Diabetes mellitus is amongst the most prevalent ailments manifesting high morbidity and affecting significant human population worldwide. Patient with diabetes are at much higher risk for development of both microvascular and macrovascular complications, including peripheral neuropathy, nephropathy, retinopathy, and cardiovascular disease [1]. Neuropathy is the most common long term complication of diabetes, which affect upto 50% of patients with longstanding disease [2].
Diabetic neuropathy consists of a family of neurological syndromes that affect specific regions of the nervous system, occurring in both Type 1 and Type 2 diabetes mellitus [2]. Chronic hyperglycaemia leads to functional and structural disturbances in microvascular system, increases oxidative stress, and adversely affects glycosylation of axonal and microvascular proteins and trophic factors needed for peripheral nerves and their ganglia [3].
Approximately 15% of patients with DM develop foot ulcer during their lifetime, of which 70% have a neuropathic origin [4,5]. Screening of patients with neuropathic pain and its treatment is a first line prevention for diabetic foot ulcers [6]. On account of the high occurrence of debilitating condition of foot ulcer, early diagnosis of peripheral neuropathy and impact of duration of diabetes on peripheral neuropathy is significant. The present study aimed to determine the correlation of duration of diabetes with SNCV of median, ulnar, superficial peroneal and sural nerves.
Materials and Methods
The present cross-sectional study was conducted in Department of Physiology, in collaboration with Rajeev Gandhi Centre for Diabetes and Endocrinology on patients of T2DM attending Diabetes clinic in Jawaharlal Nehru Medical College Hospital (JNMCH), Aligarh Muslim University from December 2014 to May 2016 after approval from the Ethical Committee of JNMC. A total of 90 subjects were taken; among them 60 subjects were diagnosed cases of T2DM, which were divided in two groups on the basis of duration of diabetes.
Group A1=30 T2DM patients having diabetes duration less than 8 years,
Group A2=30 T2DM patients having diabetes duration more than 8 years,
Group A=Rest 30 subjects were non-diabetic (control group).
Sensory nerve conduction velocity study of bilateral median nerve, ulnar nerve, superficial peroneal nerve and sural nerve was done for assessing peripheral neuropathy.
The inclusion criteria of T2DM patients for the present study were, patients aged 30-69 years, diagnosed with diabetes on the basis of revised American Diabetic Association Criteria i.e., fasting plasma glucose ≥126 mg/dL (≥6.1 mmol/1) and 2 hours postprandial plasma glucose ≥200 mg/dL (≥1 1.1 mmol/1) [7]. The exclusion criteria of these patients were, presence of thyroid disease (hypo or hyperthyroidism), previous history of any systemic condition related to peripheral neuropathy (malnutrition, alcoholic neuropathy, renal failure), trauma in the course of nerve to be examined and neuropathies associated with exogenous toxins, metals, or drugs.
The control group for the present study included non-diabetic, healthy individuals with age, sex and BMI (Body Mass Index) matching with those of the diabetic group.
The SNCV study was conducted in median, ulnar, superficial peroneal and sural nerves using Neuroperfect EMG/NCV/EP SYSTEM (Medicaid systems, Chandigarh, 160002, India) apparatus assembly. The underlying principal of the study involves the application of depolarising square wave electrical pulses to the skin over a peripheral nerve, producing a propagated Nerve Action Potential (NAP) which is recorded at a distant point over the same nerve.
In the present study, the SNAP was recorded anti-dromically [Table/Fig-1].
Stimulation sites for recording SNAP.
| Nerve | Antidromic/Orthodromic | Stimulation Site | SNAP Recorded From |
|---|
| Median | Anti-dromic | Wrist | Index finger |
| Ulnar | Anti-dromic | Wrist | Little finger |
| Sural | Anti-dromic | Distal to lower border of gastrocnemius at the junction of middle and lower 1/3rd of the leg | Ankle |
| SPN | Anti-dromic | 10-15 cm proximal to the upper edge of lateral malleolus anterior to peroneus longus. | Ankle |
Stimulation sites for recording SNAP.
Stimuli were supra-maximal and of 0.1 ms duration at a frequency of 1 Hz. The filter setting for sensory conduction was 20 Hz-3 KHz, sweep speed was 2 ms/division. The SCV was calculated by dividing the distance (mm) between the stimulating and recording sites by the latency (ms).
SNCV=Distance/Latency (m/s):Statistical Analysis
Statistical analysis was performed using SPSS version 21.0. Continuous variables were expressed as Mean±Standard deviation (SD) or range, and qualitative data was expressed in percentages. One-way ANOVA with Post-Hoc Tukey test were used for comparison of means between three groups. The association between continuous variables was tested by linear correlation using Pearson’s coefficient. A p-value of <0.05 was considered significant.
