Sesamoid Bones in the Soft Tissue of Neck as Incidental Finding on Multidetector Computed Tomography
Gitanjali Khorwal1, Rahul Dev2, Pankaj Sharma3
1 Assistant Professor, Department of Anatomy, All India Institute of Medical Sciences, Rishikesh, Uttarakhand, India.
2 Assistant Professor, Department of Radiodiagnosis and Imaging, All India Institute of Medical Sciences, Rishikesh, Uttarakhand, India.
3 Assistant Professor, Department of Radiodiagnosis and Imaging, Delhi State Cancer Institute, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Rahul Dev, Flat No.5/1, Building No.57, All India Institute of Medical Sciences, Rishikesh Residential Complex, Rishikesh-249202, Uttarakhand, India.
E-mail: rdev8283@gmail.com
Sesamoid ossicles are round to oval small bones, usually seen in relation to tendon of a muscle or a joint with less frequent occurrence at other locations. They are asymptomatic in the vast majority of cases; however, predispose to increased risk of injury. In a few other cases, they may present as a palpable mass accompanied by vague neck pain or stiffness. Rarely, these bony structures can be seen in close relation to ligamentum nuchae or paraspinal muscles and may predispose to pain in the neck. They are known to be stable in size over time and show no evidence of recurrence after surgical excision. Histologically, they are considered fibrocartilagenous tumour formed secondary to fibrocartilagenous metaplasia triggered by localised repetitive trauma or chronic mechanical stress. We report two cases where sesamoid ossicles were detected within the nuchal ligament. Only few cases of this entity lesion have been reported previously.
Ligamentum nuchae, Ossicle, Paraspinal
Case Report
Case 1
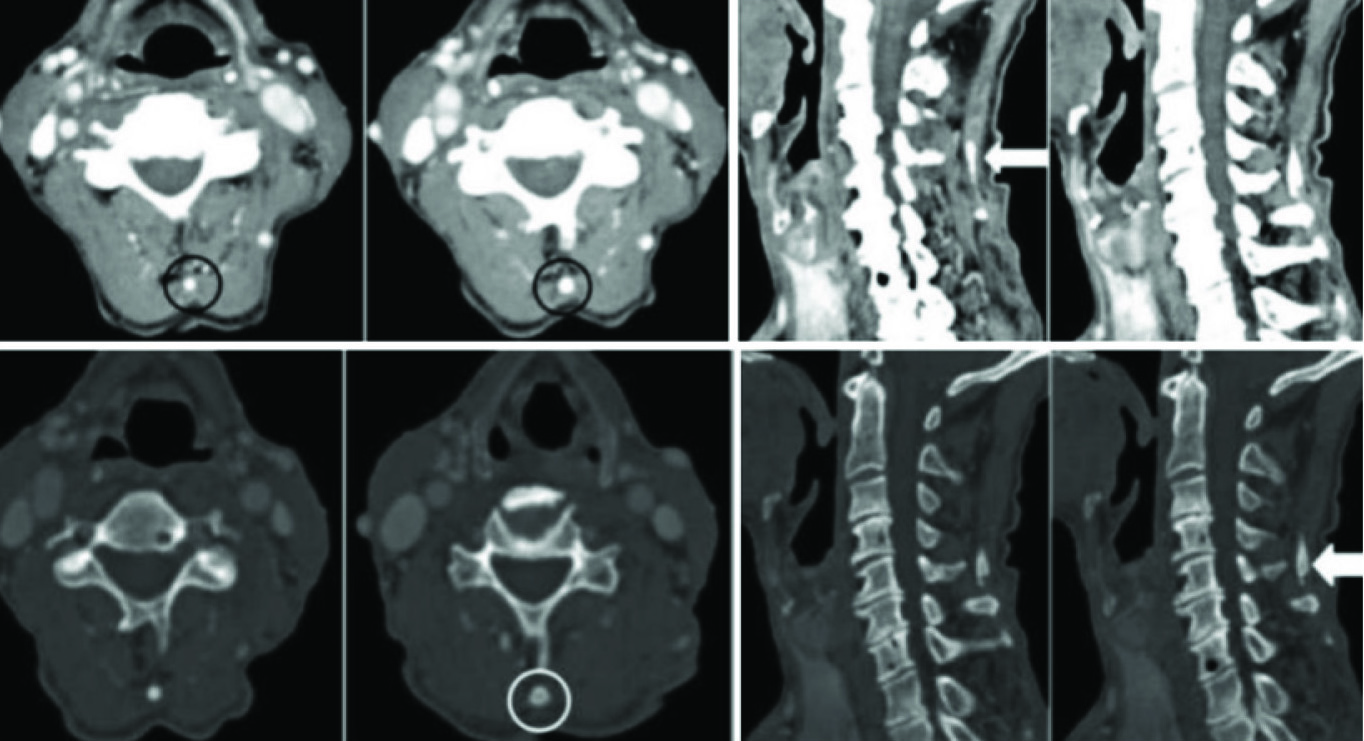
A 60-year-old male patient, known case of squamous cell carcinoma of oropharynx presented with complaints of pain in throat and prickly sensation. The patient complained of neck pain, stiffness and limitation of movement for the last 5-6 years. Subsequently, the patient underwent multidetector computed tomography of the neck for disease assessment. Axial and saggital reconstructed computed tomography images of neck showed longitudinally oriented oval ossified corticated focus posterior to spinous processes at level of superficial or funicular portion of ligamentum nuchae with background cervical spine showing degenerative changes [Table/Fig-1,2].
