Double Barrel Oesophagus- A Case Report
Gulam Mohiuddin Marfani1, Shivali Vaibhav Kashikar2, Shraddha Singhania3
1 Resident Doctor, Department of Radiodiagnosis, Acharya Vinobha Bhave Rural Hospital, Wardha, Maharashtra, India.
2 Professor, Department of Radiodiagnosis, Acharya Vinobha Bhave Rural Hospital, Wardha, Maharashtra, India.
3 Senior Resident, Department of Radiodiagnosis, Acharya Vinobha Bhave Rural Hospital, Wardha, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Gulam Mohiuddin Marfani, T-10, Raghobaji Hostel, 3rd floor, inside Acharya Vinobha Bhave Rural Hospital, Sawangi (Meghe), Wardha 442001, Maharashtra, India.
E-mail: gulam.marfani@gmail.com
Double barrel Oesophagus is a rare entity that involves a mucosal injury, thereby creating of a true and false lumen within the oesophagus. Diagnostically it is important to differentiate complete and partial dissection of oesophagus because the management of partial dissection is conservative and full dissection is a surgical emergency needing operative intervention.
Health problems, Occupational health, Unorganised sector
Case Report
We report a case on Intramural Oesophageal Dissection (IED) in a male patient aged 30 years suffering with pancreatitis and cirrhosis since a year. Patient was a chronic alcoholic and had undergone endoscopic examination for oesophageal varices two days before and was brought to our department of radiodiagnosis