Varied Orbital Inflammations in Diabetics
Sumana J Kamath1, Bindu Kolavala2, Vasuraj Saini3
1 Professor, Department of Ophthalmology, KMC Mangalore, Mangaluru, Karnataka, India.
2 Junior Resident, Department of Ophthalmology, KMC Mangalore, Mangaluru, Karnataka, India.
3 Junior Resident, Department of Ophthalmology, KMC Mangalore, Mangaluru, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Bindu Kolavala, D/O K Raja Reddy, Madhura Nagar, Tirupati, Andhra Pradesh, India.
E-mail: bindukolavala@gmail.com
Orbital cellulitis is purulent inflammation of the cellular tissue of the orbit. It is one of the clinical emergencies which need early diagnosis and treatment, especially in diabetics and immunocompromised patients. We report two rare presentations of orbital inflammations in diabetics, who recovered with early diagnosis and prompt treatment subsequently.
Diabetics, Fatal, Orbital cellulitis
Case Report
Case 1
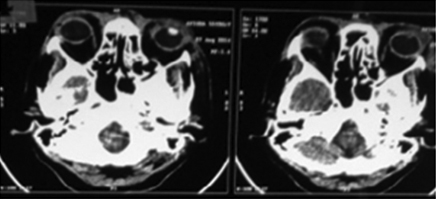
A 55-year-old diabetic female presented with swelling and redness of both eyes since two weeks [Table/Fig-1], associated with fever. Her best corrected visual acuity was 6/6 in the right eye and 6/9 in the left eye. Restriction of ocular movements was noted in all directions in both eyes. Left upper eyelid abscess was noted [Table/Fig-2]. On examination, pupillary reactions and colour vision were normal; there was no evidence of proptosis. Visual fields assessment could not be done as the patient was in severe pain. Computed Tomography (CT) scan findings were suggestive of preseptal cellulitis with suspected abscess on the superolateral aspect of left orbit [Table/Fig-3]. Incision and drainage of left upper eyelid abscess was done. Pus culture showed growth of a gram negative bacterium, Burkholderia pseudomallei, which is sensitive to Ceftazidime. A diagnosis of Melioidosis was made. As per physician’s advice, patient was started on intravenous Ceftazidime TID for 12 days, Tab. Clindamycin 300 mg TID for 10 days. Her fasting blood sugar level was 138 mg/dL and postprandial blood sugar level was 382 mg/dL. Control of blood sugar levels was achieved. On follow up after two weeks, patient’s condition improved subsequently.
Swelling and redness of both eyes at day one presentation;

Left upper eyelid at day three.

CT scan showing preseptal soft tissue thickening with subtle hypodense area on the superolateral aspect of left orbit.
Case 2
A 53-year-old diabetic male presented with swelling, redness and pain of left eye since four days, with progression to periorbital dermal necrosis and black eschar formation after day one [Table/Fig-4]. He gave history of insect bite four days ago. Best corrected visual acuity was 6/6 in Right eye, 6/60 in left eye. There was no restriction of extraocular movements. Pupillary reactions and colour vision were normal, and there was no proptosis on examination. Black eschar formation is the hallmark of mucormycosis. So, mucormycosis, a rapid fulminating condition was suspected clinically. But, pus culture reported growth of Staphylococcus aureus. A clinical diagnosis of left eye preseptal cellulitis was made. Patient was started on intravenous Magnex 2 gm BD for seven days and Clindamycin 600 mg TID for seven days. His fasting blood sugar level was 125 mg/dL and post prandial blood sugar level was 317 mg/dL. On follow up after two weeks, patient’s condition improved with subsidence of swelling and eschar, on control of blood sugar levels.
Periorbital dermal necrosis with black eschar formation.

