Parturition is painful and a relatively long process. First stage of parturition in nulliparous women and multiparous women is 12-16 hours and 6-8 hours, respectively [1]. Severe pain of parturition has harmful effects on the mother and foetus that includes increased cardiac output, increased blood pressure, mother’s tachycardia, reducing the effectiveness of contractions, slow progress of labour, reduced blood flow to the placenta and foetal oxygen limitation. Furthermore, this pain may create long-term emotional imbalance that causes mother’s health to be impaired. It also has negative effects on the foetus [2,3].
Duration of parturition is one of the effective factors in the maternal and foetal complications [4]. Prolonged duration of the labour stages has some complications such as uterine muscle fatigue, physical exhaustion, and dehydration of mother. Also, the chances of endometritis, cesarean delivery, foetal distress, foetal and infant mortality are increased. The mother is at risk of bleeding and infection after childbirth and developing mental disorders due to anxiety, insomnia and fatigue [5].
It is believed that prescribing certain drugs such as atropine and hyoscine shortens the active phase of labour and thus decreases duration of pain [9]. When hyoscine acts on the central nervous system, it shows different characteristics. Hyoscine causes depression in cerebral cortex and has a strong hypnotic effect [6]. This drug is used due to antispasmodic effects on smooth muscle in disorders of visceral spasm such as bronchial spasm, ureteral and bladder spasm and intestinal colic [10]. It is claimed that spasmolytic drugs are also effective in improving cervical spasms and facilitate dilation of the cervix during labour [6].
With regard to extensive use of pharmacological and non-pharmacological methods in birth centers and limited studies in terms of their effect, this study was conducted with an aim to compare the effect of hot shower and intravenous injection of hyoscine on the pain severity and duration of active phase of labour (primary outcomes) and adverse events during intervention (secondary outcomes) in nulliparous women.
Materials and Methods
This study was a three-arm parallel-group, randomized control study conducted in the maternity ward of 29-Bahman hospital in May 2015 to Jan 2016. The study population consisted of 162 nulliparous women who were 18-35 years old and were in active phase of labour (4 cm dilation).
Inclusion criteria were nulliparity, spontaneous start of labour pain, no pregnancy complications, normal foetal heart-rate based on cardiotocography (CTG), vertex presentation based on the diagnostic sonography, and woman’s inclination to enter the study. Exclusion criteria were contraindication of vaginal delivery, taking any sedative or narcotic drug within 48 hours prior to entering the hospital, having history of a mental disorder, having history of any medical disease such as cardiovascular, thyroid, liver, kidney, asthma and epilepsy.
Sample Size: The sample size based on both variables of labour pain and duration of first stage of labour was determined. According to the duration of the first stage of labour (in minutes) and by taking m1 = 260.4, m2 = 186.8, sd1 = 120.9, sd2 = 125.6, α = 0.05 and β =0.1, a sample size of 49 participants was calculated considering the 10% loss, 54 individuals were determined. According to labour pain and considering the m1= 6.83 and assuming a 15% reduction in labour pain (m2 = 5.80), sd1 = sd2 = 1.31, α = 0.05 and β = 0.1, a sample size of 36 participants was calculated considering the 10% loss, 40 were determined. Given the sample size calculated based on the duration of the first stage of labour was more, so the final sample size of 54 participants in each group was considered.
Sampling: After approving the project, obtaining the code of ethics (code: 93165) from Ethics Committee of Tabriz University of Medical Sciences, and registering study in clinical trial website of Iran (No. IRCT2015012610324N2), the sampling began. Primary convenience was done; hence, all women in the maternity ward of 29-Bahman hospital that had 4 cm dilation of cervix were assessed in terms of inclusion and exclusion criteria. If they had the above-mentioned eligibility criteria, the aim and method of the study were explained to them; if they had the inclination to participate in the study, written consent form was taken from them. For all participants, foetal heart-rate and cervical dilation were measured. Then, socio-demographic characteristics questionnaire was completed, and standard routine care of hospital was done. Routine care includes CTG recording on arrival, venipuncture, control of FHR every half hour and physician visit.