with haematemesis, dysphagia and severe retrosternal chest pain after the examination. Symptoms further exaggerated over the course of time. There was vomiting, and a sensation of something sticking in the lower gullet caused him to swallow repeatedly in trying to dislodge it. Auscultation of the heart and chest was non-contributory and there was no tenderness on abdominal palpation. The pain was uninfluenced by two intravenous injections of 5 ml of Buscopancompositum (hyoscinebutylbromide) and was lessened only after an intramuscular injection of 100 mg of pethidine.
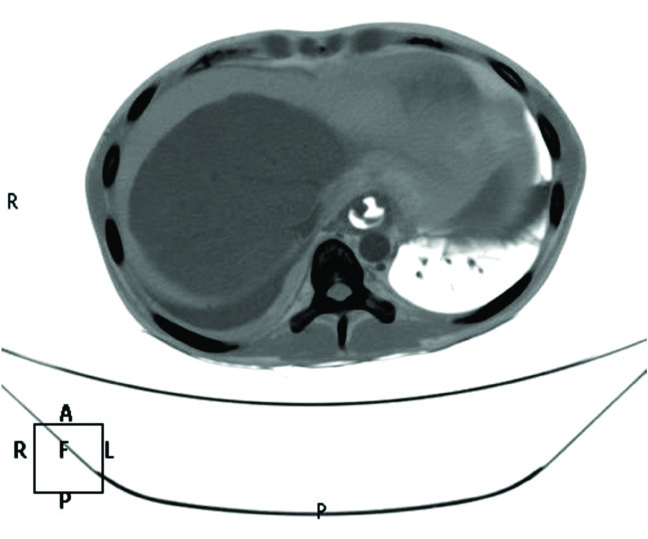
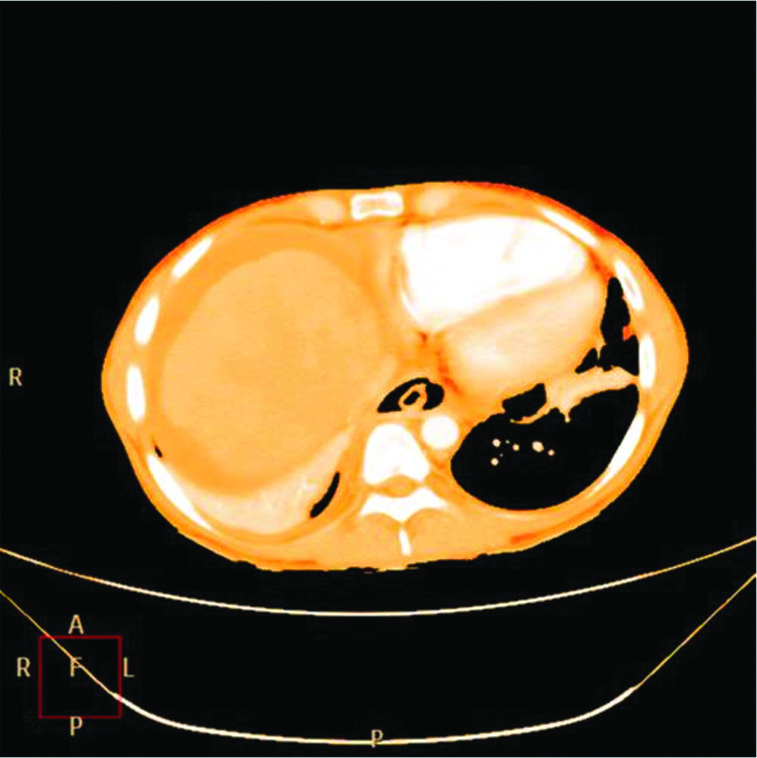
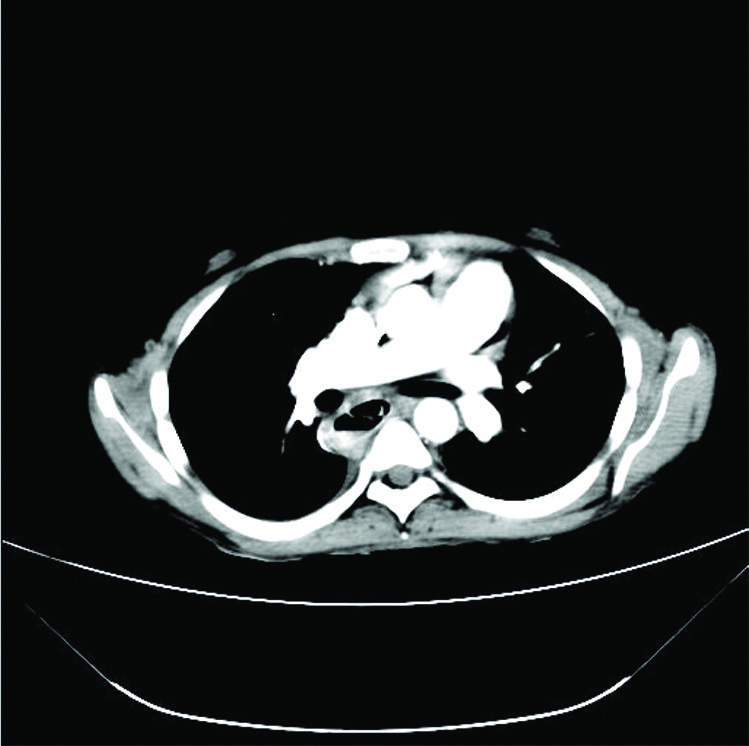
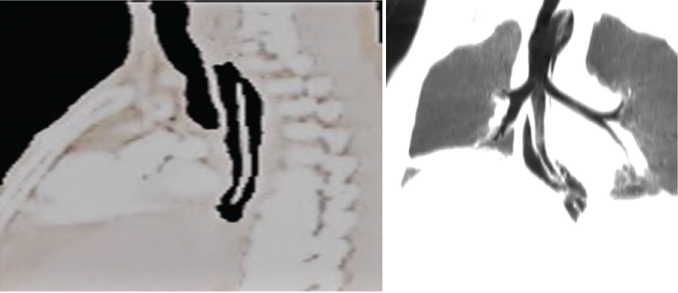
A contrast enhanced CT Thorax and Abdomen was done using ultravist (oral and intra-venous). The oesophagus appeared as a lumen within a lumen giving a double barrel appearance [Table/Fig-1,2]. The false lumen was seen posterior to the true lumen. During swallowing accumulation of contrast was noted in the false lumen seen posterior to the true lumen of the oesophagus [Table/Fig-3], on the right postero-lateral side. This accumulation was 8mm in depth and16mm wide and did not track away, which could be demonstrated repeatedly. Full extent of dissection is best appreciated on sagittal or coronal reformatted images [Table/Fig-4]. The diagnosis of an intramural rupture was made.
