Thyroid disorders are the most common endocrine disorders affecting about 42 million people in India [1]. Among all the disorders LT is the second most common thyroid lesion diagnosed on cytology next to goiter [2].
“Strauma Lymphomatosa” a chronic disorder of the thyroid gland is characterized by diffuse lymphocytic infiltration, fibrosis, parenchymal atrophy and eosinophilic changes in some of the acinar cells (Hurthle cell change). The word LT is used synonymously with Hashimoto’s thyroiditis or autoimmune thyroiditis which is again subclassified as atrophic and non goitrous thyroiditis on histopathology [3].
LT typically presents with painless enlargement of thyroid gland, hypothyroidism, or both; 90% of LT patients also have High Anti-Thyroid Peroxidase (TPO) and anti-Thyroglobulin (Tg) antibodies [4].
On histopathology, the hallmark finding is lymphocytic infiltration of thyroid follicles resulting in glandular destruction, formation of lymphoid follicles and Hurthle cell changes [5]. Fine Needle Aspiration Cytology (FNAC) of thyroid provides a safe and accurate method for diagnosis with a sensitivity of 92% in predicting LT [6]. On cytology presence of lymphocytic impingement of thyroid follicular cells, presence of a mixed population of mature and transformed lymphocytes, Hurthle cells, follicular cells with fine chromatin, an iso-nucleosis, multinucleated giant cells, scanty or absence of colloid on aspirated smears are the hallmark of LT [6-11]. Hurthle cells appears as large cells forming small syncytial aggregates having well defined abundant finely granular eosinophilic cytoplasm and large nucleus [7,12].
Cytomorphological diagnosis may be superior in the initial stages of LT as antibody production may be confined to only intrathyroidal lymphocytes or localised areas without spillover into the blood [4,7,8]. Thus, there exists a wide range of values of TSH and variability of presence of ATPO making early diagnosis of LT difficult clinically and biochemically.
However, a combination of cytomorphological, clinical and biochemical features helps in making a better diagnosis than using individual features alone [12].
Not many studies have correlated LT grading on cytology with clinical, hormonal status and thyroid auto antibodies. With this background the aim of our study is to look into cytological features of LT and grade it according to Bhatia A et al., [10], and also to correlate the cytological grades of LT with clinical presentation, TSH, ATPO and Antithyroglobulin (ATG) levels.
Materials and Methods
The present study was a retrospective study done from June 2014 to June 2016 conducted at Sri Devaraj Urs Medical College and Research centre. One hundred and eighty five cases of LT which was diagnosed on cytology during this period were included in this study. Institutional ethical clearance was obtained before start of study. Demographic and clinical details along with stained slides (Papanicolaou’s, Hematoxylin and Eosin and May Grunwald, Giemsa stains) were obtained from the archives of our Pathology department. The diagnosis was confirmed and was graded according to criteria of Bhatia A et al., [10]. Any discrepancy was discussed and resolved by the senior pathologist. All cases of LT confirmed on cytology were included and patients with co-existing malignancies were excluded. Patients with ischemic heart diseases, cerebrovascular and neurological diseases, chronic renal impairment and pregnancy were also excluded from our study as these conditions may cause variation in thyroid hormone levels. Available data regarding age, sex, presenting complaints, duration of symptoms, clinical signs of hormonal variation, presence of nodular/diffuse enlargement were obtained from our archives and entered in the master sheet.
Cytological features of Lymphocytes: Epithelial cell ratio, follicular atypia, Hurthle cells, plasma cells and eosinophils were documented.
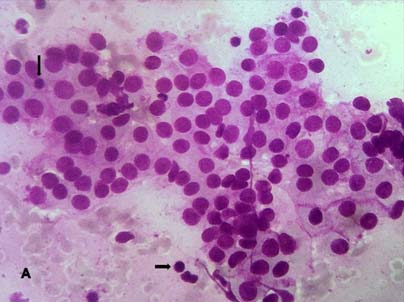
All cases were graded as per Bhatia A et al., grading system which is as follows [10]: Grade I (Mild): Few lymphoid cells infiltrating the follicles/increased number of lymphocytes in the background [Table/Fig-1].
Grade 1 Thyroiditis with mild lymphocytic infiltrate (arrows) (H&E; stain X 400).