Randomization: Participants were assigned into three groups (the first intervention group who received hyoscine, the second intervention group who received hot shower and the control group who received routine care) through block randomization with block sizes of 3 and 6. For allocation concealment, intervention type was written on the paper and was put in the sealed opaque envelopes numbered sequentially. Randomization was conducted by person not involved in the sampling and data collection.
Intervention: In first intervention group, hyoscine was prescribed by obstetricians and then 20 mg/mL hyoscine diluted with 5 cc distilled water was injected intravenously in 4 cm dilation, then in 7 cm dilation. Duration of the intravenous injection was about 1-2 minutes. In the second intervention group, in addition to routine care, hot shower was applied on pregnant mother’s arrival to active phase of labour for the first time in 4 cm dilation and then in 7 cm dilation. Hot shower was used for 20 minutes in each of both the dilations. First, there was complete wash of body or waist wash for 5 minutes, then the participants could use shower for every part of body they feel comfortable. Water temperature was continuously measured using a digital thermometer in the bathroom cabin; it was kept fixed at 37°C. After shower, foetal heart-rate and body temperature were controlled and recorded.
In Iran, with the aim to encourage vaginal births and providing a pleasant and private environment for parturient women, Labour-Delivery-Recovery (LDR) rooms (where women can give birth and stay there for 2 hours after delivery) have been constructed across the country. Bathtubs are provided to every LDR room, so women can also take advantage of water treatment services. Midwife or woman’s companion can support her.
Data Collection Tool: Information were collected by socio-demographic characteristics questionnaire, VAS, standard partograph form and adverse events checklist of received intervention.
Socio-demographic characteristics questionnaire consisted of questions about age, education, education of husband, economic status, housemate persons, smoking and planned pregnancy.
VAS was numbered like scaled ruler from 0 to 10; zero indicates lack of pain and ten indicates unbearable pain [11]. Immediately before intervention, and then every hour after intervention, pain was measured according to pain scale, VAS.
