anbari AA conducted a comparative study to evaluate efficacy, safety and reliability of autologous cryoprecipitate vis a vis absorbable sutures in pterygium excision surgery. He concluded that application of autologous cryoprecipitate glue instead of sutures for attaching the conjunctival autograft in pterygium surgery resulted in less postoperative pain and shorter surgical time [5]. In a similar study conducted by Foroutan A et al., the authors concluded that autologous fibrin glue was a safe and useful alternative method for graft fixation in pterygium surgery [6].
In the present study, glue derived from autologous blood was used for conjunctival autografting and its outcome was compared with sutures in pterygium surgery.
Materials and Methods
A pilot study was conducted in a Tertiary care hospital from October 2014-June 2016. A convenience sample of seventy-two adult patients with primary progressive pterygium undergoing pterygium surgery with conjunctival autograft was included and evaluated in this study. Ethical approval for conducting this study was obtained from Institutional Ethics Committee vide letter number INST.EC/EC/ 117/ 2014-15. Patients with eyelid/ocular surface disorders (i.e., blepharitis, etc.,), pseudopterygium (e.g., chemical burns, Sjogren syndrome and severe dry eye), history of previous ocular surgery/trauma and combined surgery (e.g., pterygium with cataract surgery) were excluded from the study. Thirty-six patients underwent primary pterygium excision and conjunctival autografting with autologous fibrin glue (glue group) and 36 with 10-0 monofilament polyamide (suture group) with every alternate patient assigned to one of the two groups (Universal sampling).
Autologous fibrin glue was prepared following the method described at www.audiotechnologies.net [7]. A 10 cc of blood was drawn from each of the patient. Whereas 4 cc of blood was transferred to empty test tube (A) and was left to coagulate, 6 cc of blood was transferred to test tube (B) with anti-coagulant (sodium citrate). Test tube (B) was centrifuged at 800 rpm for 8 minutes, which resulted in separation of red blood cells forming at the bottom and platelets on top. The “buffer coat” supernatant made up of platelets (pink) was aspirated unavoidably mixed with plasma (yellow). The “buffer coat” was transferred into empty test tube (C) and centrifuged together with test tube (A) at 1200 rpm for 8 minutes to further concentrate the platelets. The blood platelets were aspirated from the bottom of test tube (C), unavoidably intermingled with plasma. The plasma (containing the thrombin) was aspirated from the surface of test tube (A) which contained the coagulated blood. Blood platelets and thrombin were mixed on a concave microscope slide and 3-4 drops of calcium gluconate or calcium citrate was added to it.
All cases were subjected to complete history taking. After general ophthalmological examination every alternate patient was assigned to one group receiving autologous fibrin glue (glue group) and the other group receiving sutures (suture group). Surgical procedures were performed in all cases by the same surgical team under local anaesthesia. Surgery time was noted from insertion of the lid speculum till the lid speculum was removed. Eye to be operated was painted and draped. Lid speculum was applied. The Pterygium was extensively dissected to expose the sclera and corneal stroma. The subconjunctival fibrovascular tissue, including Tenon’s capsule, were thoroughly removed to provide clean scleral bed. The size of the defect was measured with Castroviejo calipers. Around 0.5 mm more than the measured defect marking was done on supero temporal conjunctiva. A thin Tenon-free conjunctival auto graft with limbal stem cell was excised. In patients in glue group a few drops of freshly prepared autologous fibrin glue was placed over the bare scleral bed. Autograft was slided over the cornea, and the orientation was kept limbus to limbus. It was slipped over the scleral bed to ensure that the epithelial side was up. After placement of graft over the bare sclera, it was gently pressed for 3 minutes. The graft adhesion was confirmed. The eye speculum removed and the eye was patched. In suture group patients, the graft with the epithelial side up was placed on bare sclera and was secured with 4-6 sutures using 10-0 monofilament polyamide. All the suture knots were buried underneath. Eye speculum removed. Eye was patched.
Patients were asked to follow up on the 1st, 5th and 14th day; and then 1st, 3rd and 6th month. Clinical photographs of the patients were taken before and after the operation. Complaints such as pain, watering, foreign body sensation and burning were graded on the 1st and 5th day. The complaints (pain, watering, foreign body sensation and burning) of patients were graded as follows: (a) No complaints: Grade 0 (nil); (b) Complaints which are easily tolerable: Grade 1 (mild); (c) Complaints and discomfort not affecting the daily activities and sleep: Grade 2 (moderate) and (d) Complaints and discomfort influencing daily activities and sleep: Grade 3 (severe) [4].