Axial and sagittal reconstructed computed tomography images of neck on both soft tissue and bone window show longitudinally oriented oval ossified corticated focus posterior to spinous processes of C5 vertebra at level of ligamentum nuchae (black and white circles and white arrows) with unremarkable adjacent soft tissue. The cervical spine shows advanced degenerative changes in the form of multilevel osteophytes and loss of disc spaces.
The bony focus as visualised on volume rendered three dimensional images (white arrows).

Case 2
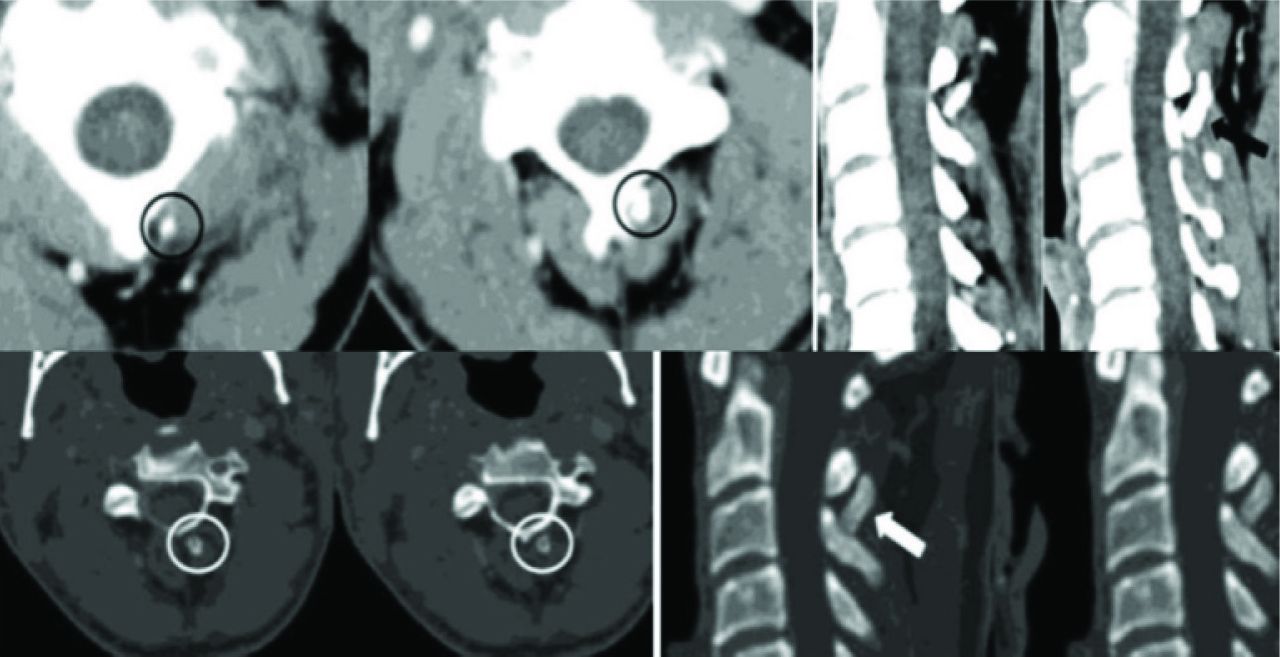
A 30-year-old male patient, known case of squamous cell carcinoma floor of mouth presented, having complaints of vague swelling and ulcerative growth on right side of the floor of mouth with vague pain and stiffness in neck for a 2 to 3 years duration underwent multidetector computed tomography of neck showing obliquely oriented oval corticated bony focus within deep or lamellar portion of the nuchal ligament with associated early degenerative changes cervical spine [Table/Fig-3,4].
