Pulmonary Artery Hypertension (PAH) is a haemodynamic and pathophysiological condition defined as an increase in mean Pulmonary Artery Pressure (PAP)> 25 mm Hg at rest and ≥ 30 mm Hg during exercise, as assessed by right heart catheterization [1]. It can be primary or secondary. In contrast to primary PAH which is a diagnosis of exclusion, secondary PAH is caused by various conditions most common being cardiac diseases, respiratory diseases or both co-existing. Among the less common causes are connective tissue diseases, haemoglobinopathies like sickle cell anaemia, infections like HIV, metabolic disorders like Glycogen storage diseases, drugs, toxins, thyroid dysfunction etc., [2].
A study suggested an increased incidence of thyroid dysfunctions (hypothyroidism and hyperthyroidism) as one of the reversible causes of PAH and it has been kept under WHO Group V of Dana Point, 2008 Classification of PAH [3]. PAH secondary to thyroid dysfunction is found to be reversible by restoration of euthyroid state i.e., they have a good prognosis if diagnosed and treated timely [1]. There are a lot of patients of thyroid dysfunction who have unexplained dyspnoea and the underlying cause maybe PAH. Hence, the purpose of our study was to observe the prevalence of PAH in newly diagnosed, treatment naïve patients of thyroid dysfunction (both hypo and hyperthyroidism) using 2D-echocardiographic assessment and to assess the reversibility of PAH with treatment, to be documented with 2D-echocardiography.
Materials and Methods
This observational prospective study included 67 inpatients and outpatients who came to Lok Nayak Hospital, New Delhi between the duration of November 2013 to April 2015.
Study Population Calculation:
The formula used to calculate sample size is as follows;
3.84 * pq/r2
Where,
p = prevalence
q = 1- prevalence
and r = allowable error
Keeping a level of significance at 95% (α=0.05) and power of study (1-β) at 80%, with absolute error of 10% as acceptable, the minimum sample size calculated is 67 (using Epi Info version 6.0, CDC, Atlanta).
Inclusion Criteria: This included individuals with age ≥ 12 years of age and patients who were diagnosed to have thyroid dysfunction by fT3 (normal value 3.5- 7.8 pmol/L), fT4 (normal value 9 – 25 pmol/L) and TSH levels (normal S.TSH levels - 0.4-5.5 mIU/L). Hypothyroidism was diagnosed with TSH >5.5 mIU/L and fT3 and fT4 below the normal limit as mentioned. Hyperthyroidism was diagnosed with TSH < 0.4 mIU/L with fT3 and fT4 above the upper normal value as mentioned above.
