Introduction
Periodontal diseases are polymicrobial infections characterised by inflammation within the periodontal tissues. If left untreated in the initial stages, it leads to the progressive destruction of the periodontal ligament, alveolar bone and cementum [1,2]. Clinically these conditions manifest themselves by periodontal pocket formation, and at times are associated with gingival recession. In the posterior sextants, the progression of periodontal diseases results in invasion of the bifurcation and trifurcations of the multirooted teeth, which is termed as furcation involvement. Furcation involvement is usually seen in the maxillary and mandibular first molars as they are the teeth which are exposed to plaque for longer duration [3]. Furcation areas, if affected with periodontal diseases, present some of the greatest challenges to the success of periodontal therapy owing to its complex anatomic morphology, that is immensely strenuous and frequently inappropriate for adequate debridement.
The literature search reveals varying incidences of furcation involvement by different authors. Bissada NF et al., reported an incidence of 30.9% furcation involved molars in Egyptian skulls, Svardstrom G et al., reported 17-22 % of prevalence of furcation involvement in molars, while Ross IF et al., reported 90% and 35% incidence of furcation involvement in maxillary and mandibular molars respectively [4-6]. Furcation involvement is more common in maxillary molars than in the mandibular molars owing to the complex anatomy, bone density and inaccessibility of the surfaces for proper cleaning. The other reasons include the difficulties in properly diagnosing the presence and severity of destruction in furcation involved teeth.
Classification of diseases or conditions is known to be useful for the purpose of diagnosis, establishing prognosis and treatment planning. Till date, a number of classifications have been proposed to categorise furcation involvements which are based either on the extent of horizontal probing depths [7-12] or the vertical extent of loss of alveolar bone or a combination of the two [13,14]. All of them present limitations, because of varied anatomy of the furcation defects which makes it almost impossible to correlate all possible clinical scenarios in a comprehensive and concise manner [15]. The currently popular classifications of the furcation involvement are arbitrarily based and heavily emphasize only on the horizontal or vertical probe penetration in to the furcation, which unfortunately has a very limited utility as far as devising an appropriate treatment plan for the concerned situation.
With a continuous improvement in the understanding of periodontal conditions and advent of better therapeutic modalities, it becomes imperative to maximise inclusion of differentials in clinical manifestations involving severity of alveolar bone destruction and gingival inter-relationships which will enable the clinician to address minute details during the treatment. This in fact has been one of the major limitations of the existing classification of furcation involvement. The proposed classification is one of the first attempts in developing a system which relates the severity of alveolar bone destruction horizontally as well as vertically in the furcation and the gingival positions, thus providing the examiner more accuracy in diagnosing the condition and optimising a precise treatment plan for the condition.
Proposed Classification:
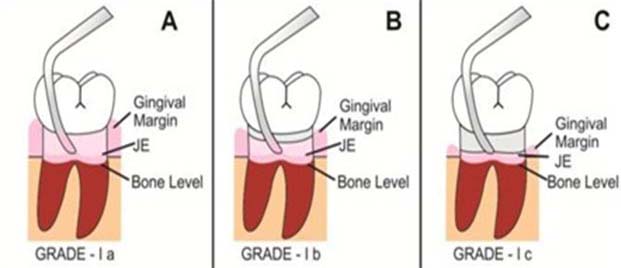
Grade I - This type of furcation involvement is an inchoate or elementary lesion which develops by mild to moderate and uniform periodontal destruction extending into the flute of the furca, and manifesting itself with increased probing depth. There are no radiographic changes associated with this type of lesion.
Furcation involvements may or may not be associated with recession of the marginal gingiva. So, depending on the position of marginal gingiva, it can be further sub-classified as:
Grade I a: It comprises of all the features of Grade I furcation involvement, with the normal position of gingival margin which is slightly coronal to the Cementoenamel Junction (CEJ).
Treatment Modality: The suggested treatment modality in such cases is scaling and odontoplasty [16].
Grade I b: It comprises of all features of Grade I furcation involvement, with the position of gingival margin, 0-3 mm apical to CEJ.
Treatment modality: The suggested treatment modality in such cases is scaling and odontoplasty along with coronally advanced flap for the root coverage [17].