Volume rendered Axial contrast enhanced CT image reveals the differentiation between the true and the false lumen the one in continuation with the gastro-oesophageal junction is the true lumen and the lumen posterior to the true lumen is the false lumen;
Volume rendered Axial contrast enhanced CT image reveals there are two lumen noted within the oesophagus giving a double barrel oesophagus (a true and a false lumen) which is pathognomonic of ‘intra-mural oesophageal dissection’;
Axial contrast enhanced CT image reveals Lumen within the lumen appearance of the oesophagus with contrast material extravasating into the false lumen in the right postero-lateral aspect giving fluid level.
a,b) Volume rendered sagittal and coronal contrast enhanced CT image showing mucosal separation of the oesophagus involving the middle and lower oesophagus.
There were a few collaterals noted along the lower oesophagus in concordance with the oesophageal varices due to portal hypertension. Furthermore, the liver appeared shrunkened and along irregular surface with deranged liver function test and the pancreas appeared bulky with calcification noted throughout the pancreatic parenchyma and deranged amylase and lipase which was in correlation with chronic pancreatitis.
Discussion
Intramural Oesophageal Dissection is a rare but well-described condition that is characterised by separation of the oesophageal mucosa and sub-mucosa but without perforation [1]. Rupture of the oesophagus is a rare but well-documented emergency and has been referred to by a number of terms, including intramucosal-oesophageal dissection, intramural oesophageal rupture, oesophageal apoplexy, and sub-mucosal haematoma [2] which may result from violent vomiting or less commonly from other causes of an abrupt increase in intra-abdominal or intra-thoracic pressure such as epilepsy, childbirth, defecation, weight-lifting, or non-penetrating blows on the chest [3]. Spontaneous intramural haematoma of the oesophagus has also been reported most often in patients who are undergoing anticoagulant drug therapy or who have inherent coagulopathy [4,5]. In our case, due to the presence of oesophageal varices due to portal hypertension and a history of recent instrumentation for endoscopy may have precipitated for the dissection of oesophagus. Symptoms include an abrupt onset of retrosternal chest pain, dysphagia or odynophagia, and haematemesis with most patients experiencing at least two of the three symptoms and with haematemesis generally occurring later in the clinical course [4]. The rupture usually occurs as a longitudnal slit in the left postero-lateral wall of the lower oesophagus within 5-6 cm of the cardia, and it is generally agreed that this may occur in the absence of underlying disease of the oesophagus [2].
CT findings of dissection are in correlation with those seen at oesophagography: a mucosal flap with sub-mucosal distribution of gas or contrast material giving the oesophagus the classic double-barrelled appearance which is seen as a true lumen and a false lumen (posterior). Since the treatment of incomplete rupture of the oesophagus would appear to be conservative, it is important to exercise considerable care in excluding a complete rupture of the oesophagus, a grave condition in which surgery usually offers the only hope of survival [2]. Patients with a presumptive diagnosis of incomplete rupture must be repeatedly examined to exclude surgical emphysema. The absence of mediastinal or surgical emphysema and lack of chest signs pointed very strongly against a complete oesophageal rupture. The condition settled on conservative measures.
Incomplete rupture of the oesophagus should not be confused with the Mallory-Weiss syndrome, a condition characterised by brisk haematemesis due to vomiting-induced mucosal tears of the cardia of the stomach (Mallory and Weiss, 1929). The long axis of these mucosal tears are in line with the oesophagus, and, rarely, they may extend from the cardia into the lower end of the oesophagus [2]. Symptomatically, Mallory-Weiss syndrome implicates painless haematemesis while intramural oesophageal rupture has severe pain with haematemesis.
The treatment of intramural oesophageal dissection is conservative; nothing by mouth, intravenous fluid supply, and total parenteral nutritional support are the mainstays of therapy. On follow-up endoscopy, most of the intramural oesophageal dissections have satisfactory healing within two to three weeks after onset of symptoms [1,6]. Endoscopic therapies including incision of the septum between the true and false lumens [7], balloon dilatation [8], transection of the true oesophageal wall [9], and metal stent insertion [10], have been used to treat intramural oesophageal dissection with refractory to conservative treatment. Surgery should be reserved for cases that do not respond or resolve with conservative management, or that have complications, such as oesophageal perforation [11] or on-going haemorrhage [12].