The data was analysed using Statistical Package for Social Sciences (SPSS) version 22.0 for windows. Binary variables were expressed as percentages and continuous variables as mean±Standard Deviation (SD) respectively. Categorical data was analysed by Fisher-exact test. Continuous data was analysed using Student’s t-test and Wilcoxon signed rank test as applicable. A probability value (p-value) of <0.05 was considered as statistically significant.
Results
Out of 72 patients, 42 (58.3 %) were males (23 in suture and 19 in glue group) and 30 (41.7%) were females (13 in suture and 17 in glue group). Age range and mean age+SD of the group receiving conjunctival autograft with suture was 26 years to 75 years and 58.1±13.35 years respectively and those for the glue group was 32 years to 84 years and 55±11.28 years respectively.
Comparison of mean operating time between the glue and suture groups has been depicted in [Table/Fig-1] and intra and postoperative findings in these two groups have been shown [Table/Fig-2,3] respectively. There was statistically significant difference between the operating times between the two groups with results favouring the glue group (p<0.05). Postoperative presenting features (with grading) between Glue and Suture groups have been depicted in [Table/Fig-4].
Comparison of mean Operating time between Glue and Suture group’s respectively.
| Presenting features | Glue Group (n=36) | Suture Group (n=36) | p-value (Unpaired students t-test) |
|---|
| Operating time (Mean±SD*) | 17.8±1.07 | 27.1±2.11 | <0.05 |
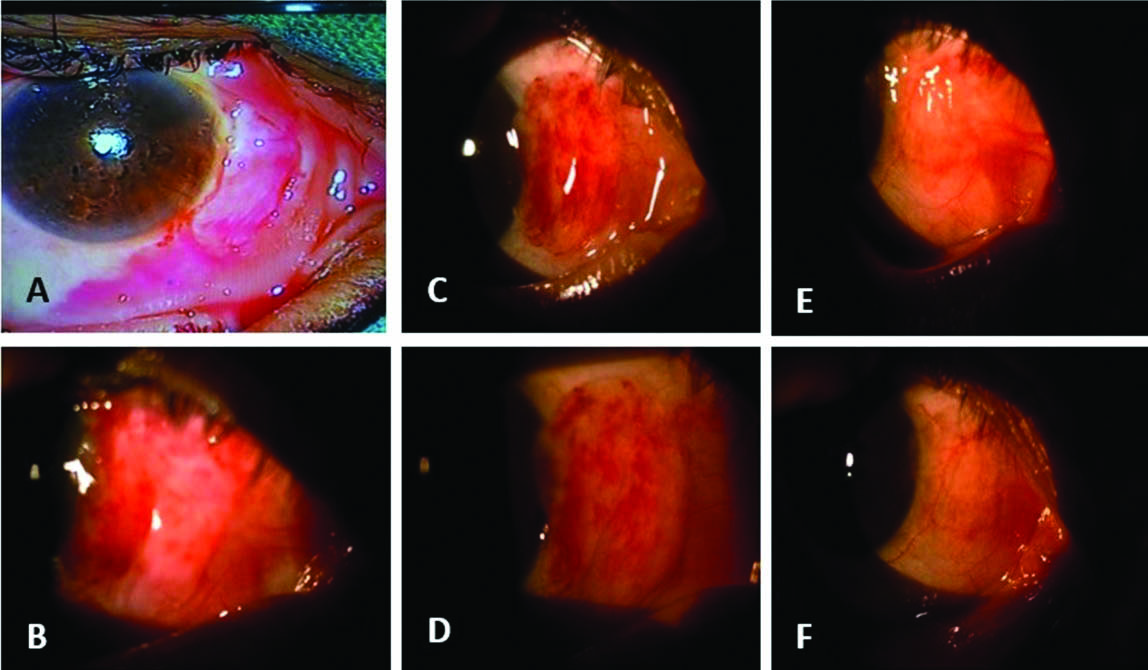
Intraoperative and postoperative findings in a 51-year-old woman operated for pterygium with autologous fibrin glue.
