Giant Cell Reparative Granuloma of Proximal phalanx of 4th Toe-A Rare Case Report
Divya Prafulla Yerraguntla1, Sachin Shivaji Kapse2, Disha B. Shankar3, Surekha U. Arakeri4, Parth Avinash Vaishnav5
1 Postgraduate Student, Department of Pathology, B.L.D.E University’s Shri. B. M. Patil Medical College, Vijayapura, Karnataka, India.
2 Postgraduate Student, Department of Pathology, B.L.D.E University’s Shri. B. M. Patil Medical College, Vijayapura, Karnataka, India.
3 Postgraduate Student, Department of Pathology, B.L.D.E University’s Shri. B. M. Patil Medical College, Vijayapura, Karnataka, India.
4 Professor, Department of Pathology, B.L.D.E University’s Shri. B. M. Patil Medical College, Vijayapura, Karnataka, India.
5 Postgraduate Student, Department of Radiology, B.L.D.E University’s Shri. B. M. Patil Medical College, Vijayapura, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sachin Shivaji Kapse, Postgraduate Student, Department of Pathology, Shri. B.M. Patil Medical College, BLDE Campus, Vijayapura, Karnataka, India.
E-mail: sachinkapse004@gmail.com
Giant Cell Reparative Granuloma (GCRG) is locally aggressive, non-neoplastic lesion. It is an uncommon lesion commonly found in maxilla and mandible and rare in the toes. Due to absence of classical radiological features and rare incidence of GCRG at toe, clinically and radiologically this lesion is frequently misdiagnosed. So, histopathological evaluation is necessary to confirm the diagnosis of GCRG. This is a case of GCRG of proximal phalanx of right fourth toe in a young woman.
Benign, Bone, Foot, Non-neoplastic
Introduction
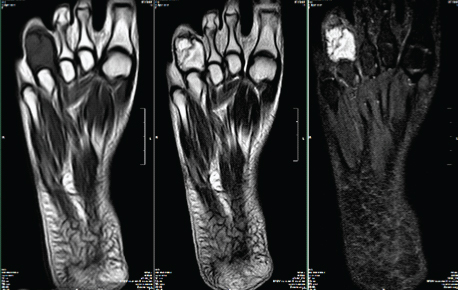
A 21-year-old female presented with complaints of pain and swelling on right side of fourth toe since one and half year. The swelling increased gradually. There was no history of trauma, fever, infection and clinical features suggestive of hyperparathyroidism. On examination, the swelling was tender and hard. A plain X-ray showed lytic lesion in the middle of fourth toe with evidence of erosion of mid and distal phalanges [Table/Fig-1]. Computed Tomography (CT) showed well defined expansile lytic lesion with multiple septations and evidence of cortical break in proximal phalanx of fourth toe with soft tissue swelling. Magnetic Resonance Imaging (MRI) revealed a well-defined expansile lesion (hypointense T1/Hyperintense T27 STIR) measuring about 2.3x2.1 cm in the proximal phalanx of fourth toe with hypointense septations [Table/Fig-2]. Diagnosis of enchondroma was considered based on radiological examination. Surgical amputation of involved fourth toe was done and the specimen was sent for histopathological study.
Plain X-ray showing lytic lesion in the middle and proximal phalanx of 4th toe.

MRI showing well-defined expansile lesion (hypointense T1/Hyperintense T27 STIR) measuring about 23x21 mm in proximal phalanx of 4th toe with hypointense septations.
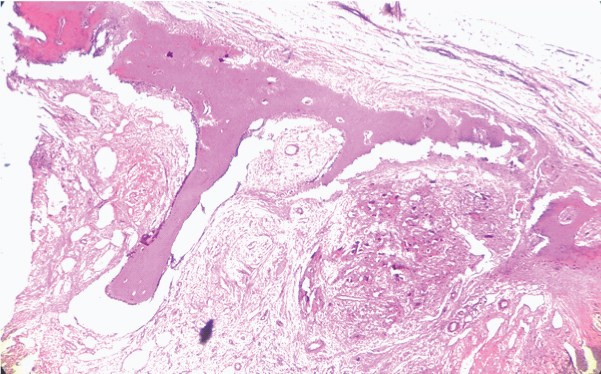
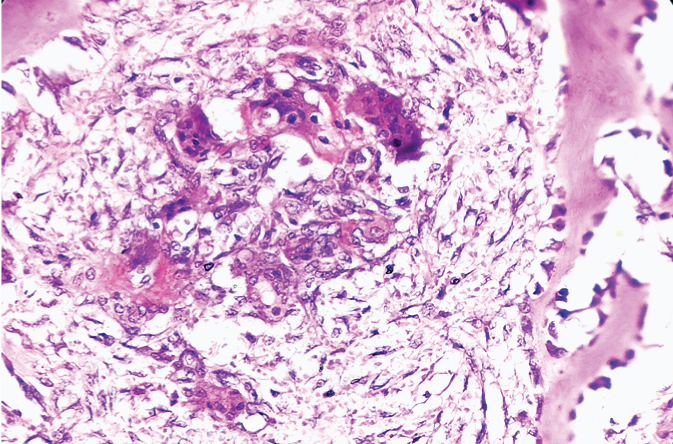
Gross morphology revealed disarticulated specimen of right fourth toe measuring 6x3.5x2.5 cm with attached skin and nail. Cut section showed a brown coloured mass surrounded by bony tissue measuring 3.5x2.5 cm. Microscopic examination showed bony trabeculae and cartilage along with extensive areas of haemorrhage, small capillaries, haemosiderin laden macrophages and reactive bone formation with osteoblastic rimming [Table/Fig-3]. Intervening stroma showed collagen rich connective tissue with small, oval and spindle shaped mononuclear cells mixed with numerous osteoclastic giant cells distributed unevenly [Table/Fig-4].