Grade I c: It comprises of all features of Grade I furcation involvement, with the position of gingival margin which is more than 3 mm apical to CEJ and may lead to mucogingival problem [Table/Fig-1,2].
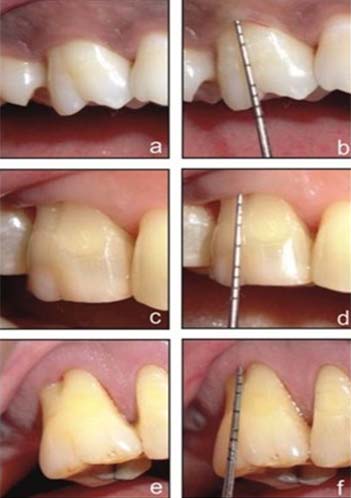
Grade I furcation involvement: a) Grade Ia; b) Grade Ib; c) Grade Ic.
Grade I furcation involvement: (a) Grade Ia; (b) Probe demonstrates gingival margin coronal to CEJ; (c) Grade Ib; (d) Gingival margin 3 mm apical to CEJ; (e) Grade Ic; (f) Gingival margin 5 mm apical to CEJ.
Treatment modality: The suggested treatment modality in such cases is scaling and odontoplasty alongwith correction of mucogingival problem which may include a subepithelial connective gingival graft for increasing the width of attached gingiva [18].
Grade II: This type of furcation involvement is a confined lesion which develops by moderate periodontal destruction of varying amount extending into the inter-radicular area, with an arched roof created by the furca and bordered by roots and bone. The lesion may appear on one or more aspects of the tooth without communicating with the other. Radiographs may reveal small areas of radiolucency in the furcation.
Depending upon the pattern of periodontal destruction in the furcation, this type of furcation involvement may further be sub-classified as:
Grade II Type 1– It comprises of all the features of Grade II furcation involvement, with uniform horizontal type of bone destruction in the furcation areas as assessed by clinical and/ or radiographic examination.
Grade II Type 2 – It comprises of all the features of Grade II furcation involvement, consisting of horizontal bone destruction with vertical component in the furcation areas as assessed by clinical and/ or radiographic examination.
Also, depending on the position of gingival margin, it can be further sub-classified as:
Grade II Type 1a– It comprises of all the features of Grade II Type 1 furcation involvement with the normal position of gingival margin which is slightly coronal to the CEJ.
Treatment modality: The suggested treatment modality in such cases is open flap debridement [19].
Grade II Type 1b – It comprises of all the features of Grade II Type 1 furcation involvement with the position of gingival margin which is 0-3 mm apical to the CEJ.
Treatment modality: The suggested treatment modality in such cases is open flap debridement alongwith root coverage procedure [19,20].
Grade II Type 1c– It comprises of all the features of Grade II Type 1 furcation involvement with the position of gingival margin which is more than 3 mm apical to the CEJ and may lead to mucogingival problem.
Treatment modality: The suggested treatment modality in such cases is open flap debridement along with correction of mucogingival problems [19-21].
Grade II Type 2a– It comprises of all the features of Grade II Type 2 furcation involvement with the normal position of gingival margin which is slightly coronal to the CEJ.
Treatment modality: The suggested treatment modality in such cases is open flap debridement which may be associated with bone augmentation or Guided tissue regeneration [19,20].
Grade II Type 2b– It comprises of all the features of Grade II Type 2 furcation involvement with the position of gingival margin which is 0-3 mm apical to the CEJ.
Treatment modality: The suggested treatment modality in such cases is open flap debridement which may be associated with bone augmentation or Guided tissue regeneration. Procedures for root coverage may include coronally advanced flap [19-21].
Grade II Type 2c– It comprises of all the features of Grade II Type 2 furcation involvement with the position of gingival margin which is more than 3 mm apical to the CEJ and may lead to mucogingival problem [Table/Fig-3].
Grade II furcation involvement: (a) Grade II Type 1a; (b) Grade II Type 1b; (c) Grade II Type 1c; (d) Grade II Type 2a; (e) Grade II Type 2b; (f) Grade II Type 2c.