In every group, time interval of 4 cm cervical dilation to full dilatation of the cervix was measured by timer. Furthermore, childbirth progress was assessed according to standard partograph form received from Ministry of Health of Iran. Side effects of intervention received during labour were recorded in the relevant checklist.
Statistical Analysis
After completing questionnaire, data was analysed by SPSS 20 software. To assess the homology of groups in terms of socio-demographic characteristics, one-way analysis of variance, chi-square test, chi-square for trend, and Fisher’s-exact tests were used. K-S test was used to assess the normality of quantitative data. One-way analysis of variance test was used to compare the baseline score of pain severity (before intervention) and duration of active phase of labour among study groups; general linear model with adjusting the baseline score was used to compare average pain severity during intervention among study groups.
Results
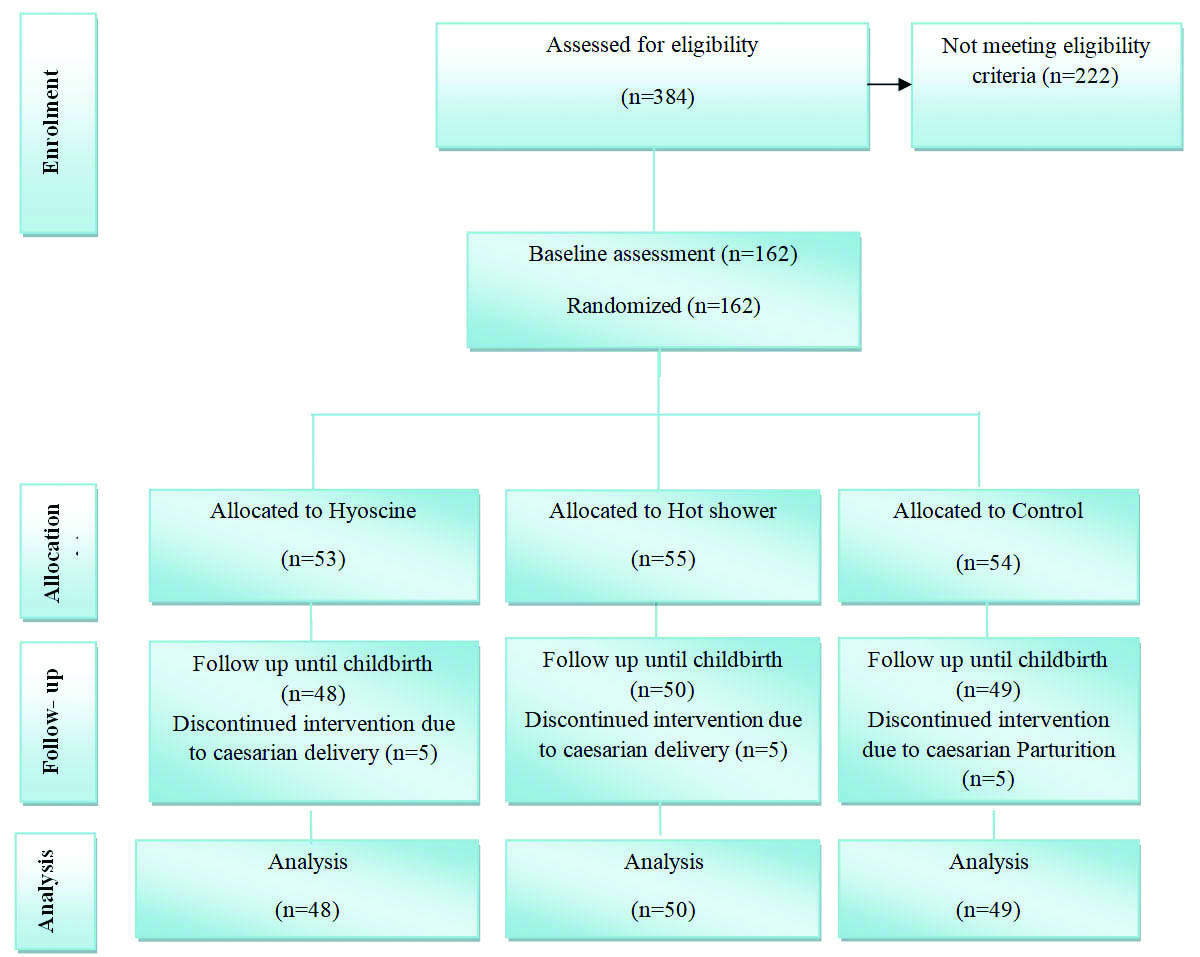
Only 162 women from 384 nulliparous women that were assessed by the researcher had eligibility criteria for the study. After receiving consent form, they were allocated into three groups {hyoscine (n=53), hot shower (n=55), and control (n=54)}. Of 162 participants, 15 women {5 women in each of the three groups) underwent Cesarean Section (CS) due to different reasons (meconium-stained amniotic fluid (4 cases; 3 cases after the first period of intervention and 1 case after the second period of intervention), lack of descent (6 cases; 3 cases after the first period of intervention and 3 cases after the second period of intervention), foetal bradycardia (5 cases; 3 cases after the first period of intervention and 2 case after the second period of intervention)}, so they were excluded. Finally, 147 women were controlled until the end of the study [Table/Fig-1]. The foetal distress was confirmed by the electronic foetal heart-rate monitoring. All newborns after CS had good APGAR scores and no newborn was hospitalized after CS.
In terms of socio-demographic characteristics, there was no statistically significant difference between the three groups. This indicates homologies of all groups (p>0.05) [Table/Fig-2].