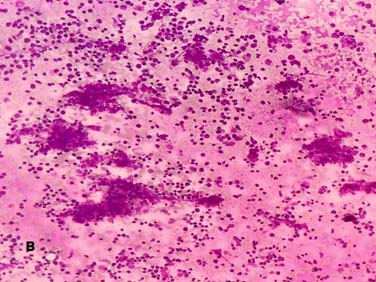
Grade II (Moderate): Moderate lymphocytic infiltration or mild lymphocytic infiltration with Hurthle cell change/giant cells/an isonucleosis [Table/Fig-2].
Grade 2 Thyroiditis with moderate lymphocytic infiltrates (H&E; X100).
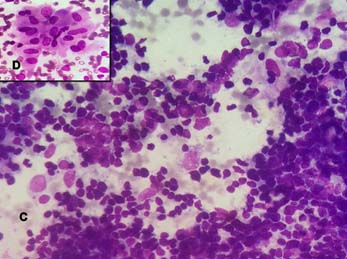
Grade III (Severe): Florid lymphocytic inflammation with germinal centre formation, very few follicular cells left [Table/Fig-3].
Grade 3 Thyroiditis total destruction of follicle with dense infiltration by lymphoid cells (MGG, X400) (Figure D: Inset shows Hurthle cell change – MGG; X1000).
Values of biochemical parameters like T3 (triiodothyronine), T4 (thyroxine), TSH and thyroid antibodies like ATPO and ATG were retrieved from biochemistry section of our hospital and documented whenever available. T3, T4 and TSH were documented in 98 cases and thyroid antibodies were documented in 59 cases. Rest of the cases did not have biochemical data.
Thyroid function tests namely T3, T4,TSH were done by electro chemilumiscence immunoassay. Test results were released only after running the quality control. The reference values considered in our study was: T3: 0.6-2.02 IU/mL, T4: 5.13-14.06 IU/mL, TSH: 0.27-5.5 IU/mL. Thyroid antibodies like ATPO and ATG levels were done using radioimmunoassay in an NABL referral lab. The reference range was as follows: ATPO: <35 IU/mL and ATG: < 25 IU/mL.
Statistical Analysis
Statistical analysis was done using SPSS version 22 (IBM, Corporation). Pearson’s Chi-square test and p≤0.05 was considered as significant. Biochemical values of thyroid function, cytological parameters and antithyroid antibody levels were correlated with one another using the Pearson’s correlation coefficient.
Results
One hundred and eighty five patients with cytology proven lymphocytic thyroiditis were included in our study. Females were 173 cases (93.5%) and 12 (6.5%) cases were male. Age of the cases ranged from 7-80 years, with majority between 25-45 years {123 cases (66.5%)}. There were 25 juvenile cases (age less than 18 years) accounting for 13.5%.
Majority of patients 134 cases (72.4%) manifested with diffuse enlargement and 51 (27.6%) cases presented with nodular presentation. Distribution of cases among various grades is represented in the [Table/Fig-4].
Grading of lymphocytic thyroiditis.
| Cytological grading | No. of Cases |
|---|
| Grade 1 | 45 |
| Grade 2 | 74 |
| Grade 3 | 66 |
| Total | 185 |
When clinical presentation was compared with grade, 97/134 (72.4%) of the patients with diffuse swelling were of grade 3 while nodular presentation was seen mostly in grade 1 32/51 (62.7%) patients.
Features of Lymphocytes: Epithelial cell ratio 120 cases (64.8%), follicular atypia 30 cases (16.2%), Hurthle cells 138 cases (74.5%), plasma cells 37 cases (20%) and eosinophils 20 cases (11%) were compared among various grades, but it did not show any statistical significance with grading (p-value >0.26).
Hormonal status was done in 98 cases. Thyroid profile values were within reference range in 49/98 (50%) cases, 43/98 (43.9%) cases showed raised TSH values and 6/98 (6.1%) cases had decreased TSH values. Out of 43 cases with increased TSH, 21 cases showed normal T3 and T4 (Subclinical hypothyroid) and 22 cases showed decreased T3 and T4 (frank hypothyroidism).
Comparison between TSH and grades are represented in the [Table/Fig-5]. A total of 30/45 cases (66.7%) of grade 1 showed normal TSH values. A total of 19/74 cases (25.7%) of grade 2 and 16/66 cases (24.2%) of grade 3 showed increased TSH values. There was a statistical significance between the cytological grades of LT and TSH (p-value <0.001).