Results
The baseline characteristics (age, sex, BMI, Blood pressure) of non-diabetic control group (Group A), patients with less than eight years T2DM (Group A1) and patients with more than eight years T2DM (Group A2) showed no significant differences amongst themselves [Table/Fig-2].
Baseline and other characteristics of all three groups.
| Variable | Group A (n=30) | Group A1 (n=30) | Group A2 (n=30) |
|---|
| Value (mean±SD) | Value (mean±SD) | Value (mean±SD) |
|---|
| n (male/female) | male 16 /female 14 | male 13 /female 17 | male 15 /female 15 |
| Age (years) | 52.50±7.31 | 51.23±7.99 | 58.33±6.45 |
| Duration of T2DM (years) | 0 | 3.31±1.72 | 12.8±4.42 |
| Weight(kg) | 62.37±10.43 | 64.63±10.37 | 63.87±9.43 |
| Height(m) | 1.56±0.10 | 1.59±0.10 | 1.58±0.09 |
| BMI(Kg/m2) | 25.48±2.68 | 25.68±3.82 | 25.43±3.10 |
| Waist/hip ratio | 0.87±0.09 | 0.99±0.07 | 0.97±0.09 |
| Systolic BP (mmHg) | 129.67±9.23 | 127.13±8.11 | 126.76±6.27 |
| Diastolic BP (mmHg) | 81.87±5.53 | 81.33±3.21 | 81.87±3.52 |
| Fasting Plasma glucose (mg/dL) | 101.87±5.87 | 136.3±27.16 | 151.53±32.73 |
| Post prandial glucose (mg/dL) | 128.43±6.70 | 198.5±35.29 | 222.2±37.93 |
| HbA1C (%) | 5.97±0.24 | 7.4±2.35 | 8.16±2.15 |
BP: Blood pressure
The results obtained from the SNCV study done for left and right-side nerves were near-identical. Therefore, for the sake of brevity, only right-side nerve’s test results have been described.
In SNCV test, among 30 patients of less than eight years duration of diabetes, 9 (30%) patients had normal SNCV of all the four nerves. In the rest 21 (70%) patients, decrease in SNCV was observed. 9 (30%) patients had decrease in SNCV of only one nerve, namely ‘Sural nerve’, 10 (33%) patients had decrease in SNCV of two nerves, namely the ‘Sural’ and ‘Superficial Peroneal Nerve’ (SPN) nerves, and 2 (7%) patients had decrease in SNCV of all the four nerves (Median, Ulnar, SPN and Sural nerves) [Table/Fig-3].
Sensory nerve conduction velocity study of 30 patients-less than 8 years of T2DM.
| S. No. | Observation | No. of patients |
|---|
| 1 | No impact-normal SNCV | 9 |
| 2 | Decrease in SNCV of one (Sural) nerve | 9 |
| 3 | Decrease in SNCV of two (Sural and SPN) nerves | 10 |
| 4 | Decrease in SNCV of all four nerves (Median, Ulnar, SPN and Sural Nerve) | 2 |
| Total | 30 |
In the patients of more than eight years duration of diabetes, 12 (40%) patients had decrease in SNCV of all the four nerves (Median, Ulnar, SPN and Sural), rest 18 (60%) patients had decrease in SNCV of Sural nerve and SPN. These are given in [Table/Fig-4].
Sensory nerve conduction study of 30 patients-more than 8 years of T2DM.
| S. No. | Observation | No. of patients |
|---|
| 1 | No impact-normal SNCV | 0 |
| 2 | Decrease in SNCV of one (Sural) nerve | 0 |
| 3 | Decrease in SNCV of two (Sural and SPN) nerves | 18 |
| 4 | Decrease in SNCV of all four nerves (Median, Ulnar, SPN and Sural Nerve). | 12 |
| Total | 30 |
There was statistically significant difference in means of SNCV of median, ulnar, SPN and sural nerve between the three groups as shown in [Table/Fig-5].