Conclusion
In this case, CT thorax enabled the diagnosis and pre-operative evaluation of this rare and unexpected aetiology of chest pain and dysphagia. The patients developing chest pain and dysphagia after an endoscopic procedure, intra mural dissection of oesophagus should always be considered. The physician or the surgeon usually treat it conservatively, however if there is clinical deterioration of patient, high suspicion of an ongoing haemorrhage or perforation should always be considered.
[1]. Cho CM, Ha SS, Tak WY, Kweon YO, Kim SK, Choi YH, Endoscopic incision of a septum in a case of spontaneous intramural dissection of the esophagusJournal of clinical gastroenterology 2002 35(5):387-90.10.1097/00004836-200211000-0000612394226 [Google Scholar] [CrossRef] [PubMed]
[2]. Young CA, Menias CO, Bhalla S, Prasad SR, CT features of esophageal emergenciesRadiographics 2008 28:1541-53.10.1148/rg.28608552018936020 [Google Scholar] [CrossRef] [PubMed]
[3]. Cullen SN, McIntyre AS, Dissecting intramural haematoma of the oesophagusEur J Gastroenterol Hepatol 2000 12(10):1151-62.10.1097/00042737-200012100-0001411057463 [Google Scholar] [CrossRef] [PubMed]
[4]. Fadoo F, Ruiz DE, Dawn SK, Webb WR, Gotway MB, Helical CT esophagography for the evaluation of suspected esophageal perforation or ruptureAJR Am J Roentgenol 2004 182:1177-79.10.2214/ajr.182.5.182117715100114 [Google Scholar] [CrossRef] [PubMed]
[5]. Younes Z, Johnson DA, The spectrum of spontaneous and iatrogenic esophageal injury: perforations, Mallory-Weiss tears, and hematomasJ Clin Gastroenterol 1999 29(4):306-17.10.1097/00004836-199912000-0000310599632 [Google Scholar] [CrossRef] [PubMed]
[6]. Hsu CC, Changchien CS, Endoscopic and radiological features of intramural esophageal dissectionEndoscopy 2001 33:379-81.10.1055/s-2001-1369611315903 [Google Scholar] [CrossRef] [PubMed]
[7]. El-Chami MF, Martin RP, Lerakis S, Esophageal dissection complicating transesophageal echocardiogram — the lesson to be learned: do not force the issueJ Am Soc Echocardiogr 2006 19:597e5-e7.10.1016/j.echo.2005.12.01616644447 [Google Scholar] [CrossRef] [PubMed]
[8]. Gluck M, Jiranek GC, Low DE, Kozarek RA, Spontaneous intramural rupture of the esophagus: clinical presentation and endoscopic findingsGastrointest Endosc 2002 56:134-36.10.1067/mge.2002.12536012085053 [Google Scholar] [CrossRef] [PubMed]
[9]. Kim SH, Lee SO, Circumferential intramural esophageal dissection successfully treated by endoscopic procedure and metal stent insertionJ Gastroenterol 2005 40:1065-69.10.1007/s00535-005-1692-y16322952 [Google Scholar] [CrossRef] [PubMed]
[10]. Soulellis CA, Hilzenrat N, Levental M, Intramucosal esophageal dissection leading to esophageal perforation: case report and review of the literatureGastroenterology & hepatology 2008 4(5):362 [Google Scholar]
[11]. Khil EK, Lee H, Her K, Spontaneous intramural full-length dissection of esophagus treated with surgical intervention: multidetector CT diagnosis with multiplanar reformations and virtual endoscopic displayKorean Journal of Radiology 2014 15(1):173-77.10.3348/kjr.2014.15.1.17324497810 [Google Scholar] [CrossRef] [PubMed]
[12]. Yeom S, Lee C, Cha S, “Double barrelled esophagus” sign in the intramural dissection of esophagusAbdominal Radiology 2016 42(3):983-84.10.1007/s00261-016-0949-727744550 [Google Scholar] [CrossRef] [PubMed]