Socio-demographic characteristics of all participants.
| Characteristics | Hyoscine Number (Percent) n=53 | Hot shower Number (Percent) n=55 | Control Number (Percent) n=54 | p-value |
|---|
| Age (year) | 23.6±3.8* | 22.6±3.8* | 24.5±4.14* | 0.044† |
| Educational level | 0.104§ |
| Primary school | 1 (1.9) | 5 (9.1) | 5 (9.3) | |
| Secondary school | 13 (24.5) | 11 (20.0) | 23 (42.6) | |
| High school or diploma | 29 (54.7) | 30 (54.5) | 19 (35.2) | |
| University | 10 (18.9) | 9 (16.4) | 7 (13.0) | |
| Job | 0.942‡‡ |
| Housewife | 52 (98.1) | 52 (94.5) | 51 (94.4) | |
| Employed | 1 (1.9) | 3 (5.4) | 3 (4.6) | |
| Husband’s Education | 0.455§ |
| Illiterate | 0 (0) | 2 (3.6) | 1 (1.9) | |
| Primary school | 8 (15.1) | 9 (16.4) | 6 (11.1) | |
| Secondary school | 12 (22.6) | 10 (18.2) | 18 (33.3) | |
| High school or diploma | 26 (49.1) | 24 (43.6) | 25 (46.3) | |
| University | 7 (13.2) | 10 (18.2) | 4 (7.4) | |
| Sufficiency of income for living costs | 0.495§ |
| Insufficient | 13 (24.5) | 12 (21.8) | 17 (31.5) | |
| Relatively sufficient | 40 (75.5) | 43 (78.2) | 37 (68.5) | |
| Housemate persons | 0.188‡ |
| Myself and my husband | 35 (66.0) | 42 (76.4) | 39 (72.2) | |
| My parents | 2 (3.8) | 0 (0) | 4 (7.4) | |
| Husband’s parents | 16 (30.2) | 13 (23.6) | 11 (20.4) | |
| Smoking | 0.500 ‡ |
| Yes | 8 (15.1) | 8 (14.5) | 12 (22.2) | |
| No | 45 (84.9) | 47 (85.5) | 42 (77.8) | |
| Wanted pregnancy | 0.195 ‡ |
| Yes | 51 (96.2) | 50 (90.9) | 53 (98.1) | |
| No | 2 (3.8) | 5 (9.1) | 1 (1.9) | |
* The numbers show mean±standard deviation; †One-way Analysis of variance (ANOVA); ‡Chi-square test; ‡‡ Fisher-exact test; § Chi-square test for trend
Average (standard deviation) duration of the active phase of labour in hyoscine, hot shower, and control groups was 221.2 (87.2), 201.9 (147.4) and 312.6 (198.0) minutes, respectively. There was statistically significant difference in terms of duration of active phase of labour among groups (p<0.001) [Table/Fig-3].
Comparison of active phase of labour duration (minutes) in studied group.
| Variable | Hyoscine (n=48)Mean (SD#) | Hot Shower (n=50)Mean (SD#) | Control (n=49)Mean (SD#) |
|---|
| Duration of active phase | 221.2 (87.2) | 201.9 (147.4) | 312.6 (198.0) |
| Comparison of groups | Hyoscine with hot showerMD (95%Cl)§; P | Hyoscine with controlMD (95%Cl)§; P | Hot shower with ControlMD (95%Cl)§; P |
| 19.3 (-40.2 to 78.8); 0.522 | -91.3 (-1150.5 to -32.1); 0.003 | -110.7 (-169.5 to -51.8); <0.001 |
For comparison groups, one-way analysis of variance was used.
# Standard deviation; §Mean difference (95% Confidence interval)
Before the intervention in the study groups, no statistically significant difference was observed in terms of average pain intensity (p=0.149). According to general linear model by adjusting the baseline values, average pain intensity in hot shower group was significantly less than control group (p<0.001). There was no statistically significant difference between the two-hyoscine and control groups (p=0.616) [Table/Fig-4].