Photomicrograph showing bony trabecula with areas of hemorrhage. (H&E, 10X).
Photomicrograph showing reactive bone formation with osteoblastic rimming along with small, oval and spindle shaped mononuclear cells admixed with osteoclastic giant cells and RBCs. (H&E, 40X).
Based on above histomorphological features diagnosis of giant cell reparative granuloma was made.
Discussion
GCRG is an uncommon, benign locally destructive disease. It is most commonly seen in facial bones like maxilla and mandible and is rarely seen in small tubular bones of the hand and feet. It should be differentiated from other giant cell forming tumour and tumour-like conditions such as giant cell tumour, aneurysmal bone cyst and brown tumour of hyperparathyroidism. As treatment modality for these conditions are different, it is important to differentiate these conditions from each other [1-3].
In 1953, GCRG was first described by Jaffe as lesion in mandible and maxilla. In 1980, Lorenzo and Dorfman coined the term ‘reparative’.
GCRG is a benign lesion usually found in facial bones. Small tubular bones of feet are infrequent site and pose difficulty in diagnosis Ackerman and Spjut in 1962 reported two cases of GCRG in small tubular bones of the hand. In foot, it is seen in tarsal bones followed by phalanges. In the present case GCRG is seen in distal phalanx of 4th toe, which is a rare site. Aetiology of this disease is unknown but in few of the cases history of trauma can be present. In the present case, patient denied any history of trauma [4-7].
Other giant cell containing lesions are Giant Cell Tumour of bone (GCTs), Aneurysmal Bone Cyst (ABC), chondroblastoma and brown tumour of hyperparathyroidism. Distinction between GCT and GCRG is difficult as they share clinical and radiological features. Histologically, GCT shows uniformly distributed osteoclast and mononuclear cells. However, in GCRG stroma is collagen rich and unevenly distributed osteoclastic giant cells with reactive bone formation is seen. Distinguishing solid variant of ABC and GCRG radiologically difficult they show lytic lesion which is expansile with thin cortex and multiple loculations. However, MRI shows cystic cavities filled with fluid in ABC, this feature is not always present. ABCs are located usually in long bones and vertebral column and rarely in small bones of hand and foot. Histologically, ABC shows cystic spaces filled with blood surrounded by osteoclast like multinucleated giant cells. However, in the present case there were no cystic spaces which were filled with blood. Distinction from chondroblastoma and GCRG is difficult as both of them show lytic lesions. Histologically, chondroblastoma shows sheets of polygonal cells showing nuclear indentation, grooving, chicken wire calcification of vessels and reactive giant cells which are characteristic of chondroblastoma. In the present case, these features were absent [1-4,5,8-11].
One of the closest differential diagnosis for GCRG is Brown tumour of hyperparathyroidism. It mimic’s GCRG both radiologically and histologically. Both the conditions show lytic lesions on X-ray and histopathologically giant cells and haemosiderin laden macrophages are seen. However, parathyroid hormones assay, serum calcium, phosphorus levels will help in differentiating these two conditions [6,10,12,13].
In the present case serum calcium and phosphorous values are under normal limits. Hence, the case was concluded as GCRG. The distinguishing features of these entities are presented in [Table/Fig-5].