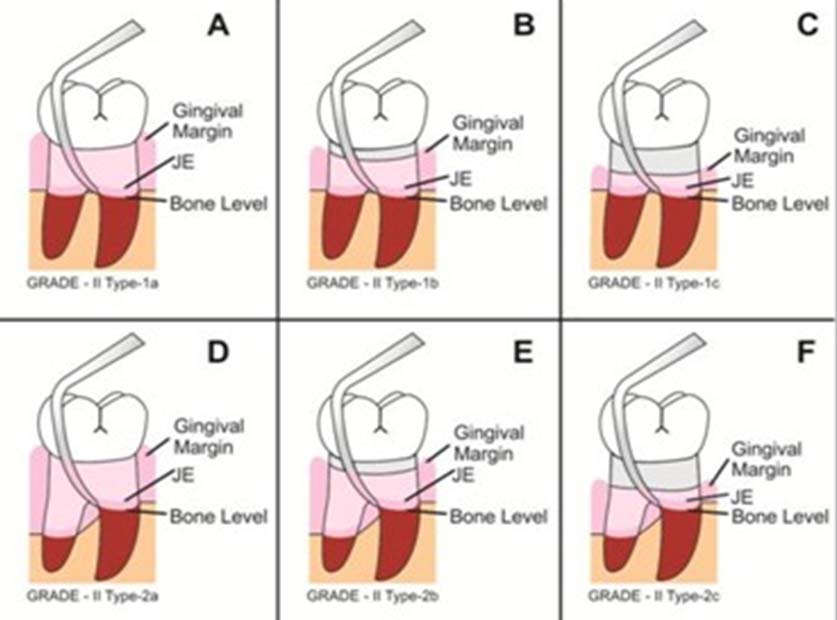
Treatment modality: The suggested treatment modality in such cases is open flap debridement which may be associated with bone augmentation or Guided tissue regeneration alongwith procedure for the correction of mucogingival problems [19-21].
Grade III – This type of furcation involvement is a complete lesion which develops by moderate to severe periodontal destruction in the furcation area permitting the passage of a probe bucco-lingually on the mandibular molars and bucco-mesially and bucco-distally on the maxillary molars. Radiographs may not reveal a distinct triangular radiolucency in the furcation in maxillary molars.
Depending upon the pattern of periodontal destruction in the furcation, this type of furcation involvement may further be sub-classified as:
Grade III Type 1– It comprises of all the features of Grade III furcation involvement, with uniform horizontal type of bone destruction in the furcation areas as assessed by clinical and/or radiographic examination.
Grade III Type 2– It comprises of all the features of Grade III furcation involvement, consisting of horizontal bone destruction with vertical component in the furcation areas as assessed by clinical and/or radiographic examination.
Also, depending on the position of gingival margin, it can be subclassified as-
Grade III Type 1a– It comprises of all the features of Grade III Type 1 furcation involvement with the normal position of gingival margin which is slightly coronal to the CEJ.
Treatment modality: The suggested treatment modality in such cases is open flap debridement which may be associated with bone augmentation, Guided tissue regeneration, root resection, bicuspidisation, tunnel preparation [19,20].
Grade III Type 1b– It comprises of all the features of Grade III Type 1 furcation involvement with the position of gingival margin which is 0-3 mm apical to the CEJ.
Treatment modality: The suggested treatment modality in such cases is open flap debridement which may be associated with bone augmentation or Guided tissue regeneration alongwith coronally advanced flap [19,20].
Grade III Type 1c– It comprises of all the features of Grade III Type 1 furcation involvement with the position of gingival margin which is more than 3 mm apical to the CEJ and may lead to mucogingival problem.
Treatment modality: The suggested treatment modality in such cases is open flap debridement which may be associated with bone augmentation or Guided tissue regeneration alongwith correction of mucogingival problems [19,20,22].
Grade III Type 2a– It comprises of all the features of Grade III Type 2 furcation involvement with the normal position of gingival margin which is slightly coronal to the CEJ.
Treatment modality: The suggested treatment modality in such cases is open flap debridement which may be associated with bone augmentation or Guided tissue regeneration or root resection [19,20].
Grade III Type 2b– It comprises of all the features of Grade III Type 2 furcation involvement with the position of gingival margin which is 0-3 mm apical to the CEJ.
Treatment modality: The suggested treatment modality in such cases is open flap debridement which may be associated with bone augmentation or Guided tissue regeneration alongwith coronally advanced flap [19,20].
