Massive Pyonephrosis Presenting as a Mammoth Tumour in Pregnancy: A Case Report
Shubha Rao1, Shyamala Guruvare2, Rajagopal Kadavigere3, PS Roopa4
1 Assistant Professor, Obstetrics and Gynaecology, Kasturba Medical College, Manipal, Karnataka, India.
2 Associate Professor, Obstetrics and Gynaecology, Kasturba Medical College, Manipal, Karnataka, India.
3 Professor, Radiology, Kasturba Medical College, Manipal, Karnataka, India.
4 Associate Professor, Obstetrics and Gynaecology, Kasturba Medical College, Manipal, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Shyamala Guruvare, Associate Professor, Obstetrics and Gynaecology, Kasturba Medical College, Manipal-576104, Karnataka, India.
E-mail: shyamaladoc@gmail.com
The overall incidence of ovarian tumours in pregnancy is 2.4-5.7% and because of the asymptomatic nature of ovarian mass it is usually diagnosed in late pregnancy when there may be symptoms produced by it. Due to the similarity of symptoms, there has always been perplexity when a patient presents with mass per abdomen in pregnancy. During pregnancy, mild hydronephrosis is considered a normal phenomenon and may be present in up to 90% of pregnancies. Dilation is usually more pronounced on the right kidney and after mid-pregnancy. Here, we present a case which presented as a huge abdominal mass in pregnancy which was mistaken to be an ovarian mass in pregnancy and then later diagnosed as pyonephrosis.
High risk pregnancy, Ovarian tumour, Pyonephrosis
Case Report
A 45-year-old Gravida 3 Para 2 Living 2 was admitted at 28 weeks of gestation with complaints of left sided pain abdomen with few episodes of vomiting since one week. Pain was more present in the lower abdomen and appeared to be continuous and pricky in nature. There were no aggravating factors but she was given analgesics following which pain subsided for a while only to reappear in a few hours. Her present pregnancy was uneventful with regular antenatal care as scheduled.
At 28 weeks she presented with pain abdomen for a week associated with few episodes of vomiting. She was afebrile and general condition was unremarkable. On examination, abdomen appeared over distended. Fetus was in longitudinal lie and Foetal heart was heard in left spino-umbilical line. The symptoms wrongly held to believe that the cause of the acute pain abdomen with an over distended abdomen could possibly be an ovarian tumour in pregnancy.
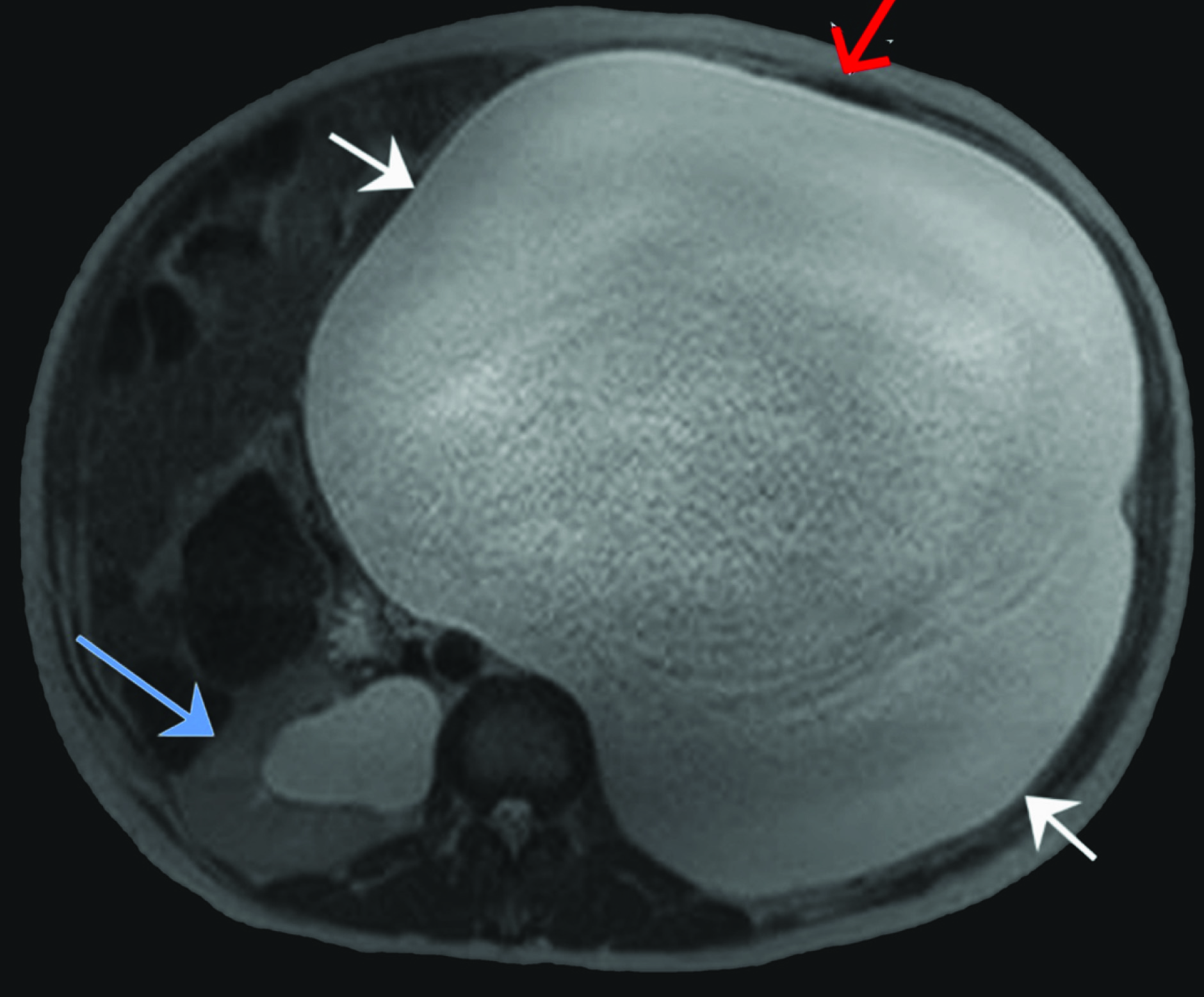