A: Intraoperative; B: Postoperative Day 1; C: Postoperative Day 5; D: Postoperative Day 14; E: Postoperative month 1; F: Postoperative month 3
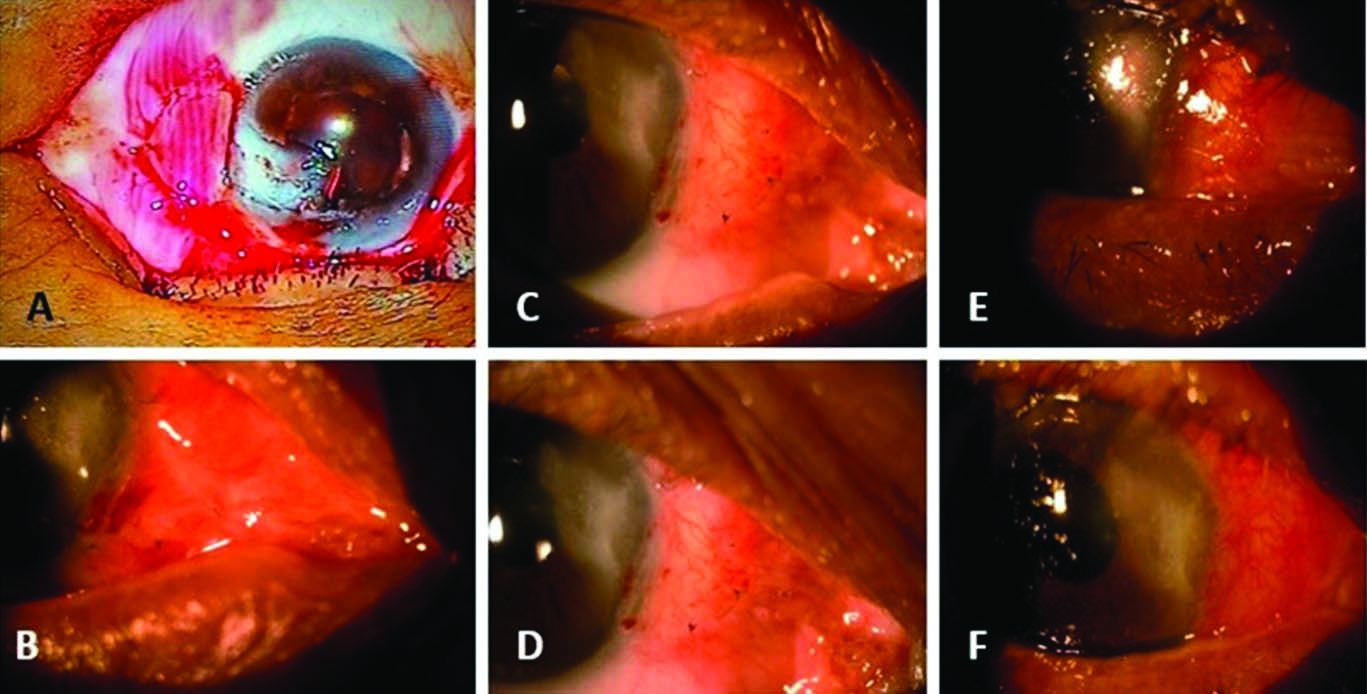
Intraoperative and postoperative findings in a 68-year-old woman treated with suture.
A: Intraoperative; B: Postoperative Day 1; C: Postoperative Day 5; D: Postoperative Day 14; E: Postoperative month 1; F: Postoperative month 3
Postoperative presenting features (with grading) between Glue and Suture group.
| Postoperative day | Glue group (N1=36) | Suture group (N2=36) |
|---|
| Grade | 0n1 (%) | 1n1 (%) | 2n1 (%) | 3n1 (%) | Grade | 0n2 (%) | 1n2 (%) | 2n2 (%) | 3n2 (%) |
|---|
| Presenting features | Presenting features |
|---|
| Day 1 | Pain | 0 (0) | 20 (55.6) | 14 (38.9) | 2 (5.6) | Pain | 0 (0) | 0 (0) | 26 (72.3) | 10 (27.8) |
| Watering | 2 (5.56) | 18 (50) | 14 (38.9) | 2 (5.6) | Watering | 0 (0) | 3 (8.4) | 32 (88.9) | 1 (2.8) |
| Burning | 4 (11.1) | 19 (52.8) | 11 (30.5) | 2 (5.6) | Burning | 0 (0) | 6 (16.7) | 29 (80.6) | 1 (2.8) |
| Foreign Body sensation | 7 (19.4) | 17 (47.2) | 11 (30.5) | 1 (2.8) | Foreign Body sensation | 0 (0) | 2 (5.6) | 28 (77.8) | 6 (16.7) |
| Day 5 | Pain | 1 (2.8) | 28 (77.8) | 7 (19.4) | 0 (0) | Pain | 0 (0) | 9 (25) | 27 (75) | 0 (0) |
| Watering | 9 (25) | 16 (44.4) | 11 (30.5) | 0 (0) | Watering | 0 (0) | 15 (41.7) | 21 (58.3) | 0 (0) |
| Burning | 10 (27.8) | 19 (52.8) | 7 (19.4) | 0 (0) | Burning | 0 (0) | 19 (52.8) | 17 (47.2) | 0 (0) |
| Foreign Body sensation | 12 (33.3) | 19 (52.8) | 5 (13.9) | 0 (0) | Foreign Body sensation | 0 (0) | 9 (25) | 27 (75) | 0 (0) |
Comparison of presenting features between Glue and Suture groups on 1st and 5th postoperative days respectively has been shown in [Table/Fig-5]. The difference in pain was found to be statistically significant between the two groups on 1st and 5th postoperative days respectively (p<0.05 each). There was statistically significant difference in watering between the two groups on 1st and 5th postoperative days respectively (p<0.05; p=0.032). The difference in burning sensation between the two groups was statistically significant on the 1st and 5th postoperative days respectively (p<0.05; p=0.023). Statistically significant difference in foreign body sensation was found between the two groups on 1st and 5th postoperative days respectively (p<0.05 each).