Represents relation of cytological grading of lymphocytic thyroiditis with values of TSH and ATPO.
| Cytological grading | Thyroid stimulating Hormone (0.27-5.5 IU/mL) (n=98) | Antibodies (IU/mL) (n=59cases) |
|---|
| ATPO(<35 IU/mL) | ATG(<20 IU/mL) |
|---|
| Within Reference range (n=49) | Increase (n=43) | Decrease (n=6) | Increased (n=48) | Normal (n=11) | Increased (n=35) | Normal (n=24) |
|---|
| Grade 1(n=45 cases) | 30 | 8 | 3 | 20 | 12 | 13 | 4 |
| Grade 2(n=74 cases) | 13 | 19 | 2 | 15 | 15 | 14 | 15 |
| Grade 3 (n=66 cases) | 6 | 16 | 1 | 13 | 8 | 8 | 7 |
Pearson’s Chi-square test; (p-value <0.001 for TSH) (p-value 0.004 for ATPO) (p-value 0.026 for ATG)
Detection of antibody levels was done in 59 cases. ATPO was elevated in 81.3% (48/59) cases and ATG was raised in 59.3% (35/59) cases.
Out of 48 cases with increased ATPO levels grade I was seen in 20/48(41.6%), grade II in 15/48 (31.2%) and grade III were 13/48(27%). A total of 35 cases showed raised ATG levels with 13/35(40%) cases were of grade 1 while 14/35 (37.1%) cases were of grade 2 and 8/35 cases (22.8%) were of grade 3. There was a statistical significance between the cytological grades of LT and ATPO (p-value: 0.004). No statistical correlation was seen between grades of LT with ATG (p-value>0.005).
A total of 20 cases of grade 1 had increased ATPO. A 7/20 cases (35%) had increased TSH, 2/20 cases (10%) had decreased TSH. Fifteen cases of grade 2 had increased ATPO in which 4/15 cases (26.6%) were with normal TSH values, 10/15 cases (66.6%) had increased TSH and only one case with deceased TSH values. All the documented 13 cases had raised ATPO and were in grade 3 with increased TSH values.
When grade 3 was compared with combination of increased TSH levels and raised ATPO levels, both were increased in 13/30 cases. This was statistically significant. As mentioned in previous paragraph grade 3 was also statistically associated with increased TSH but not with ATPO values when compared alone, So combination of raised ATPO and increased TSH or alone increased TSH was significantly better in predicting grade 3 than only raised ATPO value. Relation of cytological grading of LT with values of TSH and ATPO are represented in [Table/Fig-5].
Discussion
The pathogenesis of LT is a complex multistep process, comprising of various genetic, environmental and immunological factors. Initially in active phase there is antibody mediated destruction of the thyroid follicles and intrathyroidal lymphocytic infiltration. Later in the chronic phase, there will be only minimal residual, atrophic follicles with fibrosis of the thyroid parenchyma, Depending on the stage, the patient present with different clinical features, hormonal status and thyroid autoantibodies levels. The cytological grades also depends on the stage of the disease process [10,12].
In the present study the age of occurrence of LT ranged from 7-80 years with female predominance. Majority of the patients were in the age group of 25-45 years, this age distribution was comparable to the observation made by Bhatia A et al., [10]. Contrast to our findings, the study from United Kingdom showed that patients were predominantly older women. This change in distribution of cases may be due to geographical variations in thyroid disorders [12].
In our study, the prevalence of juvenile LT (0-18 years) was 13.5%. The incidence of juvenile LT was comparable with studies done by other authors [13,14].
The contrasting theories have been put forwarded to describe the hypothesis of prevalence of LT. This disparity in age distribution among India and foreign studies is because of onset of thyroiditis in younger age group, due to high prevalence of iodine deficiency in India [12,15].
One more school of thought has proposed that high iodine intake may be an important risk factor for onset of thyroiditis. These patients with ATPO and ATG levels positive at baseline are more likely to be prone for thyroid dysfunction than seronegative patients [16].