Comparison of means of SNCV between all three groups.
| Sensory Nerve Conduction Velocity according to Mean Duration of T2DM |
|---|
| Sensory Nerve Conduction in groups (each N=30) with different Mean Duration of T2DM years | ANOVA | p-value# |
|---|
| Group A (No Diabetes) | Group A1 (3.31±1.72) | Group A2 (12.8±4.42) | F-value | p-value | Group A vs A1 | Group A vs A2 | Group A1 vs A2 |
|---|
| Median Nerve | 52.12±4.76 | 51.63±4.59 | 44.29±5.36 | 18.75 | 0.001* | 0.46 | 0.001* | 0.001* |
| Ulnar Nerve | 56.29±4.94 | 50.88±4.34 | 48.63±4.99 | 20.44 | 0.001* | 0.001* | 0.001* | 0.166 |
| SPN Nerve | 51.21±3.01 | 45.17±3.51 | 35.86±6.14 | 90.89 | 0.001* | 0.001* | 0.001* | 0.001* |
| Sural Nerve | 51.47±3.38 | 35.00±10.00 | 24.72±7.59 | 96.93 | 0.001* | 0.001* | 0.001* | 0.001* |
*p-value <0.05 is significant; #: Post-Hoc Tukey Test
Variation in mean between non-diabetic and less than eight years diabetic in B/L median nerve SNCV was not significant, whereas in ulnar, SPN, sural nerves, the said variation in mean was found to be significant. Variation in means between non-diabetic and more than eight years diabetic is significant in all