On Ultrasonography(USG) foetal growth was corresponding to the gestational age with normal liquor and estimated foetal weight of 1.2 kg. A large thin walled cystic lesion occupying entire upper abdomen above the uterus and left lumbar region was noted with homogenous low level internal echoes and few peripheral incomplete thin septations. A provisional diagnosis of mucinous cyst or dermoid cyst was made. This diagnosis further consolidated our prior diagnosis of ovarian tumour in pregnancy. However on investigating further in MRI of abdomen and pelvis the mass was diagnosed to be gross hydronephrosis with pelviureteric junction obstruction [Table/Fig-1a,b].
T2 weighted axial MR shows a large cystic lesion (white arrows) in the left renal fossa displacing the descending colon anteriorly (red arrow) suggestive of gross left hydronephrosis. Left renal parenchyma is not visualised. Mild right hydronephrosis noted (blue arrow)
T2 weighted coronal MR shows large cystic lesion in left hemiabdomen crossing the midline (white arrows). Intrauterine foetus is seen insitu (red arrow).

In view of the above findings Urology consultation was sought for. Under local anaesthesia, USG guided left percutaneous nephrostomy was done with 5 litres of pus being drained; a pigtail catheter was kept in situ for continuous drainage until delivery. Pus culture did not show any growth. Post procedure she was given ceftriaxone. Two weeks later the pigtail catheter had to be replaced by a Foley’s catheter in view of blocked catheter and accumulation of pus.
Subsequently, she had antenatal follow ups at her hometown. Unfortunately, when she visited us after six weeks, we found Foetal demise. She underwent elective lower segment caesarean section with sterilization in view of previous two caesareans and delivered a macerated female baby weighing 2.0kg.
She has been discharged with percutaneous nephrostomy and Foleys catheter in situ and asked to be reviewed after six weeks for pyeloplasty.
Discussion
Pregnancy is a condition where there is a physiological dilation of the urinary collecting system, however it can become symptomatic and if left untreated, may endanger the life of both the mother and fetus [1]. Dilation of the pelvicalyceal system is referred to as hydronephrosis and when this dilation is complicated by infection, it is called as pyonephrosis [2]. In pregnancy the most common cause of hydronephrosis is renal calculi but the occurrence is rare (0.04%) [3] compared to normal adults where the most common cause of hydronephrosis is congenital stenosis of uretero-pelvic junction. However, conditions such as ovarian cysts or tumours, ascites are a list of differentials that mimic a case of hydronephrosis [4] and in pregnancy the diagnosis becomes more difficult due to a distended abdomen which may prove a hindrance as the clinical examination would not prove to be conclusive.
