Gestational Gigantomastia: Challenges in Management and Follow Up
Vidyashree Ganesh Poojari1, Rekha Upadhya2, Muralidhar V. Pai3, L. Ramachandra4, Vidya Monappa5
1 Assistant Professor, Department of Obsterics and Gynaecology, Kasturba Medical College, MAHE, Manipal, Karnataka, India.
2 Assistant Professor, Department of Obsterics and Gynaecology, Kasturba Medical College, MAHE, Manipal, Karnataka, India.
3 Professor and Head, Department of Obsterics and Gynaecology, Kasturba Medical College, MAHE, Manipal, Karnataka, India.
4 Professor, Department of Surgery, Kasturba Medical College, MAHE, Manipal, Karnataka, India.
5 Associate Professor, Department of Pathology, Kasturba Medical College, MAHE, Manipal, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Vidyashree Ganesh Poojari, Assistant Professor, Department of Obsterics and Gynaecology, Women and Child Block, Kasturba Medical College, MAHE, Manipal-576104, Karnataka, India.
E-mail: drvidyaganesh@gmail.com
Gestational Gigantomastia (GG) is a rare condition that presents with excessive enlargement of breast which becomes uncomfortable and embarrassing. Here is a case report of a primigravida who presented to us with GG at term. Post-delivery she had abscess formation and difficulties in breastfeeding. She was conservatively treated by abscess drainage and lactation suppression.
Cabergoline, Breastfeeding, Mastectomy
Case Report
A 28-year-old primigravida was referred to us at 38 weeks of gestation with bilateral enlargement of the breast. Patient reported that breast enlargement was noticed since third month of pregnancy and since past one month the breast had grown almost five times the prepregnancy size measuring approximately 20 cm in circumference. She had severe pain and discomfort due to abnormal enlargement of breast for which she was given analgesics intermittent. She was finding difficult to do her routine activities due to the abnormal enlargement of breasts. Past medical surgical history was unremarkable.
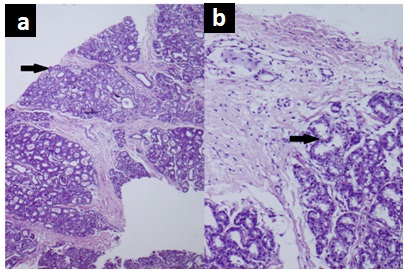
On examination, patient was afebrile. There was abnormally enlarged breast bilaterally with dilated superficial veins [Table/Fig-1]. Uterus was term size, cephalic presentation. For the histopathological diagnosis, trucut biopsy of breast was done which was suggestive of gestational hyperplasia of the breast [Table/Fig-2]. Serum prolactin was 80ng/mL (40-270 ng/mL), serum calcium was 10 mg/dl (8.6-10mg/dL). In view of foetal distress she underwent caesarean section, had a live female baby of 3.2 kg with good Apgar score.
Patient with gestational gigantomastia at 38 weeks-initial presentation

a) Section shows hyperplastic breast lobules with interspersed thick fibrous septae, (H&E 40x); b) Acinar cells show lactational change with vacuolated cytoplasm surrounded by thick oedematous fibrous septae (H&E, 200x).
Patient opted to breast feed her baby which was consented by the paediatrician also. Though she had difficulty in breast feeding due to enlarged breasts, good nursing care was given and she continued with breast feeding. She was discharged on seventh postoperative day with an advice to come for postnatal checkup after six weeks. During her six week postnatal visit, she complained of, intermittent fever and severe pain in the left breast. On examination, there was redness and rise of temperature of left breast but right breast had relatively reduced in size. Ultrasound of the breast showed abscess in the left breast measuring 5 x 6 cm which was drained. She continued to have excessive pain, engorgement and could not continue with breastfeeding. Hence, lactation was suppressed with the help of Cabergoline 0.5mg (2 doses 24 hours apart) after which she drastically improved. [Table/Fig-3] shows grossly reduced size of the breast after three months of delivery.
Regression of the size of the breast, three months after delivery.

Discussion
Gestational gigantomastia is a rare condition that presents as breast enlargement during pregnancy. It is also known as gravid macromastia. It causes massive enlargement of the breasts with thinning of the skin, tissue necrosis, infection and hemorrhage. Restricted movements, respiratory difficulty, emotional, social and psychological problems may also occur [1-3].
Aetiology and pathogenesis of GG have yet to be fully understood. However, studies have suggested several theories including endocrine imbalance, hyperprolactinemia and end organ hypersensitivity [2-4]. A prior history of gestational gigantomastia increases the risk in subsequent pregnancies. Occurrence is more commonly seen in Caucasian and multiparous women [3].
Phylloides tumour, fibroadenoma, non-Hodgkin’s lymphoma and lymphoblastic lymphoma are possible differential diagnosis, which can be excluded by biopsy [4]. Hence, a thorough workup including white blood cell count, haematocrit level, platelet count, hormone profile (oestrogen, progesterone, and prolactin), and tissue biopsy needed to come to a diagnosis. Furthermore, there have been reported cases of hypercalcaemia with gigantomastia, possibly attributed to excessive production of Parathyroid Hormone related Protein (PTHrP) by hypertrophied breast tissue [3-5]. Hence, patients presenting with gigantomastia should also be worked up for hypercalcaemia, as high levels may require bilateral mastectomy. Rule out concurrent liver disease as deranged liver function tests have also been reported with this condition.