the four nerves. Variation in mean between less than eight years diabetic and more than eight year diabetic was not significant in ulnar nerve, whereas it was significant in rest all the three nerves as shown in [Table/Fig-5].
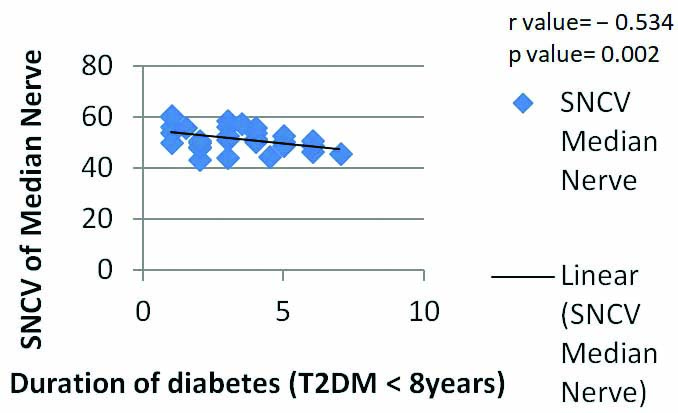
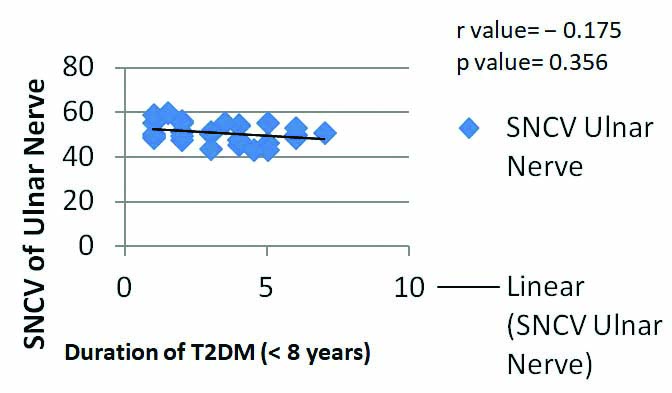
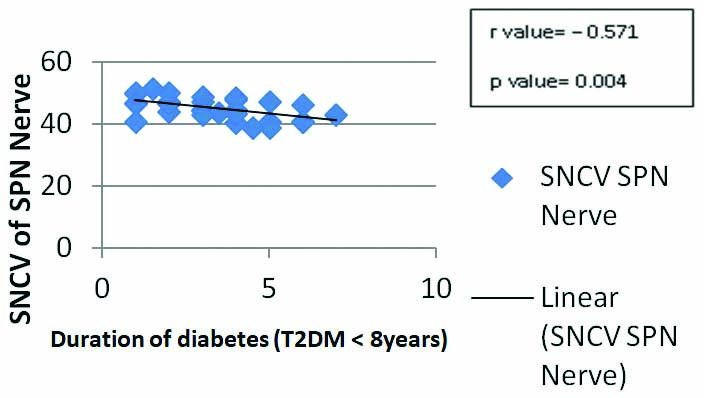
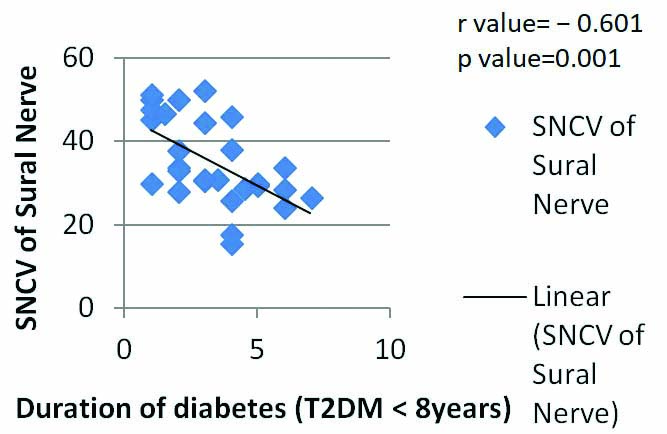
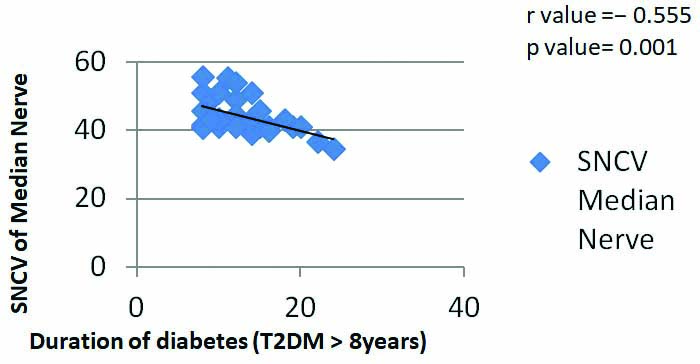
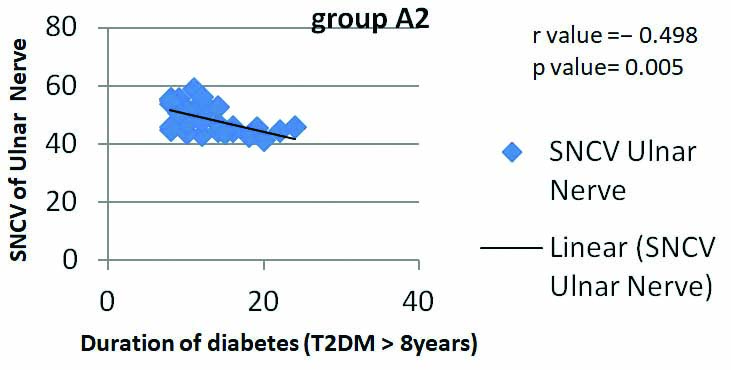
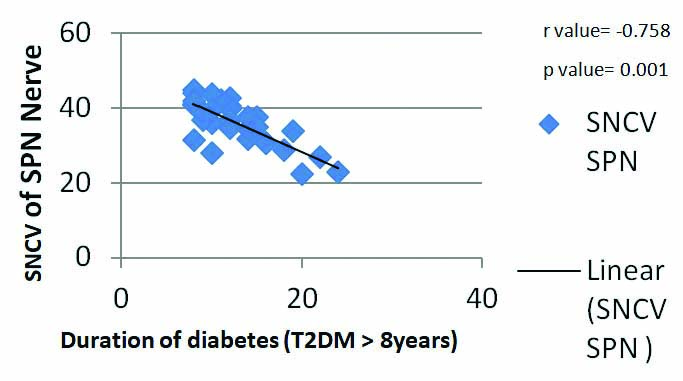
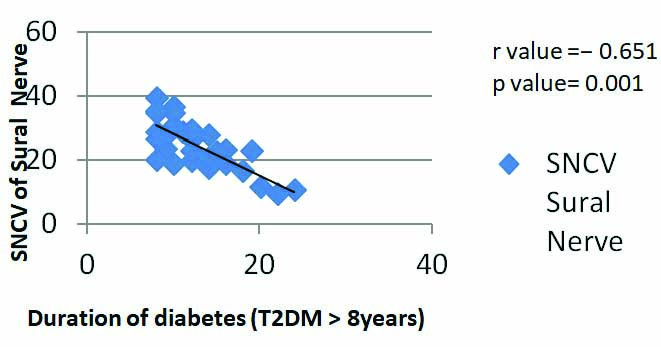
In the study group of duration less than 8 years diabetes, there was significant negative correlation between the duration of diabetes and SNCV values of sural, SPN, and median nerves respectively, whereas, correlation between SNCV values of ulnar nerve and duration of diabetes was not significant [Table/Fig-6,7,8 and 9]. However, in the study group of more than eight years diabetes, there was significant negative correlation between the duration of diabetes and SNCV of all the four nerves [Table/Fig-10,11,12 and 13].
Correlation of duration of type 2 diabtes with SNCV of Median Nerve in Group A1.