Discussion
Orbital cellulitis, an infection of the orbital soft tissues posterior to the orbital septum may be associated with serious complications including vision loss and can be life threatening. Preseptal cellulitis is more common than orbital cellulitis but has favorable prognosis [1]. Early diagnosis and proper treatment is essential to minimize vision loss and life threatening complications [2,3].
In case 1 discussed above, patient had swelling, redness of both eyes and abscess of left upper eyelid suggestive of orbital inflammatory condition. Differential diagnosis includes other conditions causing swelling and redness of eyelids such as angioedema, insect bites, cavernous sinus thrombosis. But considering there was no history of insect bite, allergy and clinical picture of abscess of eyelid, a diagnosis of preseptal cellulitis was made.
In case 2, patient had periorbital dermal necrosis and black eschar formation. Differential diagnosis of eschar formation included mucormycosis and anthrax. But pus culture helped to rule out these conditions. Though there was history of insect bite, considering the clinical picture of eyelid swelling with atypical findings and pus culture, a diagnosis of preseptal cellulitis was made.
Orbital cellulitis can have atypical presentation in patients with uncontrolled diabetes mellitus which without timely intervention, can lead to life threatening complications [4]. Both the patients discussed above, were known cases of diabetes with uncontrolled blood sugar levels. Control of blood sugar levels had helped in effectively controlling the orbital inflammations.
Preseptal cellulitis can progress posteriorly into the orbit and lead to significant ocular and CNS complications. Preseptal cellulitis is caused most commonly by bacteria. Gram positive cocci (Staphylococcus and Streptococcus species) are the most prevalent microorganisms. Adenovirus, herpes simplex and varicella zoster are also associated. In immunocompromised patients, fungal aetiology must be suspected. Orbital cellulitis most commonly occurs due to the spread of infection from the adjacent paranasal sinuses or periorbital structures to the orbit or through heamatogenous spread.
It can also occur following direct inoculation from trauma. Staphylococcus aureus, Streptococcus pneumoniae and beta-haemolytic streptococci, Haemophilus influenza type B are the most common bacteria that can cause orbital cellulitis. Swelling can lead to proptosis and compression of orbital structures [5]. Typically patients presents with pain, redness of eye, proptosis, and ophthalmoplegia. In severe cases, compressive optic neuropathy can occur. Infection from orbital and preseptal cellulitis can spread into the cavernous sinus. Orbital cellulitis causing fatal complication of cavernous sinus thrombosis has been reported [6].
Burkholderia pseudomallei is a gram negative saprophyte bacterium, that causes Melidiosis, an infectious disease. It spreads through contact with soil and water. It is life threatening as it can lead to fulminant septicaemia. Orbital and periorbital infection is mainly due to spread from contiguous structures like paranasal sinuses, eyelids etc., Ischemic optic neuropathy can occur due to septic vasculitis or by compression of infected material. Subperiosteal abscess may cause displacement of globe and restriction of ocular movements. Orbital abscess may cause marked proptosis, vision loss and ophthalmoplegia [7].
Mucormycosis, which is aggressively invasive with rapid progression has a predilection for diabetics or immunocompromised. Despite aggressive antifungal treatment, fungal orbital cellulitis has a high mortality rate. Soon after the diagnosis is confirmed, orbital exenteration may be necessary [8].
A detailed medical history and visual acuity, along with complete physical examination, and laboratory and radiologic testing will help narrow the differential diagnosis.
Early diagnosis and initiation of treatment is very essential in management of orbital/preseptal cellulitis. It can have variable presentation, especially in diabetic patients as exemplified above -case 1 diagnosed as Melioidosis and case 2 mimicking as anthrax/mucormycosis with eschar formation. Melioidosis is a significant opportunistic infection with a high mortality rate in immunocompromised patients [9].
Treatment options for orbital cellulitis in diabetics include control of diabetes, oral and intravenous antibiotics. In cases with subperiosteal and intraorbital abscess, surgical drainage is indicated in addition to antibiotics. In case 1, drainage of left upper eyelid abscess was done. In patients with orbital compartment syndrome, emergency canthotomy and cantholysis should be performed. In both the cases discussed above, there were no signs of orbital compartment syndrome or optic nerve involvement.
Conclusion
Orbital cellulitis in diabetics, immunocompromised individuals, can have atypical presentations and is rapidly fatal. Any symptom or sign in a diabetic should not be ignored. Thus, in orbital /preseptal cellulitis emphasis should be on early diagnosis and treatment based on pus culture sensitivity and imaging data. Early diagnosis and prompt treatment may prevent the need for destructive procedures like exenteration in rapidly fulminating conditions and thereby avoid morbidity.
[1]. Chaudhry IA, Shamsi FA, Elzaridi E, Al-Rashed W, Al-Amri A, Al-Anezi F, Outcome of treated orbital cellulitis in a tertiary eye care center in the middle eastOphthalmology 2007 114(2):345-54.10.1016/j.ophtha.2006.07.05917270683 [Google Scholar] [CrossRef] [PubMed]
[2]. Jones DB, Steinkuller PG, Strategies for the initial management of acute preseptal and orbital cellulitisTrans Am Ophthalmol Soc 1988 86:94-108. [Google Scholar]
[3]. Lee S, Yen MT, Management of preseptal and orbital cellulitisSaudi J Ophthalmol 2011 25(1):21-29.10.1016/j.sjopt.2010.10.00423960899 [Google Scholar] [CrossRef] [PubMed]
[4]. Karambelkar VH, Joshi BS, Sharma A, Professor A, Orbital cellulitis – an unusual first clinical presentation in undiagnosed diabetic patientInt J Recent Trends Sci Technol 2013 9(2):248-49. [Google Scholar]
[5]. Lam Choi VB, Yuen HKL, Biswas J, Yanoff M, Update in pathological diagnosis of orbital infections and inflammationsMiddle East Afr J Ophthalmol 2011 18(4):268-76.10.4103/0974-9233.9012722224014 [Google Scholar] [CrossRef] [PubMed]
[6]. Bilir BE, A rare complication of orbital cellulitis in a diabetic case: Cavernous sinus thrombosisJ Kartal Train Res Hosp 2016 27(3):233-37.10.5505/jkartaltr.2016.36097 [Google Scholar] [CrossRef]
[7]. Detporntewan P, Suankratay C, Orbital infection caused by Burkholderia pseudomallei: A mini-reviewJ Infect Dis Antimicrob Agents 2011 2929(2):99-103. [Google Scholar]
[8]. Farooq AV, Patel RM, Lin AY, Setabutr P, Sartori J, Aakalu VK, Fungal orbital cellulitis: presenting features, management and outcomes at a referral centerOrbit 2015 34(3):152-59.10.3109/01676830.2015.101451225906127 [Google Scholar] [CrossRef] [PubMed]
[9]. Lim RSM, Flatman S, Dahm MC, Sinonasalmelioidosis in a returned traveller presenting with nasal cellulitis and sinusitisCase Rep Otolaryngol 2013 2013:92035210.1155/2013/92035223936707 [Google Scholar] [CrossRef] [PubMed]