The choice of treatment for these patients is different based on the severity of each case. Proper brassiere support, good skin hygiene, adequate nutrition, and analgesia are helpful in these cases. In most of the cases conservative management have resulted in spontaneous resolution of tissue hypertrophy in the postpartum period. However, medical and surgical interventions are essential in cases that fail to regress or in those who present with the aforementioned complications [2,4].
To date, bromocriptine is the most widely used medical regimen for the treatment of GG, but results have been variable. Studies have shown that bromocriptine therapy during pregnancy may lead to intrauterine foetal growth restriction; therefore it is suggested that foetal growth should be monitored if bromocriptine is used during the course of pregnancy [5,6]. Studies have shown that use of bromocriptine during pregnancy is helpful in preventing and healing necrotic breast ulcerations, cessation of further enlargement of breast, promoting regression, and decreasing the need for surgical management. Bromocriptine may also be continued during the postpartum period to suppress lactation and breast growth [7]. Unlike the case described by Turkan H et al., our patient was stable till term pregnancy without any complications, requiring postnatal lactation suppression. In that case, the woman had massive breast enlargement at midtrimester itself requiring bilateral mastectomy [8].
Surgical intervention is the most successful treatment for gestational gigantomastia. It may be indicated in cases of massive hemorrhage, ulceration, sepsis, and breast necrosis. Surgery during the immediate postpartum period may be indicated to prevent further complications such as puerperal mastitis, in cases of enormous hypertrophy in which reduction is unlikely with bromocriptine therapy alone or in those cases where there is continued growth despite of medical therapy. But in the present case, symptoms regressed with medical management alone and did not require mastectomy. Since there is a possibility of recurrence with simple mastectomy or reduction mammoplasty, bilateral mastectomy with reconstruction is the treatment of choice in women who desire future pregnancies [6,7].
Conclusion
A complete knowledge regarding this rare but distressing condition is a must among all practicing obstetricians. Multidisciplinary team effort is required for a successful fetomaternal outcome. In order to rule out other underlying disease processes which can present as gigantomastia, a full workup including haematology, endocrinology, and biopsy should be completed. Treatment option should be tailored based on the severity of the disease. A trial of postpartum Cabergoline with cessation of breastfeeding is recommended to possibly reduce breast size before surgical intervention.
Financial or Other Competing Interests
Permission was taken for publication of this case and images from patient.
[1]. Pollyana ER, Natalia QB, Fernanda AB, Fabio C, Danielle C, Antonio CF, Management and follow-up of a case of gestational gigantomastia in a Brazilian hospitalCase Reports in Obstetrics and Gynecology 2014 2014:61036310.1155/2014/61036325215252 [Google Scholar] [CrossRef] [PubMed]
[2]. Van Wingerden JJ, Gigantomastia—definition and association with hypercalcaemiaJ Plastic, Reconstructive & Aesthetic Surgery 2009 62(1):112-15.10.1016/j.bjps.2008.06.01918805078 [Google Scholar] [CrossRef] [PubMed]
[3]. Ibrahim A, Enesi PO, Abur PP, Oguntayo AO, Garba ES, Bilateral gestational gigantomastia complicated by severe sepsis; case report of a preventable mortalityNigerian J Surgical Research 2013 15(1):29-32.10.4103/1595-1103.141392 [Google Scholar] [CrossRef]
[4]. Shoma A, Elbassiony L, Amin M, Zalata K, Megahed N, Elkhiary M, Gestational gigantomastia’: a review article and case presentation of a new surgical management optionSurgical Innovation 2011 18(1):94-101.10.1177/155335061039110621189267 [Google Scholar] [CrossRef] [PubMed]
[5]. Vidaeff AC, Ross PJ, Livingston CK, Parks DH, Gigantomastia complicating mirror syndrome in pregnancyObstetrics & Gynecology 2003 101(5):1139-42.10.1016/S0029-7844(03)00061-9 [Google Scholar] [CrossRef]
[6]. Bloom SA, Nahabedian MY, Gestational macromastia: a medical and surgical challengeBreast J: The Breast Journal 2008 14(5):492-95.10.1111/j.1524-4741.2008.00628.x18657144 [Google Scholar] [CrossRef] [PubMed]
[7]. Rezai S, Nakagawa JT, Tedesco J, Chadee A, Gottimukkala Mercado R, Gestational gigantomastia complicating pregnancy: a case report and review of the literatureCase Reports in Obstetrics and Gynecology 2015 2015:89236910.1155/2015/89236926713166 [Google Scholar] [CrossRef] [PubMed]
[8]. Turkan H, Gokgoz MS, Taşdelen I, Dundar HZ, Gestational gigantomastiaBreast Health 2016 12:86-87.10.5152/tjbh.2016.285228331740 [Google Scholar] [CrossRef] [PubMed]