Radiographic Retrograde Urethrography (RGU) remains the gold standard imaging study for evaluating anterior stricture disease, first popularised in 1910 by Cunningham [1]. Though RGU is a straightforward, readily available and cost-effective technique, its limitations include undermined stricture length, inability to clearly determine spongiofibrosis and need for multiple films for bilateral oblique views. Alteration of patient posture and penile traction while injecting contrast medium before imaging can alter the radiographic appearance of the stricture area and urethra. Stricture length in anterior urethra is often underestimated. It also entails need for repeated radiation exposure. To overcome these limitations, Sonourethrography (SUG) was proposed as a reliable, specific, reproducible, adjunctive imaging study, first popularised by McAninch [2]. The SUG better defines the extent of urethral stricture disease and spongiofibrosis, and hence, is favoured to evaluate the length and spongiofibrosis in anterior urethral stricture. For an appropriate treatment plan to be devised, it is important to determine the location, length, depth, and density of the stricture (spongiofibrosis). Though, the usefulness of SUG has been demonstrated in the evaluation of anterior urethral strictures [3-5], there is a lack of literature to correlate SUG over RGU or surgical method to determine stricture characteristics. The aim of this study was to prospectively analyse the role of SUG in the evaluation of anterior urethral stricture and its correlation with RGU and intraoperative findings.
Materials and Methods
This prospective study was conducted at a tertiary care institute in India from August 2012 to July 2014. Study participants were males aged more than 18 years with confirmed diagnosis of anterior urethral stricture. Patients with pelvic fracture, urethral distraction defect, multiple/complex strictures, pan-anterior strictures, prior urethral stricture surgery, and short segment strictures planned for Visual Internal Urethrotomy (VIU) were excluded. Patients with psychiatric illness were also excluded.
The study protocol was reviewed and approved by the institutional ethics committee. The study was conducted in accordance with the approved protocol and ethical principles that have their origin in Declaration of Helsinki. Each study participant provided written informed consent before participation.
Retrograde Urethrogram Procedure
Each patient received prophylactic antibiotic (ceftriaxone 1 gm, IV) before the procedure. The RGU was performed using standard technique, where patient was placed in supine position with pelvis oblique to 45 degrees with the dependent thigh acutely flexed to 90 degrees [Table/Fig-1]. The penis was placed on moderate stretch. Either a 10 mL syringe tip, or infant, or 8F Foley’s catheter inserted with bulb inflated to 1 mL in fossa navicularis was used to instill contrast material. The study was performed using 10 to 20 mL of urografin 76% (1:1 dilution with sterile water) by slowly injecting into urethra and static RGU films were taken. The stricture length was measured using electronic calipers. Simultaneously, Micturating Cysto-Urethrogram (MCU) was performed in all patients to assess posterior urethra. For MCU, the bladder was distended with dilute contrast, either via a catheter already placed in supra-pubic region, or by retrograde catheterization of infant feeding tube under full aseptic precaution after injecting 2% lignocaine jelly before catheterization. Right and left oblique views radiographs were obtained while patient was voiding on table.
Patient position during radiographic retrograde urethrography, and measurement of urethral stricture length.

Sono-Urethrography Procedure
The patient was placed in supine frog leg position for SUG procedure. Foley’s catheter (8 F) was placed in the urethra with bulb inflated to 1 mL in the fossa navicularis. A linear array transducer (7.5 MHz) was placed directly on the ventrum of penis, scrotum and perineum after applying the gel. Saline was slowly and repeatedly instilled by catheter tip syringe and simultaneous real time images of the anterior urethra were obtained sequentially from the pendulous urethra proximally toward the deep bulbar area. The stricture site and length were assessed using electronic calipers [Table/Fig-2]. Periurethral Fibrosis (PUF) was identified on sonography as regions of greater echogenicity (brighter) than normal parts of the corpus spongiosum. These were classified as mild (up to 33%), moderate (33-50%) and severe (more than 50%) depending on the thickness of the corpus spongiosum [2].
Transducer placement and urethral stricture measurement during sonourethrography procedure.

Intraoperative Measurement
The stricture length was assessed using measuring scale, after surgically opening the stricture site [Table/Fig-3]. The PUF was further assessed by palpating the stricture segment.
Intraoperative measurement of urethral stricture.

Statistical Analysis
Statistical analysis was performed using SPSS version 20.0 (IBM Corp., Armonk, NY, USA). Nonparametric spearman correlation was performed between RGU, SUG and intraoperative findings and p-value of <0.05 was considered statistically significant.