Grade III Type 2c– It comprises of all the features of Grade III type 2 furcation involvement with the position of gingival margin which is more than 3 mm apical to the CEJ and may lead to mucogingival problem [Table/Fig-4].
Grade III furcation involvement: (a) Grade III Type 1a; (b) Grade III Type 1b; (c) Grade III Type 1c; (d) Grade III Type 2a; (e) Grade III Type 2b; (f) Grade III Type 2c.
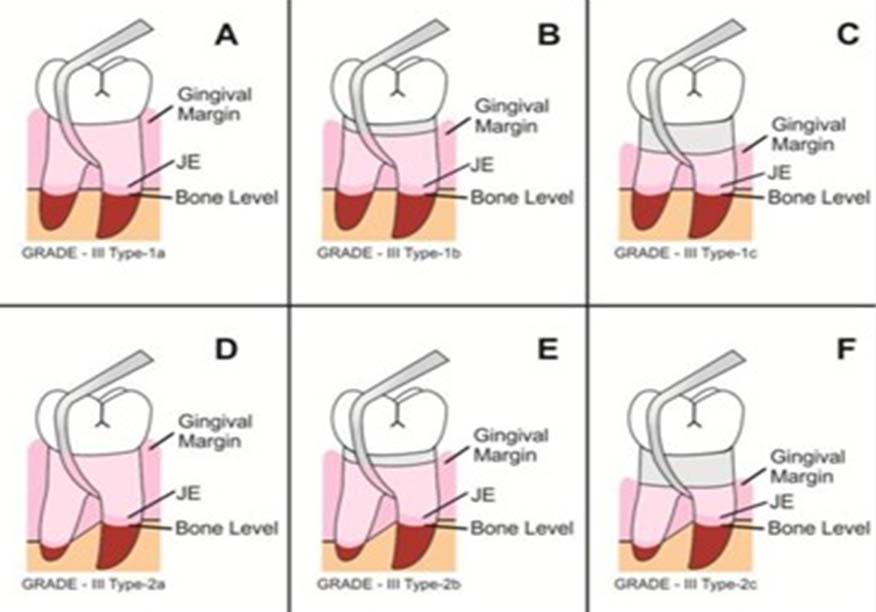
Treatment modality: The suggested treatment modality in such cases is open flap debridement which may be associated with bone augmentation or Guided tissue regeneration along with correction of mucogingival problems [19,21,22].
The recession is measured at the mid buccal region in this classification system.
The authors feel that a differentiation between horizontal and vertical component of bone destruction needs to be made in Grade II furcation and Grade III furcation involvement, since it has been time and again established that vertical bone destruction will be better amenable and responsive to regenerative therapeutic modalities [23,24]. Periodontal regenerative procedures have evolved over time with current techniques and have enabled the therapists to achieve success in increasingly difficult cases. The clinical characteristics of periodontal defects including the vertical or angular bone loss are more amenable to the regenerative therapy [25]. Though Grade II furcation defects themselves are self containing lesions, however, the vertical component will add up to the additional bone walls as a source of regenerative cells thus yielding optimum regenerative tissue post-therapy.
Therapeutic modalities for the correction of furcation defects have shown varying degrees of success, owing to the inherent complexities encountered within the hard and soft tissues in and adjacent to the furcation region. The ultimate goals of therapy in furcation areas includes arresting of the disease process, restoration of the lost attachment apparatus and maintaining the teeth in health and function with adequate aesthetics. However, the differences in furcation architecture along with the soft tissue positions pose a serious challenge to the efficacy of established modalities. In order to overcome these situations, specific treatment approaches have been proposed in each category of furcation involvement [Table/Fig-5].