Comparison of presenting features between Glue and Suture groups on 1st and 5th postoperative days.
| Presenting features | Glue Group | Suture Group | p-value(Wilcoxon signed rank test) |
|---|
| Grade 2 and 3 pain on P.O.* Day 1 | 16 | 36 | <0.05 |
| Grade 2 and 3 watering on P.O. Day 1 | 16 | 33 | <0.05 |
| Grade 2 and 3 burning on P.O. Day 1 | 13 | 30 | <0.05 |
| Grade 2 and 3 FB** sensation on P.O. Day 1 | 12 | 34 | <0.05 |
| Grade 2 pain on P.O. Day 5 | 07 | 27 | <0.05 |
| Grade 2 watering on P.O. Day 5 | 11 | 21 | 0.032 |
| Grade 2 burning on P.O. Day 5 | 7 | 17 | 0.023 |
| Grade 2 FB sensation on P.O. Day 5 | 5 | 27 | <0.05 |
*Postoperative, **Foreign body
Comparison of graft stability in Glue and Suture group has been shown in [Table/Fig-6]. The difference between the two groups was not statistically significant. (p=0.114).
Comparison of graft stability in Glue and Suture group.
| Presenting features | Glue Group | Suture Group | p-value (Fisher-exact test) |
|---|
| Graft in place on P.O.* Day 1 | 32 | 36 | = 0.114 |
*Postoperative
Discussion
In the present study, the mean operating time was found to be significantly shorter in glue group compared to suture group. Similar studies conducted by Karalezli A et al., Anbari AA, Koranyi G et al., Pan HW et al., Cha DM et al., and Uy HS et al., respectively also observed reduced mean operating time [4,5,8-11].
Postoperative patient discomfort was significantly lower in glue group. Koranyi G et al., in their study found significantly lower pain levels in the glue group both on day 0, and at each point of time during the first postoperative week, p<0.05 [8]. Karalezli A et al., in their study observed the intensity of postoperative pain, foreign-body sensation, irritation and epiphora were significantly lower in fibrin group than in those treated with sutures (p<0.001) at both postoperative days 1 and 10 [4]. Yuksel B et al., studied 58 eyes of 58 patients operated for primary nasal pterygium with fibrin tissue adhesive and 8-0 Virgin silk sutures in 29 eyes each; their study showed using fibrin glue for graft fixation in pterygium surgery significantly decreases postoperative patient discomfort (p<0.001) [12]. Arora R et al., in their study found that patient comfort was significantly higher in the tissue glue group than the vicryl suture group (p<0.05) during the first 6 weeks of postoperative follow up; they also reported in their study that the postoperative inflammation was less often seen with fibrin glue compared to suture [13]. Ozdamar Y et al., in their study concluded that the use of tissue glue decreases patient symptoms during the postoperative period after pterygium surgery compared with sutures (p<0.05) [14]. Uy HS et al., in their study found that postoperative symptoms were fewer for the fibrin glue than the suture group [11].
There was no statistically significant difference in graft stability on first postoperative day between the two groups. Uy HS et al., reported that all autografts in both group were successfully attached and were intact after two months [11]. Ozdamar Y et al., reported that tissue glue was efficacious in securing the limbal conjunctival autograft in pterygium surgery [14]. In a study by Foroutan A et al., two eyes (13.3%) developed total graft dehiscence, and sutures were used for reattachment of the graft in its correct position [6]. Haemorrhage was noted under the graft in two patients in glue group which subsided by 14th day.
Limitation
The limitation of our study was short study duration as a result of which recurrence could not be evaluated.