Results
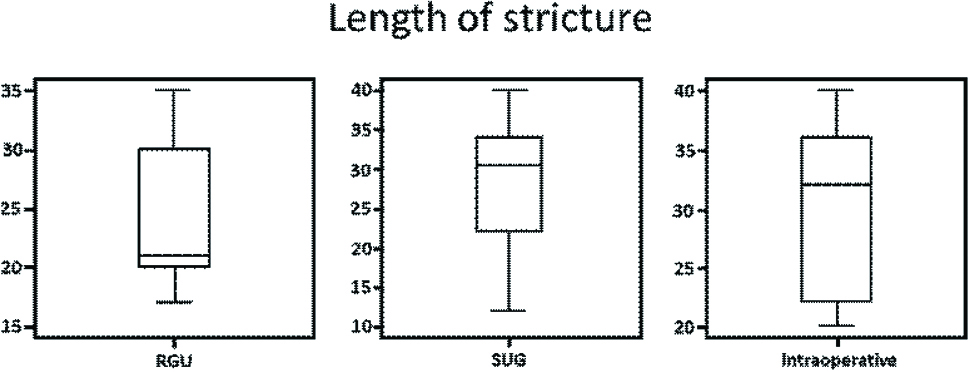
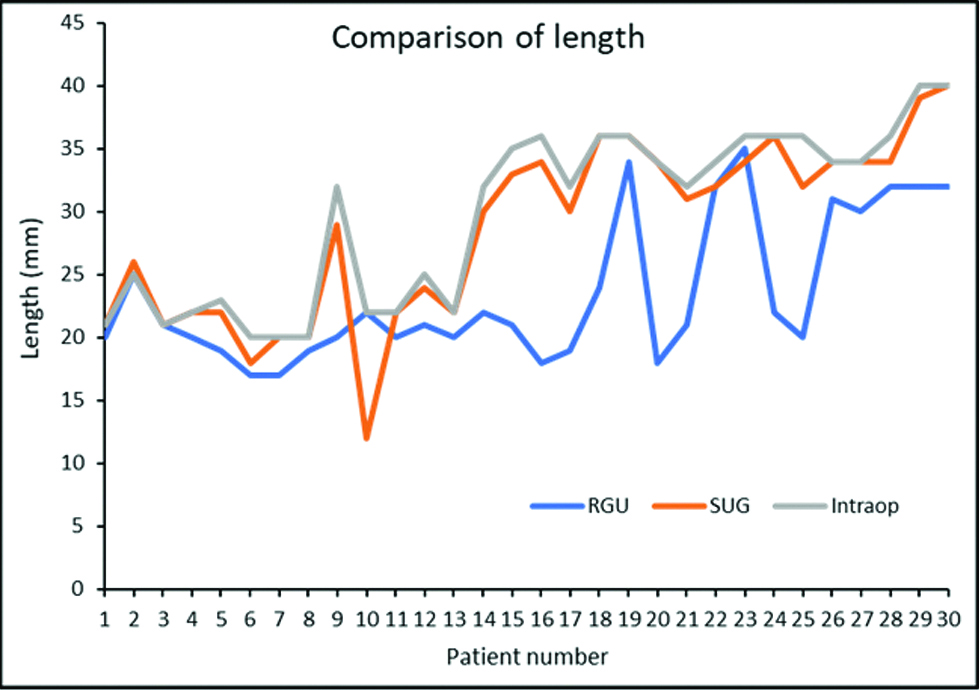
During the study period, a total of 369 patients diagnosed with anterior urethral stricture and were screened for study. Of these, a total of 30 patients underwent RGU and SUG preoperatively and intraoperative stricture length and spongiofibrosis were assessed and participated in this study. The mean (SD) age was 39 (16) years (range 18-62). The aetiology of stricture was inflammatory (n=10), trauma (n=7), catheter induced (n=7) and idiopathic (n=6) [Table/Fig-4]. The median (IQR) length for RGU, SUG and intraoperative group was 21 (11) mm, 30.5 (13) mm and 32 (14) mm, respectively [Table/Fig-5]. After SUG, four, 12 and 14 patients had mild, moderate and severe spongiofibrosis, respectively. Spearman correlation calculated between RGU, SUG and intraoperative stricture lengths showed significant correlation between SUG and intraoperative lengths [Table/Fig-6]. Overall, the RGU underestimated stricture length; however, the SUG was closer to intraoperative stricture length in all patients. The median RGU length correlation was up to 59% with intraoperative findings and median SUG length correlation was up to 94% compared with intraoperative findings (p<0.001) [Table/Fig-7].