Comparison of pain intensity in studied groups.
| Variable | Hyoscine (n=48)Mean (SD) * | Hot Shower (n=50) Mean(SD) * | Control (n=49)Mean (SD) * |
|---|
| Pain intensity |
| Before intervention | 6.7 (1.6) | 6.6 (1.6) | 7.2 (1.9) |
| During intervention | 8.6 (1.1) | 7.2 (1.2) | 8.5 (1.3) |
| Comparison of the groups | Hot shower with hyoscine AMD (95% Cl)†; P | Hyoscine with control AMD (95%Cl)†; P | Hot shower with Control AMD (95%Cl)†; P |
| Before intervention | 0.0 (-0.8 to 0.8); 1.000 | -0.6 (-1.4 to 0.2); 0.261 | -0.6 (-1.4 to 0.2); 0.239 |
| During intervention | -1.3 (-1.8 to -0.8); <0.001 | 0.2 (-0.3 to 0.7); 0.616 | -1.1 (-1.6 to -0.6); <0.001 |
For comparison groups before intervention, one-way analysis of variance was used and for comparison after intervention groups, ANCOVA was used.
* mean (Standard Deviation); † Adjusted mean difference (Confidence interval of 95%)
Adverse events such as dry mouth, hot flash, dry skin, heart palpitations, insomnia, dizziness, fatigue, blurred vision, constipation, abdominal distension, photophobia and urinary incontinence were observed in the three groups [Table/Fig-5].
Adverse events of intervention in studied groups.
| Adverse event | Hot showerNumber (Percent)n=50 | HyoscineNumber(Percent)n=48 | ControlNumber(Percent)n=49 |
|---|
| Dry mouth | 37 (77.1) | 37 (74.0) | 29 (59.2) |
| Hot flash | 16 (33.3) | 11 (22.0) | 14 (28.6) |
| Dry skin | 7 (14.6) | 7 (14.6) | 4 (8.2) |
| Heart palpitations | 34 (70.8) | 27 (54.0) | 22 (44.9) |
| Insomnia | 23 (47.9) | 29 (58.0) | 24 (49.0) |
| Dizziness | 18 (37.5) | 20 (40.0) | 11 (22.4) |
| Fatigue | 29 (59.2) | 37 (74.0) | 33 (68.8) |
| Blurred vision | 18 (37.5) | 8 (16.0) | 5 (10.2) |
| Constipation | 7 (14.6) | 10 (20.0) | 5 (10.2) |
| Abdominal distension | 5 (10.4) | 10 (20.0) | 7 (14.3) |
| Photophobia | 6 (12.5) | 4 (8.0) | 2 (4.1) |
| Urinary incontinence | 17 (35.4) | 18 (36.0) | 17 (34.7) |
Discussion
In this study, duration of active phase of labour in two intervention groups (hyoscine and hot shower) was less than control group. Furthermore, in terms of pain intensity during intervention, average pain intensity in hot shower group was significantly less than control group and hyoscine group.
In this study, duration of active phase of labour in both intervention groups was less than that in the control group. Makvandi S et al., conducted a study about the effect of hyoscine on the delivery process. In terms of average cervical effacement and dilatation at 1 and 2 hours after intervention as well as the duration of the active phase of labour, there was significant difference between the intervention and control groups; and the second stage of labour in intervention group was significantly less than that in the control group [5]. Sekhavat L et al., and Al Qahtani NH et al., showed in their studies that hyoscine injection in active phase of labour results in reduced time of active phase without foetal and maternal complications [12,13]. In a study, Samuels LA et al., showed that hyoscine significantly reduced duration of active phase of labour [14]. The results of the above studies are in line with the current study. Mechanism by which hyoscine reduces duration of delivery stages, is not known and evidence for effectiveness of the drug is empirical to a large extent [12]. Gupta B et al., and Ebrahimzadeh Zagami S et al., concluded that hyoscine has no important role in labour progress [15,16]. Contrarily, Mortazavi F et al., have assessed the effects of atropine, hyoscine and promethazine and they stated that these drugs cause increased delivery duration in intervention group than in the control group [17]. Hyoscine is an anticholinergic drug whose relaxant effects work directly on the smooth muscle but has no effect on the spontaneous contractions of the uterus [18].
