Marsupialization of Inflammatory Dentigerous Cyst Associated with Pulpotomised Primary Second Molar-A Case Report
Ranu Bhandari1, Seema Thakur2, Parul Singhal3, Deepak Chauhan4, Cheranjeevi Jayam5
1 Postgraduate Student, Department of Pedodontics, H.P. Government Dental College, Shimla, Himachal Pradesh, India.
2 Head, Department of Pedodontics, H.P. Government Dental College, Shimla, Himachal Pradesh, India.
3 Assistant Professor, Department of Pedodontics, H.P. Government Dental College, Shimla, Himachal Pradesh, India.
4 Senior Lecturer, Department of Pedodontics, H.P. Government Dental College, Shimla, Himachal Pradesh, India.
5 Lecturer, Department of Pedodontics, H.P. Government Dental College, Shimla, Himachal Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ranu Bhandari, Jaswal Bhawan, North Oak, Sanjauli, Shimla-171006, Himachal Pradesh, India.
E-mail: Dr.ranubhandari@gmail.com
Pulpotomy of a deciduous tooth is a standard procedure done in paediatric patients. Quite a few times it can give rise to side effects, one of the side effects being cyst formation in the periradicular area of pulpotomised tooth. Diagnosis of this cyst is difficult, as classifying them under radicular cyst or dentigerous cyst is reported dilemma in literature. This paper discusses the differential diagnosis of such periradicular cyst, the probable theory of pathophysiology of the infected dentigerous cyst, and treatment by marsupialization technique. The successful eruption of a horizontally impacted involved tooth was noted, with the alignment of the arch and healthy bone formation after treatment.
Impacted tooth, Jaw cysts, Mixed dentition
Case Report
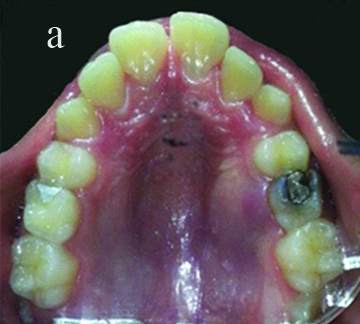
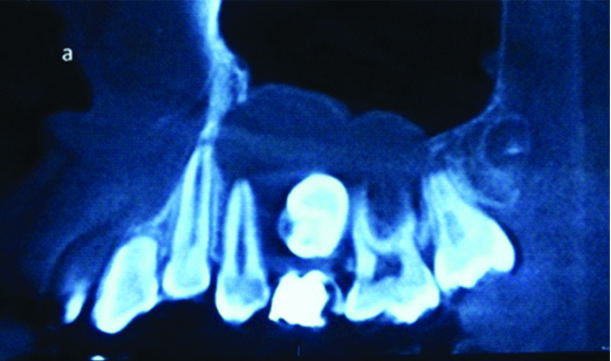
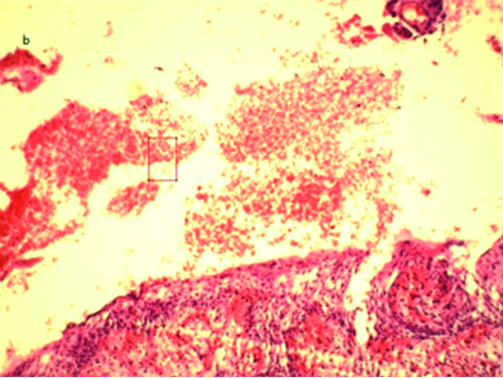
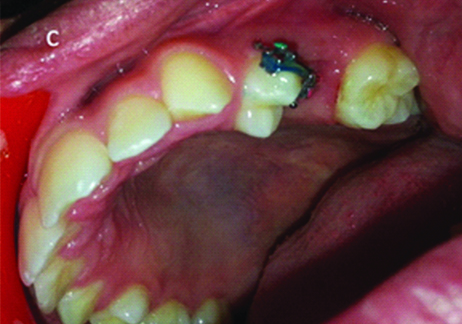
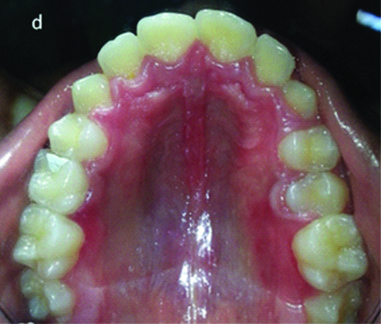
A 12 Years eight-month-old female patient reported in Department of Paediatric and Preventive Dentistry with a chief complain of pain and swelling on the posterior palate since three days. Medical history of the patient was taken and it was unremarkable. The pain was dull and gnawing. There was a discharge of blood-stained fluid from the swelling after brushing one day before, after which there was some relief from the pain. The Patient’s parents gave a history of treatment done for deciduous maxillary left second molar in same department, It was concluded through provided documents that pulpotomy followed by silver amalgam restoration was done three years back. Palatal Swelling concerning deciduous maxillary left second molar was present. The swelling was soft and tender, extending from the mesial surface of the permanent maxillary left first premolar till the mesial surface of the