Demographics and clinical characteristics.
| Parameter | TotalN=30 |
|---|
| Age (years), median (SD) | 39.0 (16.0) |
| Age (Years), n (%) |
| 18-20 | 3 (10.0) |
| 21-30 | 5 (16.7) |
| 31-40 | 9 (30.0) |
| 41-50 | 10 (33.3) |
| 51-62 | 3 (10.0) |
| Stricture etiology |
| Trauma | 7 (23.3) |
| Catheter induced | 7 (23.3) |
| Idiopathic | 6 (20.0) |
| Inflammatory | 10 (33.3) |
| Site of stricture |
| Bulbar | 19 (63.3) |
| Distal bulbar | 11 (36.7) |
| Intervention |
| No suprapubic cystotomy | 8 (26.7) |
| Suprapubic cystotomy | 22 (73.3) |
SD: Standard deviation
Length of stricture.
RGU: Retrograde urethrography; SUG; Sonourethrography; Intraop: Intraoperative stricture length
Correlation between RGU, SUG and intraoperative stricture lengths.
| Modality | Spearman correlation coefficient (significance) |
|---|
| RGU | SUG | Intraop |
|---|
| RGU | 1.00 | 0.673 (<0.001) | 0.597 (0.001) |
| SUG | 0.673 (<0.001) | 1.00 | 0.946 (<0.001) |
| Intraoperative | 0.597 (0.001) | 0.946 (<0.001) | 1.00 |
RGU: Retrograde urethrography; SUG: Sonourethrography; Intraop: Intraoperative stricture length
Comparison of structure length. p-value <0.001 (Friedman test).
RGU: Retrograde urethrography; SUG: Sonourethrography; Intraop: Intraoperative stricture length
Discussion
Urethral strictures are common generally affecting young adult males causing morbidity and discomfort. Urethral stricture refers to anterior urethral narrowing, which involves corpus spongiosum, caused due to injury, infection or instrumentation. Patients may present with obstructive voiding symptoms, urinary tract infections such as prostatitis and epididymitis, or urinary retention.
Retrograde urethrography was the standard imaging technique for the evaluation of anterior male urethra until the introduction of SUG by McAninch [2]. Since then, both RGU and SUG have been used; however, RGU provides limited information about periurethral structures. The SUG is able to assess both, the urethral and periurethral structures. Measurement of the stricture length in the bulbar urethra is more accurate than conventional RGU [6], while spongiofibrosis is manifested by lack of urethral distensibility during retrograde installation of saline solution. Morey et al reported that the length of the stricture measured through SUG was double or more than the value reported through urethrography demonstrating its usability on selection [7]. In contrast, several other studies have demonstrated that SUG is equally efficacious in detecting anterior urethral strictures and can be used as an alternative to RGU in determining the stricture length of anterior urethra [8-10]. A greater sensitivity can be achieved when both of these methods are used in combination [11].
Gupta et al conducted a study comparing SUG versus RGU in patients with anterior urethral stricture (n=30) and result showed that SUG was an accurate predictor of stricture length, while RGU underestimated the length in most of the cases [12]. It was further reported that SUG was unsatisfactory in evaluation of membranous stricture [12].
In another previous study by Pushkarna R et al. that included 20 patients with urethral strictures, SUG was positive in all cases in which RGU showed strictures and was also positive in one case where RGU was negative. In none of the cases, only picked up a lesion where SUG did not [13]. Similarly, Nash PA et al., found a significant difference between stricture length (p<0.003), measured by RGU as compared to SUG. Same study also suggested that SUG was unreliable in predicting the depth of spongiofibrosis when compared with full depth biopsies with histopathological correlation [14].
Heidenreich A et al., reported 98% sensitivity and 96% specificity while using SUG in the detection urethral stricture [15]. Samaiyer SS et al., described the diagnostic accuracy by RGU was lower (85.7%) compared to SUG in 96.4% in their study [16]. Findings of the present study suggest lower median RGU length correlation (up to 59%) with intraoperative findings, as compared to greater median SUG length correlation (up to 94%) when compared with intraoperative findings (p<0.001). Additionally, spongiofibrosis was detected in all 30 cases (100%). SUG had similar sensitivity in identifying false tracts (5 out of 30 patients) as compared with RGU. Moreover, SUG was 100% sensitive and specific in identifying spongiofibrosis.
Conclusion
Results showed that both SUG and intraoperative have almost equal efficacy in detecting anterior urethral stricture. Though, further stricture characterization (stricture length and periurethral soft tissue abnormalities) can be done by SUG with greater confidence and accuracy. Additionally, non-exposure to radiation is an added benefit with SUG. Results of the present study also showed similar observations with SUG to that of operative findings, as compared to RGU. Overall, SUG is a simple technique that provides a dynamic, precise assessment of anterior urethral strictures.
SD: Standard deviation
RGU: Retrograde urethrography; SUG: Sonourethrography; Intraop: Intraoperative stricture length