Exclusion Criteria: Individuals with pre-existing cardiovascular disease or symptomatic heart failure at presentation, any history of pulmonary thromboembolism or chronic pulmonary disease like COPD, presence of autoimmune connective tissue diseases like SLE, Rheumatoid disease etc., critically ill patients and patients with severe hepatic and renal dysfunctions were excluded from the study.
Patient’s data was prospectively collected and included detailed history, clinical examination, Electrocardiography (ECG), chest X-ray, laboratory results including serum fT3, fT4, TSH, anti TPO antibodies and ANA levels.
Ethical Considerations: The study protocol was approved by local research ethics committee and an informed consent was obtained from all participants.
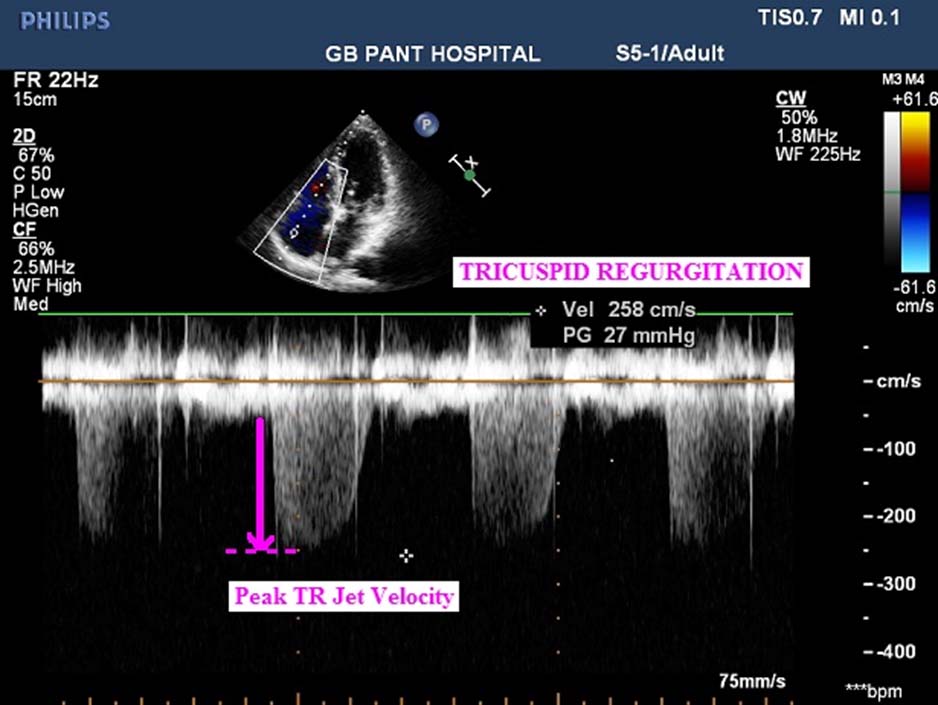
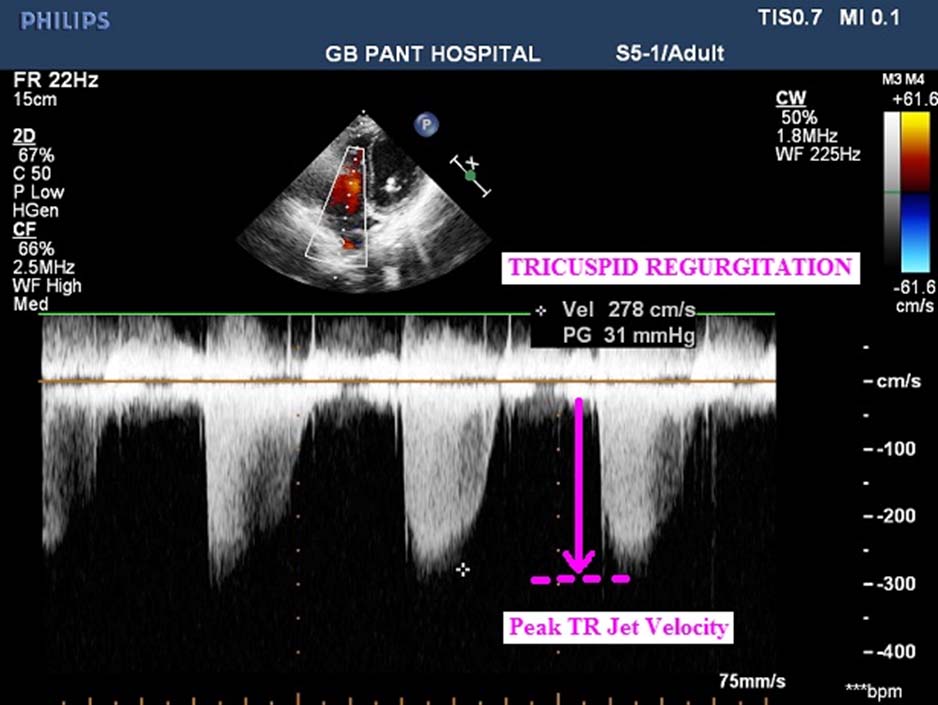
Echocardiographic Examination: All the patients underwent 2-D echocardiographic assessment in which various parameters were taken into account like presence or absence of tricuspid regurgitation and pulmonary regurgitation, size of right heart chambers, presence of pericardial effusion, pulmonary artery systolic pressure and right ventricular systolic pressure. PASP determined by measuring the peak systolic pressure gradient from the right ventricle to the right atrium was calculated using the modified Bernoulli equation [4]:
PASP = RVSP = 4(TVR)2+ RAP
Where, TVR is the maximum velocity of the tricuspid valve regurgitant jet, measured by continuous wave Doppler, added to the estimated Right Atrial Pressure (RAP).
Classification of PAH on the basis of PASP [4]:
Mild - PASP = 25-49 mm Hg
Moderate - PASP = 50-69 mm Hg
Severe - PASP ≥ 70 mm Hg
Statistical Analysis
The data collected was coded and entered into MS Excel software 2007. Analysis was carried out using SPSS-20.0 software. The statistical analysis was carried out to determine the association of PAH with thyroid dysfunction using student’s t-test and chi-square test of association. A p-value /of <0.05 was kept as significant.
Results
Study Population: In the study, the age of presentation of patients with thyroid dysfunctions ranged from 17-70 years with the mean age being 34.25±10.27 years. Most (84%) of the patients were female. Among them, 54 (80.6%) patients were hypothyroid and 13 (19.4%) patients were hyperthyroid.
Among the hypothyroid individuals (54 patients), the mean value of TSH was 105.41 mIU/L, mean fT3 was 5.93 pmol/L and mean fT4 was 10.71 pmol/L. Among the hyperthyroid patients (13 patients), mean TSH was 0.051 mIU/L, mean fT3 was 101.04 pmol/L and mean fT4 was 20.62 pmol/L.