In the current study, use of hot water caused duration of active phase of labour to be reduced more than the control group. Today, use of hot water and its physiologic and mental effects has become increasingly popular as one of the non-pharmacological methods. In hot shower, increase of relaxation is due to heating and hydrostatic effects of water; it also causes reduction in sympathetic nervous system activity and reduces catecholamine levels [19]. Liu Y et al., showed that there is no significant difference in terms of duration of first stage of delivery between water birth and control groups [8]. Cluett ER in a systematic review concluded that water immersion during the first stage of labour reduces the use of epidural/spinal analgesia and duration of the first stage of labour [20]. Behmanesh F et al., assessed thermotherapy effect on the duration of labour stages in nulliparous women and showed that thermotherapy decreases duration of first and third stages of labour [21]. In this regard, studies of Mollamahmutoglu L et al., Harper B., and Zanetti-Daellenbach RA et al., showed that warm water reduces duration of labour stages [22-24]. Furthermore, heat creates a significant increase in the uterine activity without any abnormal changes in foetal heart. The results of current study are consistent with the results of all above mentioned studies. Furthermore, in the current study, duration of active phase of labour in hot shower was similar to hyoscine.
In current study, average pain intensity in hot shower was statistically lower than the control and hyoscine groups. In order to determine effectiveness of hot shower on the pain intensity and experience of childbirth, Lee SL et al., in his study concluded the intervention group had less pain in 4-7 cm dilatation and also had better experience in childbirth than control group [25]. Aggarwal P et al., and Fardiazar Z et al., considered hyoscine as an effective drug in reducing severe pain [26, 27]. The results of these studies didn’t approve results of current study. Hyoscine may reduce pain due to spasmolytic effects [28]. But, some studies such as studies of Makvandi S et al., suggested failure in reducing labour pain in the group received hyoscine that are consistent with the results of present study [5].
Regarding effect of warm water on the pain intensity, Lee and his colleagues (2013) showed that women of intervention group who received hot shower have remarkably less pain. In aforementioned study such as current study, duration of hot shower was 20 minutes [25]. Davim RM et al., showed the effect of non-pharmacological strategies such as hot shower on pain relief [29]. Also, in a research, Santana SL et al., showed that shower bath therapy during the first stage reduced pain intensity compared with control groups. It can create feeling of comfort and relaxation between contractions without the side effects that is satisfactory from mothers’ points of view [19]. In addition to positive and healthy effects, use of hot shower is an easy and non-pharmacological method to reduce labour pain, so women can participate in child- birth process and feel comfortable and supportive.
In this study, adverse events such as dry mouth, hot flash, dry skin, heart palpitations, insomnia, dizziness, fatigue, blurred vision, constipation, abdominal distension, photophobia and urinary incontinence were observed. Hyoscine may cause drowsiness, low blood pressure, dryness of oral mucosa, nausea, vomiting, blurred vision, constipation and urinary retention. Confusion, irritability, chills, hallucinations, psychosis and behavioural disorders are other side effects of this medication [18]. Dry mouth, flushing and tachycardia have been reported as side effects of hyoscine in some studies [30,31]. In some studies, hyoscine butylbromide had not any adverse effect on mother and neonate [5,12-15].
Limitation
The strength of this study is to compare a pharmacologic method with a non-pharmacologic method to reduce pain and the duration of labour stages. Following all principals of clinical trials including random allocation and allocation concealment is other strength of this study. This study was implemented only in one hospital affiliated with the social security organization in Tabriz that reduces the generalizability of study findings, a limitation of our study.
Conclusion
The results of this study show that use of non- pharmacological method of hot shower reduces the pain intensity and duration of labour. Thus, it is suggested to apply hot shower as a safe method of pain relief in childbirth process.
* The numbers show mean±standard deviation; †One-way Analysis of variance (ANOVA); ‡Chi-square test; ‡‡ Fisher-exact test; § Chi-square test for trend
For comparison groups, one-way analysis of variance was used.
# Standard deviation; §Mean difference (95% Confidence interval)
For comparison groups before intervention, one-way analysis of variance was used and for comparison after intervention groups, ANCOVA was used.
* mean (Standard Deviation); † Adjusted mean difference (Confidence interval of 95%)