Axial and sagittal reconstructed computed tomography images of neck on both soft tissue and bone window show obliquely oriented oval ossified corticated focus within ligamentum nuchae at level of C2 and C3 vertebral spinous processes (black and white circles and arrows) with no adjacent soft tissue changes. The cervical spine shows early degenerative changes in the form of multilevel anteroinferior vertebral marginal osteophytes.
The bony focus as visualised on volume rendered three dimensional images (white arrows).

Discussion
Sesamoid bones have been first described by Barsony T and Winkler K, in 1929 and histologically attributed as osteomas by Jutras in 1938 [1]. The terminology was derived from the seeds of Sesamum indicum plant. Sesamoid ossicles within the posterior neck musculature are seen as an incidental finding, invariably painless and solitary. Morphologically it is seen as well-defined round to oval corticated densities with a central area of lucency corresponding to marrow elements on computed tomography with both cases in the present study showing similar morphology. This entity was found to be about three times more common in males, most prominently seen around the third decade of life, localised to C5-C7 vertebral level in more than 80% cases attributed to higher mechanical stress as this is a high mobility region as postulated by Scapinelli R [2]. In the present study the ossicle was localised to C5 vertebral level in one of the case in correlation to the general frequency of occurrence. In the other case the ossicle was seen at C2-C3 vertebral level. These are believed to be originated within tendinous or ligamentous structures, however the exact aetiology of this entity was not clearly understood. These can have variable composition ranging from fibrous, cartilaginous, bony elements or a combination of any. Histologically these are postulated to be formed secondary to slow and gradual osseous metaplasia of cartilaginous elements triggered by mechanical stress [2]. In other studies it was also postulated that myositis ossificans is a closely related entity formed secondary to osseous metaplasia of connective tissue elements due to long standing mechanical injury [3]. The circumscripta type of myositis is frequently found to be localised at level of ligamentum nuchae and mistaken as sesamoid ossicles [4,5]. However, the multiplicity of lesions along with history of injury and pain in neck favours the former. In the present study, both cases were solitary with no history of trauma to cervical spine. An extremely rare case of secondary ossification centre of cervical spinous process mimicking sesamoid ossicle was reported by Fiandesio D and Quaglia C [6]. They also postulated association of hydroxyapatite deposition disease. There is a wide range of differentials of this entity which can be developmental as in overgrowth of ossification centres of vertebral elements, post-traumatic like spinous process fracture or myositis ossificans, post inflammatory diseases like lupus erythematosus, sarcoidosis or tendinitis, metabolic conditions like hyperparathyroidism, amyloidosis and fluorosis [1,7]. In vast majority of cases they remain asymptomatic, within a minor subset being asymptomatic and confused with post-traumatic changes of fracture or dislocation. In one study, 64 slice multidetector computed tomography was found to be best possible imaging modality for visualisation of posterior spinal elements [8]. Sesamoids were seen solitary in 82% cases and two sesamoids in 18% cases [2]. The nuchal ligament is a midline stabilising structure for neck serving multiple purpose including support and stabilisation of head, site for attachment of muscles, maintaining cervical curvature and preventing excessive cervical flexion. It has two separately identifiable portions comprising of anterior or deep bilayered lamellar portion with intervening contained fat and posterior or superficial fibrous funicular portion postulated to be posterior extension of lamellar portion. This bilayer configuration of lamellar portion provides basis for bloodless surgical plane [9]. Both the components are attached to external occipital protuberance superiorly and C7 spinous process inferiorly [9]. In the study by Wang H et al., and Kim DG et al., the prevalence of ligamentum nuchae ossification was found to be in nearly 50% cases with both studies showing higher prevalence in cases with cervical spondylosis, male gender and with advanced age with very few cases seen before third decade of life [10,11]. The present study is in accordance with both cases seen in elderly male patients with cervical spine showing degenerative changes. The prevalence of same was significantly less in a previous study, probably due to use of radiography alone [2]. Tsai YL et al., in their study showed a positive statistically correlation between ligamentum nuchae ossification and multiple clinical and radiographic parameters including cross-section area of cervical canal, active range of motion of cervical spine and associated secondary degenerative changes with most significant association seen with flexion-extension movements on clinical examination, uncovertebral osteophytes and canal dimensions [12]. The sesamoid ossicles of lower limbs are similar to that of neck region in terms of clinical presentation, radiological appearance and histological findings. On clinical, radiographical and histological grounds the nodules detectable in the ligamentum nuchae of man appear to be true sesamoid bones, similar to those commonly found in some tendons of the lower limbs. A closely related entity termed nuchal fibrocartilaginous pseudotumour was seen more commonly in young women having similar symptomatology, lesional level and histology as sesamoid ossicles. There was associated thickening of ligamentum nuchae [13,14].