Clinical and Echocardiographic Features: Out of the 67 patients, 25 patients (37.3%) were observed to have cardiovascular manifestations. The spectrum of cardiovascular manifestations were PAH in 19 patients (28.3%), Pericardial Effusion (PE) in 9 (13.4%), Dilated Cardiomyopathy (DCMP) in 5 (7.5%), arrhythmias in 4 (5.9%) and Pulmonary Regurgitation (PR) in 2 (3%). Out of the 4 patients with arrhythmias, 3 had atrial fibrillation while 1 had Paroxysmal Supraventricular Tachycardia (PSVT).
Pulmonary Artery Hypertension in Thyroid Dysfunctions: In the study, 19 patients (28.3%, 13 hypothyroid and 6 hyperthyroid) had evidence of pulmonary artery hypertension on echocardiographic assessment as calculated by using the modified Bernoulli equation.
Fatigue was the most common symptom [Table/Fig-1]. ECG changes were present in 36.8% patients and Chest Radiograph changes were seen in about 26.3% patients, in which cardiomegaly was present in 9 (13.4%) patients.
Clinical presentation of PAH patients.
| Presenting complaint | No. of patients | Percentage |
|---|
| Dyspnoea | 8 | 42.1 |
| Fatigue | 17 | 89.5 |
| Chest pain | 7 | 36.8 |
| Syncope | 5 | 26.3 |
| Peripheral oedema | 7 | 36.8 |
| Palpitations | 3 | 15.8 |
In the echocardiographic assessment, Tricuspid Regurgitation (TR) (100%), PE (26%), dilatation of Right Heart (RH) chambers (21%), reduced Left Ventricular Ejection Fraction (LVEF) (16%) and Pulmonary Regurgitation (PR) (5%) were the main findings recorded [Table/Fig-2]. When graded according to severity of PAH (based on PASP), 84% patients had mild PAH, 16% patients had moderate PAH and severe PAH was seen in none of the patients. Images of 2D-echo of few patients are depicted in [Table/Fig-3,4].
Echocardiographic findings in PAH patients.
| Echocardiographic findings | No. of patients | Percentage |
|---|
| TR | 19 | 100 |
| PE | 5 | 26.3 |
| Dilatation of right heart chambers | 4 | 21 |
| Reduced LVEF | 3 | 15.8 |
| PR | 1 | 5.3 |
(Tricuspid Regurgitation (TR); Pericardial Effusion (PE); dilatation of Right Heart (RH) chambers; reduced Left Ventricular Ejection Fraction (LVEF); Pulmonary Regurgitation (PR)
Echocardiogram of one of the patients showing peak TR jet velocity (pink arrow) and estimation of pulmonary artery systolic pressure.
Echocardiogram of one of the patients showing peak TR jet velocity and estimation of pulmonary artery systolic pressure.
No correlation could be established between S.TSH levels and PASP-values in both hypothyroid as well as hyperthyroid groups {Pearson’s correlation coefficient in hypothyroid group (r = -0.054) and hyperthyroid group (r = -0.109)}.
Out of the 67 patients, anti TPO antibodies was positive (>35 IU/L) in 26 (38.8%) patients. In the PAH patients’ group, 11 (57.8%) out of 19 patients and in the non-PAH patients’ group, 15 (31.2%) out of 48 patients had positive anti TPO antibodies. Applying chi-square test to the data, keeping degree of freedom as 1, Pearson’s chi-square coefficient is 4.069 with a p-value of 0.044 (<0.05) which is significant. It favours the role of an autoimmune mechanism in development of PAH in thyroid dysfunctions.
Hence, it was inferred from this study that development of PAH in thyroid dysfunctions may have an autoimmune basis, though further studies are needed to substantiate this conclusion with a larger sample size.
Prognostic Indicators:
Pericardial effusion: Pericardial effusion was present in 5 (26.3%) out of 19 patients having PAH.
TAPSE: TAPSE (tricuspid annular plane systolic excursion), an indicator of right ventricular function, was significantly reduced in only 1 patient having PAH. The mean of TAPSE was comparable in the PAH and non-PAH group of patients and no conclusion could be drawn on the significance of TAPSE in prognosis of PAH in the study.
Right Heart Catheterization: Right heart catheterization was carried out in 1 patient after taking written consent. Right femoral vein was used to make access and following observations were made.
Pulmonary artery systolic pressure = 25 mm Hg
Pulmonary artery diastolic pressure = 7 mm Hg
Mean pulmonary artery pressure = 14 mm Hg
Discussion
Cardiovascular manifestations are frequently seen in both hypothyroidism and hyperthyroidism. The spectrum of CVS manifestations in thyroid dysfunctions includes pulmonary artery hypertension, pericardial effusion, DCMP, arrhythmias, systolic as well as diastolic dysfunction and pulmonary regurgitation [5]. In our study, out of the 67 patients, 25 (37.3%) patients were found to have cardiovascular manifestations, which included 18 (33.3%) out of 54 patients of hypothyroidism and 7 (53.8%) out of 13 patients of hyperthyroidism. A comparison of data obtained in our study with review of literature is done in [Table/Fig-5] [6-10].