Conclusion
Autologous fibrin glue offers an alternative method of graft attachment. In our study we found that autologous fibrin glue was associated with significantly shorter duration of surgery, lesser postoperative discomfort compared to suturing.
*Postoperative, **Foreign body
*Postoperative
[1]. Cornea and Sclera. In: Duke-Elder S, editorTextbook of Ophthalmology 1954 1st ednUnited StatesSt Louis, Mosby:570-86.10.1136/bmj.1.4866.859 [Google Scholar] [CrossRef]
[2]. Dulani N, Dulani H, Efficacy of blood oozed during pterygium excision to secure autograftInt J Pharm Biomed Res 2014 5:58-60. [Google Scholar]
[3]. Janson BJ, Sikder S, Surgical management of pterygiumOcular Surface 2014 12:112-19.10.1016/j.jtos.2014.01.00124725323 [Google Scholar] [CrossRef] [PubMed]
[4]. Karalezli A, Kucukerdonmez C, Akova YA, Altan-Yaycioglu R, Borazan M, Fibrin glue versus sutures for conjunctival autografting in pterygium surgery: a prospective comparative studyBr J Ophthalmol 2008 92:1206-10.10.1136/bjo.2008.13960018621797 [Google Scholar] [CrossRef] [PubMed]
[5]. Anbari AA, Autologous cryoprecipitate for attaching conjunctival autografts after pterygium excisionMiddle East Afr J Ophthalmol 2013 20:239-43.10.4103/0974-9233.114801PMC3757635 [Google Scholar] [CrossRef] [PubMed]
[6]. Foroutan A, Beigzadeh F, Ghaempanah MJ, Ashghi P, Amirizadeh N, Sianati H, Efficacy of autologous fibrin glue for primary pterygium surgery with conjunctival autograftIranian J Ophthalmol 2011 23:39-47. [Google Scholar]
[7]. Gossolengo, Piacenza. Audio Tips: Preparation of autologous “fibrin glue” [Internet]. Audio Technologies srl Italy. 2008 [cited 4 August 2014]. Available from: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=12&cad=rja&uact=8&ved=0ahUKEwiHyOWU4J3cAhXEYysKHTt0AJ8QFghGMAs&url=http%3A%2%2Fwww.audiotechnologies.ne%2F&usg=AOvVaw3PFs47ENdzeEpPqytYFaMq [Google Scholar]
[8]. Koranyi G, Seregard S, Kopp ED, Cut and paste: a no suture, small incision approach to pterygium surgeryBr J Ophthalmol 2004 88:911-14.10.1136/bjo.2003.03285415205236 [Google Scholar] [CrossRef] [PubMed]
[9]. Pan H-W, Zhong J-X, Jing C-X, Comparision of fibrin glue versus suture for conjunctival autografting in pterygium surgeryOphthalmology 2011 118:1049-54.10.1016/j.ophtha.2010.10.03321292327 [Google Scholar] [CrossRef] [PubMed]
[10]. Cha DM, Kim KH, Choi HJ, Kim MK, Wee WR, A comparative study of effect of fibrin glue versus sutures on clinical outcome in patients undergoing pterygium excision and conjunctival autograftsKorean J Ophthalmol 2012 26:407-13.10.3341/kjo.2012.26.6.40723204794 [Google Scholar] [CrossRef] [PubMed]
[11]. Uy HS, Reyes JMG, Flores JDG, Lim-Bon-Siong R, Comparison of fibrin glue and sutures for attaching conjunctival autografts after pterygium excisionOphthalmology 2005 112:667-71.10.1016/j.ophtha.2004.08.02815808260 [Google Scholar] [CrossRef] [PubMed]
[12]. Yuksel B, Unsal SK, Onat S, Comparison of fibrin glue and suture technique in pterygium surgery performed with limbal autograftInt J Ophthalmol 2010 3:316-20. [Google Scholar]
[13]. Arora R, Goyal JL, Kang J, Seetaram S, Fibrin glue versus vicryl suture in limbo conjunctival autograft in the management of primary pterygium: A prospective comparative study. In: Bhattacharya D, editorAll India Ophthalmological Conference proceedings 2010 2010 Jan 21-24 Kolkata, India2010: Pp 263-65 [Google Scholar]
[14]. Ozdamar Y, Mutevelli S, Han U, Ileri D, Onal B, Ilhan O, Comparative study of tissue glue and vicryl suture for closing limbal-conjunctival autografts and histologic evaluation after pterygium excisionCornea 2008 27:552-58.10.1097/ICO.0b013e318165b16d18520504 [Google Scholar] [CrossRef] [PubMed]