Corelation of duration of diabetes with SNCV of Ulnar Nerve in Group A1.
Correlation of duration of type 2 diabtes with SNCV of SPN Nerve in Group A1.
Correlation of duration of type 2 diabtes with SNCV of Sural Nerve in Group A1.
Correlation of duration of type 2 diabtes with SNCV of Median Nerve in Group A2.
Correlation of duration of type 2 diabtes with SNCV of Ulnar Nerve in Group A2.
Correlation of duration of type 2 diabtes with SNCV of SPN Nerve in Group A2.
Correlation of duration of type 2 diabtes with SNCV of Sural Nerve in Group A2.
Discussion
The present study was undertaken to determine the correlation of duration of diabetes with SNCV of median, ulnar, superficial peroneal and Sural nerves. A related study in the past has indicated that both sensory and motor nerve conduction serve as a useful modality for detecting diabetic neuropathy in sub-clinical diabetes [8]. Another study has concluded that diabetic Neuropathy Symptom Score (NSS) and Neuropathy Disability Score (NDS) can help in evaluation of diabetic sensori-motor polyneuropathy though nerve conduction study is more powerful test and can help in diagnosing cases of neuropathy [9]. The data of the present study show that there was no significant difference in baseline characteristic of all three groups as shown in [Table/Fig-2]. It was also observed in present study that SNCV of all four nerves was normal in as much as 30% of less than 8 years T2DM patients [Table/Fig-3], whereas none of the patients with more than 8 years T2DM patients demonstrated normal SNCV [Table/Fig-4]. This clearly shows that with increasing duration of diabetes, involvement of number of nerves increases as also stated in the study [10]. It was also noted from the present study that isolated involvement of only median or ulnar was not seen. Instead, their involvement was always in conjugation with lower limb nerves (Sural and SPN) [Table/Fig-3,4].
It was also evident that sensory neuropathy is present even in shorter duration T2DM patients [Table/Fig-3]. This finding is consistent with the finding of Halar EM et al., study in which it is seen that, in diabetic subjects, before treatment average Nerve Conduction Velocity (NCV) of the median, peroneal sural, and tibial nerves and H-reflex latency results were all significantly impaired (p<0.025) and there was no difference found between right and left NCVs of the same nerve (p<0.05) and NCVs in the lower as well as the upper extremities were significantly reduced (p<0.05) [11].
The present study also shows that overall variance of SNCV of all four nerves between the three groups was statistically significant [Table/Fig-5]. It was also seen that, when compared with control group, in shorter duration of T2DM, sensory NCV was significantly reduced in lower limb (sural nerve and superficial peroneal nerve) and while upper limb (median nerve) shows reduced SNCV but not to significant levels [Table/Fig-5]. However, in patients with longer duration of T2DM when compared with control group both lower limb and upper limb SNCV shows significant decrease. When both the groups are compared with each other, there was significant decrease in SNCV of median, SPN and sural nerve, while there was not significant decrease in ulnar nerve. This shows that sensory neuropathy first affects the lower limb and subsequently other body part and upper limbs [12,13].
Sensory Nerve Conduction Velocity is a very sensitive test as shown in the study by Liu MS et al., who supports the fact, that sub-clinical neuropathy can be detected by nerve conduction studies [14].
There is significant negative correlation between SNCV Median, SPN and Sural nerve in less than eight year T2DM group whereas there is significant correlation between SNCV of all the four nerves and duration of diabetes in more than eight-year group [Table/Fig-6,7,8,9,10,11,12 and 13]. Thus, it appears that decrease in SNCV commences early with the onset of the disease and the effect becomes more pronounced with the progression of diabetes. The association between the duration of diabetes mellitus and neuropathy was also evident in a research study on the epidemiology of diabetic complications [15]. So screening early diagnosis and intervention can be done to prevent the progression of neuropathy in diabetes patients.
Limitation
The limitation of the present study was that it covers relatively small number of diabetic patients. So, future recommendation study should include more number of diabetic patients, as well as follow-up study can be done to observe the effect of lifestyle and treatment intervention on neuropathy progression.
Conclusion
In conclusion, lower limb nerves (i.e., sural and SPN nerves) are the first to be affected and upper limb nerves are not impacted in isolation. Also, there is significant impact of duration of diabetes on SNCV. Sensory impairment is also seen in cases of shorter duration of diabetes. So, it is recommended to incorporate SNCV studies as part of early screening test of peripheral neuropathy in T2DM to prevent the debilitating complications arising out of sensory neuropathy.
BP: Blood pressure
*p-value <0.05 is significant; #: Post-Hoc Tukey Test