Review of literature regarding comparison of echocardiographic findings with other studies [6-10].
| Echo finding | Merce J et al., [6] | Ansari SM et al., [7] | Hardisty CA et al., [8] | Gupta A et al., [9] | Rawat B et al., [10] | Current study |
|---|
| PAH | 41% | - | - | - | - | 28.3% |
| PE | - | - | 32.5% | 45.5% | 72% | 13.4% |
| Arrhythmia | - | - | - | - | - | 5.9% |
| PR | 23% | - | - | - | - | 3% |
| Chamber enlargement | - | 19.1% | - | - | - | 5.9% |
| Systolic Dysfunction | 39% | 2.1% | - | - | - | 7.5% |
Pulmonary artery hypertension has been associated with both, hyperthyroidism and hypothyroidism, but primarily with hyperthyroidism [11]. PAH secondary to thyroid dysfunctions is found to be reversible by restoration of euthyroidism i.e., the patients have a good prognosis if diagnosed and treated timely. In our study, 19 patients (28.3%) had evidence of pulmonary artery hypertension on echocardiographic assessment. This is comparable with the data obtained by Curnock AL et al., and Li JH et al., in their respective studies, as shown in [Table/Fig-6] [12-18].
Comparison of prevalence of PAH in thyroid dysfunctions in various studies [6,12-18].
| Name of study | Prevalence of PAHPAH |
|---|
| Armigliato M et al., [12] | 65% |
| Curnock AL et al., [13] | 22.5% |
| Li JH et al., [14] | 24% |
| Marvisi M et al., [15] | 35% |
| Marvisi M et al., [16] | 43% |
| Merce J et al., [6] | 41% |
| Reddy BH et al., [17] | 56% |
| Siu CW et al., [18] | 47% |
| Current study | 28.3% |
There are not many studies done in past to determine the prevalence of PAH in thyroid dysfunctions. All the studies done so far are based on 2D-echocardiography. The gold standard investigation, right heart catheterization, is invasive and was not included in any of the studies. Our study was conducted to determine the occurrence of PAH in patients of thyroid dysfunctions on the basis of echocardiographic assessment. Right heart catheterization was done in only one patient who consented, to confirm the presence of PAH.
In our study, PAH secondary to thyroid dysfunctions was more prevalent in females (84%) with a mean age of presentation of 34.3±10.70 years. PAH was seen to be present in total 19 (28.3%) patients with thyroid dysfuction (total 67). Out of 54 hypothyroid patients, 13 (24%) had PAH. In the hyperthyroid group, out of 13 patients, 6 (46%) had developed PAH. Majority of them had mild (84%) PAH, 16% patients developing moderate PAH and none of them having severe PAH. Repeat echocardiography after 6 months of treatment was performed in 7 of the 19 patients diagnosed with pulmonary artery hypertension and reduction in PASP was observed in 3 of them.
The development of PAH in a patient of thyroid dysfunction was not affected by its type (p-value 0.113) or the serum TSH levels in the study. Autoimmunity seems to have a role in the development of PAH in thyroid dysfunctions, as observed in the study by raised anti TPO levels [19].
Limitation
The study has its shortcomings. The sample size recruited was small. Most of the patients did not give consent for right heart catherization, which is the most precise method for calculation of PASP. Moreover, it is a one-time study and hence actual follow up of patients to check for decrease and/or resolution of PAH has not been done in a calculative manner after achieving euthyroid state.
Conclusion
Hence, our study showed that PAH is present in about one-fourth (28.3%) of the patients of thyroid dysfunction, which was mostly mild (84%) with only 16 % developing moderate and none severe PAH. It is more prevalent in females with a mean age of 34.3+10.70 years. Cardiovascular manifestations were present in 37.3% of the patients with thyroid dysfunction. The development of PAH was not affected by TSH levels in this study. Autoimmunity might play a role in the development of PAH as evidenced by raised levels of TPO in our study.
While further research is needed based on larger sample size, our study indicates the need of thyroid function tests to be considered in every patient of idiopathic PAH, so that timely institution of medications can prevent and treat PAH and cardiovascular manifestations in these patients along with a follow up to assess for reversibility in PAH.
(Tricuspid Regurgitation (TR); Pericardial Effusion (PE); dilatation of Right Heart (RH) chambers; reduced Left Ventricular Ejection Fraction (LVEF); Pulmonary Regurgitation (PR)