Prognosis and treatment modalities decision tree.
| Grade I | Grade I a | Scaling, Odontoplasty. |
| Prognosis – Excellent |
| Grade I b | Same as Grade I a + Coronally advanced flap. |
| Prognosis- Good |
| Grade I c | Same as Grade I a + Correction of mucogingival problems. |
| Prognosis – Fair |
| Grade II | Grade II Type 1 a | Open flap debridement. |
| Prognosis- Excellent |
| Grade II Type 1 b | Same as Grade II Type 1 a+ Coronally advanced flap. |
| Prognosis - Good |
| Grade II Type 1 c | Same as Grade II Type 1a + Correction of mucogingival problems. |
| Prognosis – Fair |
| Grade II Type 2 a | Open flap debridement, Bone augmentation, Guided tissue regeneration. |
| Prognosis- Excellent |
| Grade II Type 2 b | Same as Grade II Type 2 a + Coronally advanced flap. |
| Prognosis - Good |
| Grade II Type 2 c | Same as Grade II Type 2 a + Correction of mucogingival problems. |
| Prognosis – Fair |
| Grade III | Grade III Type1 a | Open flap debridement, which may be associated with bone augmentation, Guided tissue regeneration, root resection, bicuspidisation, tunnel preparation |
| Prognosis – Good |
| Grade III Type1 b | Same as Grade III Type 1 a + Coronally advanced flap. |
| Prognosis - Fair |
| Grade III Type1 c | Same as Grade III Type 1 a + Correction of mucogingival problems. |
| Prognosis – Poor |
| Grade III Type2 a | Open flap debridement, Root resection, Bone augmentation, Guided tissue regeneration. |
| Prognosis – Good |
| Grade III Type 2 b | Same as Grade III Type 2 a + Coronally advanced flap. |
| Prognosis - Fair |
| Grade III Type2 c | Same as Grade III Type 2 a + Correction of mucogingival problems. |
| Prognosis – Poor |
The current comprehensive classification system is based on the evidence in the literature with regards to differing clinical conditions and therapeutic modalities utilized in the treatment of the same.
This classification system is probably the only one which takes into account the hard and soft tissue conditions around molars in periodontal diseases and can provide meaningful guidelines into advising a complete therapeutic correction of the defects.
Conclusion
Accurate diagnosis, accomplished treatment, precise management and long-term retention of multirooted teeth in periodontal diseases have long been a challenge to the general clinician as well as periodontal specialists. This new classification system of furcation involvement is a more efficient guide to the clinician in proper diagnosis and treatment planning. It is not only based on the destruction of the alveolar bone, but also takes into account the soft tissue positions which are an important but all the more neglected aspects in therapeutic modalities. Treatment advocated towards correction of both will enable the clinician and the patient in establishing periodontal structures in normal or near normal conditions making it more amenable for long-term retention through oral hygiene measures.
[1]. Page RC, Schroeder HE, Pathogenesis of chronic inflammatory periodontal disease: a summary of current workLab Invest 1976 33:235-49. [Google Scholar]
[2]. Offenbacher S, Periodontal diseases: pathogenesisAnn Periodontol 1996 1:821-78.10.1902/annals.1996.1.1.8219118282 [Google Scholar] [CrossRef] [PubMed]
[3]. Cattabriga M, Pedrazzoli V, Wilson TG Jr, The conservative approach in the treatment of furcation lesionsPeriodontol 2000 2000 22:133-53.10.1034/j.1600-0757.2000.2220109.x11276510 [Google Scholar] [CrossRef] [PubMed]
[4]. Bissada NF, Abdelmalek RG, Incidence of cervical enamel projections and its relationship to furcation involvement in Egyptian skullsJ Periodontol 1973 44:583-85.10.1902/jop.1973.44.9.5834518847 [Google Scholar] [CrossRef] [PubMed]
[5]. Svardstrom G, Wennstrom JL, Prevalence of furcation involvements in patients referred for periodontal treatmentJ Clin Periodontol 1996 23:1093-99.10.1111/j.1600-051X.1996.tb01809.x8997653 [Google Scholar] [CrossRef] [PubMed]