Conclusion
The presence of sesamoid ossicles within nuchal ligament is invariably seen in patients having symptoms of chronic pain in cervical region signifying mechanical stress as key inciting factor, most frequently localised at C5-C6 vertebral level. They are more commonly seen in elderly male patients with cervical spine showing degenerative changes.
[1]. Paraskevas GK, Raikos A, Martoglou S, Ioannidis O, Sesamoid ossicles within the nuchal ligament: a report of two cases and review of the literatureJ Radiol Case Rep 2011 5(8):22-29.10.3941/jrcr.v5i8.70822470809 [Google Scholar] [CrossRef] [PubMed]
[2]. Scapinelli R, Sesamoid bones in the ligamentum nuchae of manJ Anat 1963 97(3):417-22. [Google Scholar]
[3]. Edeiken J, Hodes PJ, Roentgen diagnosis of diseases of bone 1967 BaltimoreWilliams & Wilkins [Google Scholar]
[4]. Noble TP, Myositis ossificans: a clinical and radiologicalstudyJ Surg Gynec Obst 1924 39:795 [Google Scholar]
[5]. Thomson JE, Myositis ossificans (circumscripta) in the ligamentum nuchaeAnn Surg 1934 100:279-83.10.1097/00000658-193408000-0000317856346 [Google Scholar] [CrossRef] [PubMed]
[6]. Fiandesio D, Quaglia C, Nuclei ossificanti aberrant delrachide cervicaleRadiol Med 1955 41:819 [Google Scholar]
[7]. Gokce E, Beyhan M, Evaluating ossifications of the nuchal ligament with cervical computed tomographyThe Eurasian Journal of Medicine 2018 50(1):23-27.10.5152/eurasianjmed.2018.1731429531487 [Google Scholar] [CrossRef] [PubMed]
[8]. Mellado JM, Larrosa R, Martín J, Yanguas N, Solanas S, Cozcolluela MR, MDCT of variations and anomalies of the neural arch and its processes: part 1-pedicles, pars interarticularis, laminae, and spinous processAm J Roentgenol 2011 197:W104-13.10.2214/AJR.10.580321700970 [Google Scholar] [CrossRef] [PubMed]
[9]. Kadri PA, Al-Mefty O, Anatomy of the nuchal ligament and its surgical applicationsNeurosurgery 2007 61(5 Suppl 2):301-04.10.1227/01.neu.0000303985.65117.ea18091243 [Google Scholar] [CrossRef] [PubMed]
[10]. Wang H, Zou F, Jiang J, Lu F, Chen W, Ma X, Analysis of radiography findings of ossification of nuchal ligament of cervical spine in patients with cervical spondylosisSpine (Phila Pa 1976) 2014 39:E7-E11.10.1097/BRS.000000000000043025504097 [Google Scholar] [CrossRef] [PubMed]
[11]. Kim DG, Oh YM, Eun JP, The clinical significance of ossification of ligamentum nuchae in simple lateral radiograph: a correlation with cervical ossification of posterior longitudinal ligamentJ Korean Neurosurg Soc 2015 58:442-47.10.3340/jkns.2015.58.5.44226713144 [Google Scholar] [CrossRef] [PubMed]
[12]. Tsai YL, Weng MC, Chen TW, Hsieh YL, Chen CH, Huang MH, Correlation between the ossification of nuchal ligament and clinical cervical disordersKaohsiung J Med Sci 2012 28:538-44.10.1016/j.kjms.2012.04.01623089319 [Google Scholar] [CrossRef] [PubMed]
[13]. O’Connell JX, Janzen DL, Hughes TR, Nuchal fibrocartilaginous pseudotumor: a distinctive soft-tissue lesion associated with prior neck injuryAm J Surg Pathol 1997 21(7):836-40.10.1097/00000478-199707000-000129236840 [Google Scholar] [CrossRef] [PubMed]
[14]. Laskin WB, Fetsch JF, Miettinen M, Nuchal fibrocartilaginous pseudotumor: a clinicopathologic study of five cases and review of the literatureMod Pathol 1999 12(7):663-68. [Google Scholar]