There have been many cases of mistaken diagnosis. Similar to our case Nerli RB et al., explored a case of giant hydronephrosis which was intra-operatively diagnosed as giant hydronephrosis and a higher consult was sought for. However, this patient was treated with J stenting unlike our patient who had undergone percutaneous nephrostomy [5]. Balakrishnan T et al., reported an antenatal patient with acute pain abdomen similar to our case was diagnosed with hydronephrosis. However this patient underwent nephrostomy followed by nephrectomy. This highlights the importance of diagnosis and timely intervention especially during the antenatal period [6].
Percutaneous nephrostomy is the most common surgical procedure and also a life saving procedure done with a high success rate and often used in the setting such as seen in our case of pyonephrosis [7]. Shullai WK et al., recently reported two antenatal patients who were diagnosed with pyonephrosis [8]. When medical management failed to prove effective, percutaneous nephrostomy proved to be successful in both of the patients.
Conclusion
Pyonephrosis complicating pregnancy should be treated with utmost importance and most commonly used procedure is percutaneous nephrostomy. Pyonephrosis is life endangering condition which if allowed to progress may result in maternal mortality and morbidity. The diagnosis becomes difficult as the clinical symptoms are similar to various other conditions such as ovarian cysts/tumour, ascites thereby help of imaging modalities such as MRI makes the diagnosis easier and also treatment can be begun earlier to reduce morbidity. It should be stressed upon the need of frequent visits in these patients, lack of which may result in maternal and Foetal morbidity and mortality.
[1]. Puskar D, Balagovic I, Filipovic A, Knezović N, Kopjar M, Huis M, Symptomatic physiologic hydronephrosis in pregnancyEur Urol 2001 39:260-63.10.1159/00005244911275715 [Google Scholar] [CrossRef] [PubMed]
[2]. Mediavilla E, Ballestero R, Correas MA, Gutierrez JL, About a case report of giant hydronephrosisCase Reports in Urology 2013 2013:25796910.1155/2013/25796924191226 [Google Scholar] [CrossRef] [PubMed]
[3]. Haller H, Mozetic V, Topljak-Polik D, Randic LJ, Fuckar Z, Management and complications of urolithiasis during pregnancyInt J Gynaecol Obstet 1993 40(2):135-39.10.1016/0020-7292(93)90373-5 [Google Scholar] [CrossRef]
[4]. Yang WT, Metreweli C, Giant hydronephrosis in adults: the great mimic. Early diagnosis with ultrasoundPostgrad Med J 1995 71:409-12.10.1136/pgmj.71.837.4097567732 [Google Scholar] [CrossRef] [PubMed]
[5]. Nerli RB, Mungarwadi A, Mudegowdar AS, Patil A, Hiremath MB, Ghagane S, A giant hydronephrosis mistakenly diagnosed as ovarian tumour in a pregnant womanUrol Case Rep 2015 4:20-21.10.1016/j.eucr.2015.10.00226793569 [Google Scholar] [CrossRef] [PubMed]
[6]. Balakrishnan T, Narayana D, A diagnostic pitfall in a patient with acute abdominal pain: congenital hydronephrosis/hydroureter misdiagnosed as hydrosalpinxOpen Access Library Journal 2015 1:1-5.10.4236/oalib.1100701 [Google Scholar] [CrossRef]
[7]. Li AC, Regalado SP, Emergent percutaneous nephrostomy for the diagnosis and management of pyonephrosisSemir Intervent Radiol 2012 29(3):218-25.10.1055/s-0032-132693223997415 [Google Scholar] [CrossRef] [PubMed]
[8]. Shullai WK, Agarwal M, Reddy K, Singh AS, Successful pregnancy outcome in two patients with pyonephrosis treated with percutaneous nephrostomyAsian Journal of Medical Sciences 2016 7:109-11.10.3126/ajms.v7i2.10446 [Google Scholar] [CrossRef]