Distinguishing features between giant cells lesions of bone.
| Features | GCRG | Giant cell tumour | Brown tumour of Hyperparathyroidism | Aneurysmal Bone Cyst | Chondroblastoma |
|---|
| Nature | Reactive | Benign | Metabolic | Benign | Benign |
| Age of presentation | 10-20 years | >25 years | 20-40 years | <25 years | <25 years |
| Sites | Maxilla and mandible | Ends of long bones, sacrum | Humerus, femur, tibia, maxilla | Any bone | Ends of long bones |
| Giant cells | Irregular distribution, clustering | Regular distribution, No apparent clustering | Irregular distribution, clustering | Variable size, clustering | Variable, smaller than GCT |
| Microscopy | Stroma is collagen rich and unevenly distributed osteoclastic giant cells with reactive bone formation | Uniformly distributed osteoclast and mononuclear cells | Osteoclastic giant cells embedded in stroma. Foamy cells, haemosiderin laden macrophages, reactive bone formation is seen | Cystic spaces filled with blood surrounded by osteoclast like multinucleated giant cells | Sheets of polygonal cells showing nuclear indentation, grooving, chicken wire calcification of vessels and reactive giant cells |
Usually enucleation and curettage is the treatment for GCRG. Recurrence rate by this method is 33-75%. Complete surgical excision has lower recurrence rate but there is loss of function. In the present case, the complete excision of tumour was done and there was no evidence of recurrence after 6 months of follow-up.
Conclusion
The present case illustrated diagnostic difficulty encountered due to its unusual location that was distal phalanx. Therefore, differential diagnosis of GCRG should be kept in mind for lytic lesions of metaphyseal-phalangeal swellings present in young patient. Complete resection of the lesion was curative treatment. Close follow-up of the patient is required since recurrence is common in GCRG.
[1]. Cm H, Norzila AB, Usm MMR, Giant cell reparative granuloma mimicking aneurysmal bone cyst in proximal phalanx of toeMalays ortho J 2016 10(1):55-56.10.5704/MOJ.1603.01128435549 [Google Scholar] [CrossRef] [PubMed]
[2]. Perkins A, Izadpanah A, Meng HS, Bernard C, Williams HB, Facs F, Giant cell reparative granuloma of the proximal phalanx: A case report and literature reviewCan J Plast Surg 2011 19(2):19-21.10.1177/229255031101900205 [Google Scholar] [CrossRef]
[3]. Ackerman LV, Spjut HJ, Giant cell reaction in tumours of bones and cartilage. In: Spjut HJ, Dorfman HD, Fechner RE, Ackerman LVAtlas of Tumour Pathology 1962 WashingtonArmed Forces Institute of Pathology:282 [Google Scholar]
[4]. Dahlin DC, Unni KK, Benign Giant Cell Tumour (Osteoclastoma). In Dahlin DC, Unni KK (eds)Bone Tumours. General Aspects and Data on 8542 Cases 1986 Springfield, ILCharles C. Thomas:119-140. [Google Scholar]
[5]. Pogrel AM, The diagnosis and management of giant cell lesions of the jawsAnn Maxillofac Surg 2012 2(2):102-06.10.4103/2231-0746.10132523482697 [Google Scholar] [CrossRef] [PubMed]
[6]. De Corso E, Politi M, Marchese MR, Pirronti T, Ricci R, Paludetti G, Advanced giant cell reparative granuloma of the mandible: radiological features and surgical treatmentActa Otorhinolaryngol Ital 2006 26(3):168-72. [Google Scholar]
[7]. Forouhar FA, Phelan NP, Benton DC, Giant cell reparative granuloma of the small bones of the hands and feet: A report of three casesAnn Clin Lab Sci 2000 30(3):272-77. [Google Scholar]
[8]. Lorenzo JC, Dorfman HD, Giant-cell reparative granuloma of short tubular bones of the hands and feetAm J Surg Pathol 1980 4:551-63.10.1097/00000478-198012000-000067212148 [Google Scholar] [CrossRef] [PubMed]
[9]. Campanacci M, Baldini N, Boriani S, Sudanese A, Giant-cell tumour of boneJ Bone Joint Surg 1987 69A:106-14.10.2106/00004623-198769010-00018 [Google Scholar] [CrossRef]
[10]. Schajowicz F, Giant Cell Tumour. In Schajowicz F (1sted)Tumours and Tumour-Like Lesions of Bone. Pathology, Radiology and Treatment 1990 BerlinSpringer- Verlag:257-295. [Google Scholar]
[11]. Cook DL, Rosenthal DC, Shikoff MD, Giant cell reparative granuloma of the middle phalanx of the foot: a review and case reportJ Foot Ankle Surg 2008 47(6):589-93.10.1053/j.jfas.2008.07.00119239873 [Google Scholar] [CrossRef] [PubMed]
[12]. Kamoun K, Sellami T, Jlailia Z, Abid L, Jenzri M, Bouaziz M, Giant cell reparative granuloma of the hallux following enchondromaPan Afr Med 2015 22:01-05.10.11604/pamj.2015.22.363.830926985281 [Google Scholar] [CrossRef] [PubMed]
[13]. Murphey MD, Nomikos GC, Flemming DJ, Gannon FH, Temple HT, Kransdorf MJ, From the archives of AFIP. Imaging of giant cell tumour and giant cell reparative granuloma of bone: radiologic-pathologic correlationRadiographics 2001 21(5):1283-309.10.1148/radiographics.21.5.g01se25128311553835 [Google Scholar] [CrossRef] [PubMed]