permanent maxillary left first molar. The swelling size was 3×2 cm [Table/Fig-1a]. Additional findings were increased overjet of 6 mm and maxillary and mandibular teeth are malaligned [Table/Fig-1b,c]. After clinical examination and history taking, provisional diagnosis of radicular cyst or dentigerous cyst was made. IOPA, Occlusal radiograph and CBCT (Panoramic View) were advised, which showed a well-defined radiolucency involving the apices of maxillary left first premolar, apices of the deciduous maxillary left second molar and an horizontally impacted permanent maxillary left second premolar [Table/Fig-2a,b and c]. To delineate the exact extent of the cystic margins CBCT was advised. In sagittal view [Table/Fig-3a], extension anteriorly was from distal surface of left maxillary canine, up till mesial surface of the maxillary left second molar posteriorly, In frontal view of CBCT [Table/Fig-3b], the cyst was seen invading the maxillary antrum and also the floor of the nose, and In transverse view [Table/Fig-3c], horizontally impacted permanent maxillary left second premolar with root facing buccally was seen. Additionally cortical expansion along with the breach in continuity can be appreciated in the palatal aspect of transverse section in CBCT. Exploratory puncture biopsy was performed, which produced a bloody liquid. Parents were narrated the treatment options of surgical removal of whole of the cyst which would harm the vital adjacent structures and marsupialization technique which was a conservative treatment. Pros and cons of both the treatments were explained. Marsupialization was opted by patient as well as the doctor for its relative conservative approach. Consent was taken from both patient and parents followed by extraction of the left maxillary deciduous second molar [Table/Fig-4a] and removal of parts of the lesion for histopathology report. The microscopic findings of cystic lining showed thick stratified epithelium cells which were secondarily infected also cystic wall showed fibrous tissue [Table/Fig-4b]. Based on the clinicopathological findings, the final diagnosis was made as a dentigerous cyst which was secondarily infected. Benn A et al., carried out a clinicopathologic study on dentigerous cyst of inflammatory origin [1]. They found all of the cysts were moderately or intensely inflamed and were lined predominantly or entirely by nonkeratinized stratified squamous epithelium that in some cases was markedly hyperplastic and exhibited anastomosing rete ridges mimicking radicular cysts. Therefore, the differentiation form radicular cyst was not possible.
Swelling present in the second quadrant with respect to the pulpotomised deciduous second molar.
Right lateral view showing increased overjet.