[6]. Ross IF, Thompson RH Jr, Furcation involvement in maxillary and mandibular molarsJ Periodontol 1980 51:450-54.10.1902/jop.1980.51.8.4506931205 [Google Scholar] [CrossRef] [PubMed]
[7]. Glickman I, Clinical Periodontology 1958 PhiladelphiaWB Saunders Co:694-96. [Google Scholar]
[8]. Goldman HM, Therapy of the incipient bifurcation involvementJ Periodontol 1958 29:11210.1902/jop.1958.29.2.112 [Google Scholar] [CrossRef]
[9]. Staffileno HJ, Surgical management of the furca invasionDent Clin North Am 1969 13:103-19. [Google Scholar]
[10]. Easley JR, Drennan GA, Morphological classification of the furcaJ Can Dent Assoc (Tor) 1969 35:104-07. [Google Scholar]
[11]. Ramfjord S, Periodontology and Periodontics 1979 PhiladelphiaW.B. Saunders [Google Scholar]
[12]. Hamp SE, Nyman S, Lindhe J, Periodontal treatment of multirooted teeth. Results after 5 yearsJ Clin Periodontol 1975 2:126-35.10.1111/j.1600-051X.1975.tb01734.x1058213 [Google Scholar] [CrossRef] [PubMed]
[13]. Tarnow D, Fletche P, Classification of the vertical component of furcation involvementJ Periodontol 1984 55:283-84.10.1902/jop.1984.55.5.2836588186 [Google Scholar] [CrossRef] [PubMed]
[14]. Hou G-L, Tsai C-C, Cervical enamel projection and intermediate bifurcational ridge correlated with molar furcation involvementsJ Periodontol 1997 68:687-93.10.1902/jop.1997.68.7.6879249641 [Google Scholar] [CrossRef] [PubMed]
[15]. Avila-Ortiz G, De Buitrago JG, Reddy MS, Periodontal regeneration–Furcation defects: A systematic review from the AAP regeneration workshopJ Periodontol 2015 86(Suppl):S108-S130.10.1902/jop.2015.13067725644295 [Google Scholar] [CrossRef] [PubMed]
[16]. Parihar AS, Katoch V, Furcation Involvement & Its TreatmentJ Adv Med Dent Sci Res 2015 3:81-87. [Google Scholar]
[17]. Zucchelli G, Marzadori M, Mele M, Stefanini M, Montebugnoli L, Root coverage in molar teeth: A comparative controlled randomized clinical trialJ Clin Periodontol 2012 39:1082-88.10.1111/jcpe.1200222943446 [Google Scholar] [CrossRef] [PubMed]
[18]. Harris RJ, Root coverage in molar recession: Report of 50 consecutive cases treated with subepithelial connective tissue graftsJ Periodontol 2003 74:703-08.10.1902/jop.2003.74.5.70312816304 [Google Scholar] [CrossRef] [PubMed]
[19]. Al-Shammari KF, Kazor CE, Wang HL, Molar root anatomy and management of furcation defectsJ Clin Periodontol 2001 28:730-40.10.1034/j.1600-051X.2001.280803.x11442732 [Google Scholar] [CrossRef] [PubMed]
[20]. Marinescu AG, Carligeriu V, Nica L, Onisei D, Evaluation of treatment techniques for advanced (grade ii–iv) furcation defects. A literature review of the regenerative methodsTMJ 2011 61:115-23. [Google Scholar]
[21]. Deo V, Gupta S, Ansari S, Kumar P, Yadav R, Evaluation of effectiveness of connective tissue graft as a barrier with bioresorbable collagen membrane in the treatment of mandibular Class II furcation defects in humans: 4-year clinical resultsQuintessence Int 2014 45:15-22. [Google Scholar]
[22]. Pontoriero R, Lindhe J, Guided tissue regeneration in the treatment of degree III furcation defects in maxillarv molarsJ Clin Periodontol 1995 22:810-12.10.1111/j.1600-051X.1995.tb00265.x8682929 [Google Scholar] [CrossRef] [PubMed]
[23]. Klein F, Kim T, Hassfeld S, Staehle H, Reitmeir P, Holle R, Radiographic defect depth and width for prognosis and description of periodontal healing of infrabony defectsJ Periodontol 2001 72:1639-46.10.1902/jop.2001.72.12.163911811498 [Google Scholar] [CrossRef] [PubMed]
[24]. Cortellini P, Pini Prato G, Tonetti MS, Periodontal regeneration of human intrabony defects with titanium reinforced membranes. A controlled clinical studyJ Periodontol 1995 66:797-98.10.1902/jop.1995.66.9.7977500246 [Google Scholar] [CrossRef] [PubMed]
[25]. Schallhorn RA, McClain PK, Periodontal regeneration: Management of periodontal osseous defects by the periodontist-dental hygienist teamJ Evid Based Dent Pract 2014 14:42-45.10.1016/j.jebdp.2014.04.00824929588 [Google Scholar] [CrossRef] [PubMed]