Our findings of clinical presentation of 72.4% with diffuse enlargement and 27.6% of patients with nodular presentation was similar by Bhatia A et al., and Kumar N et al., [10,17]. Contrast to our findings Friedman M et al., have found nodular presentation in 80% of cases [18]. There is a controversial opinion that nodules represent early stages of the disease even before the clinical and biochemical changes have set in [10,12,17].
Lymphoid: Epithelial ratio is important feature for diagnosis of LT ranging from 2:1 to 10:1 on cytology smear in florid cases mimicking reactive lymphoid hyperplasia [8,18,19]. In our study, 120 cases (64.8%) showed high ratio.
Hurthle cell change was seen in 74.5% of patients which was comparable with other studies. [10,17,19]. Friedman M et al., showed that 98% cases having Hurthle cell change and characteristically seen in LT on cytological smears [18].
In our study follicular atypia was seen in 16.2% which is lesser than that seen in other studies [8,19].
Plasma cells were present in 37 cases (20%) of LT. Probable reason may be that T-cells are the predominant population of intrathyroidal lymphocytes in LT with B-cells confined to germinal centres, making plasma cells relatively infrequent on cytological smears. Studies conducted by Jayaram G et al., have also reported 23%, and Rathi M et al., 18% of LT [7,19].
Though none of these features were statistically significant, presence of these cytological features may help us in rising suspicion of LT on FNAC when few cells are yielded on aspiration of thyroid.
Grading of LT was done according to Bhatia A et al., criteria [10]. In our study majority of patients presented with grade 2 (40%) which was in tandem with Bhatia A et al., who reported 44% of grade 2 cases [10]. Sood N et al., (40%) and Kumar N et al., (38.1%) also have reported similar findings [2,17].
In our study euthyroid were predominant in grade 1 with 73.1%, which was in contrast to studies by Uma P et al., and Kudva R et al., where they showed balanced distribution of hypothyroid cases in all the grades [14,20]. This can be because of geographical variations in prevalence of hypothyroidism.
Raised ATPO levels was also described by Anila KR et al., wherein majority of cases (41.6%) were of grade 1, grade 2 (31.7%) and grade 3 in 27% [12]. We also found similar distribution [Table/Fig-5]. These findings supports that our patient presents at an early stage with raised ATPO levels, even before there is serological evidence of hormonal imbalance [12,21].
The relationship between grades, TSH levels and auto antibodies can be explained as follows. Alteration of autoantibodies causes destruction of thyrocytes which in turn leads to abnormalities in the hormonal levels. Early stages, autoantibodies will be elevated without much destruction of thyrocytes, hence normal hormonal levels [10,12]. Thus, on cytology these changes are reflected as grade 1 wherein only lymphocytes, without much Hurthle cells and follicular atypia are seen. No follicular cell infiltration by lymphocytes is seen.
Once the destruction is progressive, as in grade 3 with abundant lymphoctyes, germinal follicle form, numerous Hurthle cells and destruction of follicles are seen. This destruction also results in hormonal abnormalities which is in agreement with our observation of Sood N et al., Anila KR et al., Uma P et al., and Baker JR et al., [2,12,14,21].
Out of six cases of hyperthyroid three cases showed increased APTO. In that two cases were of grade 1 and one case was of grade 2. This phenomenon can be explained as follows; in early stage of the disease acute autoantibody mediated destruction of thyroid follicular cells results in exudation of hormones into the circulation resulting in hyperthyroidism [12,21]. Similar to the present study, Chandanwale SS et al., and Bagchi N et al., showed 23% and 8.1% respectively hyperthyroid cases where there was no clinical presentation but on cytology showed features of LT. They showed that most of the patients recover from hyperthyroidism [3,22].
Limitation
The number of cases of hyperthyroidism was very less to arrive at any logical conclusion and all cases of FNAC did not have biochemical parameters for correlation.
Conclusion
Cytological grading of LT reflects the hormonal and antithyroid antibodies levels. Diagnosis at early stage (grade 1) will help the treating clinicians to start early treatment and decrease the disease burden by preventing the patients going into hypothyroid state. Fine needle aspiration studies are affordable when compared with thyroid antibody testing. Hence, cytological grading can be considered as a basic investigation even when biochemical parameters are not available.
Pearson’s Chi-square test; (p-value <0.001 for TSH) (p-value 0.004 for ATPO) (p-value 0.026 for ATG)