Left lateral view showing swelling in sulcus region with respect to maxillary deciduous second molar.

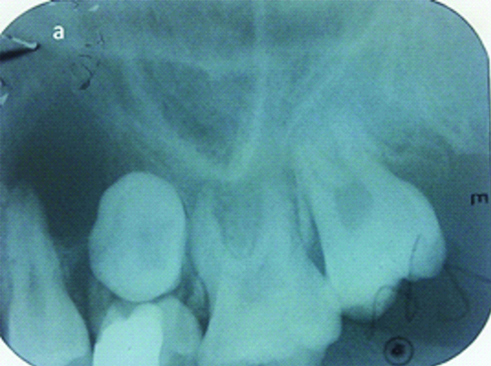
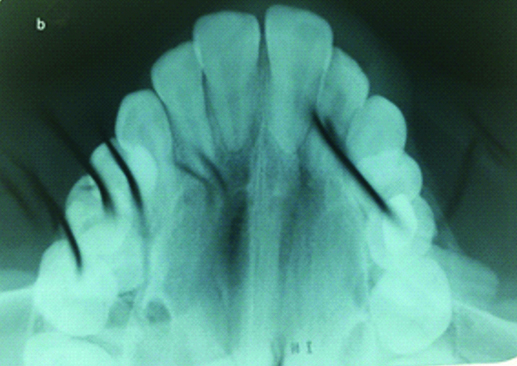
CBCT (Panoramic View) showing radiolucency involving the apices of permanent left first premolar, deciduous maxillary left second molar and horizontally impacted permanent maxillary left second premolar.
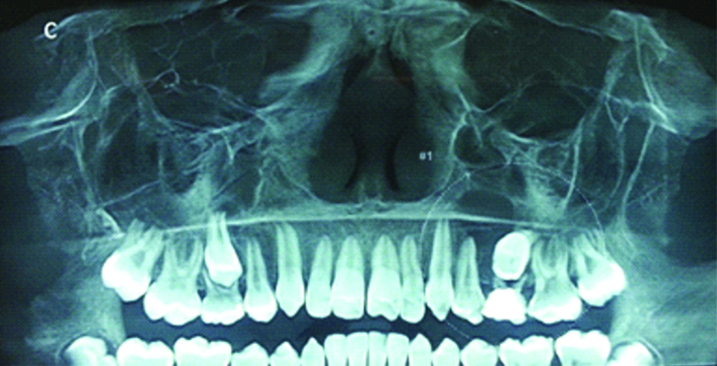
Sagittal view: extension anteriorly was from distal surface of left maxillary canine, up till mesial surface of the maxillary left second molar posteriorly.
Frontal view: the cyst was seen invading the maxillary antrum and also the floor of the nose.
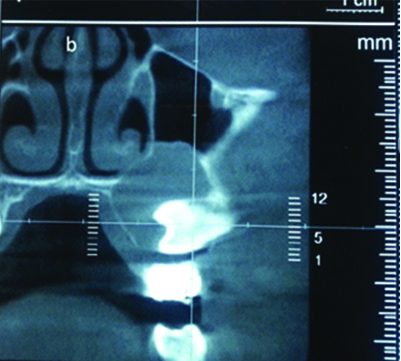
Transverse view: horizontally impacted permanent maxillary left second premolar with root facing buccally was seen, Also cortical expansion was evident in CBCT when viewed in all the three views.

Extraction of the left maxillary deciduous second molar and removal of parts of the lesion for histopathology report was done.

Histopathological image showing thick stratified epithelium cells and fibrous tissue. (4X, H&E staining).
The cystic lining was sutured to the gingiva. Buccal surface of the permanent maxillary left second premolar was visible Gauze piece in Betadine was placed in the cavity for one week to prevent primary wound closure. Amoxicillin with Clavulanic acid was prescribed, and the postsurgical period was uneventful. Suture removal was done after one week following which Impression of the maxillary teeth with the surgical opening was made. An acrylic appliance with jack screw, active labial bow, and acrylic plug were fabricated to maintain the patency of cystic cavity, and to correct the proclination of anterior maxillary teeth simultaneously [Table/Fig-5a,b]. The acrylic plug was reduced in every 15 days. There was some up-righting of permanent maxillary left second premolar seen at every appointment. To deviate the path of the impacted tooth, a bracket was placed on the same and permanent maxillary left first premolar and rubber band traction was applied [Table/Fig-5c]. After six months tooth became vertical [Table/Fig-5d] and there was a reduction in overjet. MBT appliance was given to correct prominent root of the permanent maxillary left second premolar and proper alignment of the arch. Formation of healthy bone with no residual cyst around the tooth root was evident after eight months [Table/Fig-6a,b]. Up righting of horizontally impacted tooth within one year of follow-up was evident [Table/Fig-6c,d].
Acrylic appliance with jack screw, active labial bow and the acrylic plug was fabricated to maintain the patency of cystic cavity, and to correct the proclination of maxillary anterior teeth simultaneously.

To deviate the path of the impacted tooth a bracket was placed on the same and permanent maxillary left first premolar and rubber band traction was applied.
Uprighting of left second premolar evident.
a) IOPA; and b) Occlusal radiograph showing up righting of the root of horizontally impacted tooth, and formation of healthy bone around the root of maxillary permanent second premolar. c): Maxillary and left lateral view’ and d) occlusal after one year follow-up showing some alignment of arch.

Discussion
Pulpotomy is a safe procedure. However, Malposition of the permanent tooth, delayed successor eruption, developmental enamel defects, discolored permanent enamel, and cyst formation are some of the quoted side effects after pulpotomy procedure in deciduous teeth [2].
In very few cases after this procedure radiolucency can be seen in the periapical region of the pulpotomised tooth [3]. These radiolucent space in relation with the succedaneous permanent tooth are mostly diagnosed as periapical granuloma or radicular cyst or dentigerous cyst. In the mixed dentition, any lesion originated via infected deciduous tooth lie in proximity to permanent successor follicle [3].
Dentigerous cysts is secondarily caused by the collection of fluid between tooth bud and Reduced Enamel Epithelium (REE). These cysts are usually secondarily infected, are diagnosed on routine examination, seen as radiolucency greater than 5 mm or when facial asymmetry is present because of lesions greater than 2 cm [4-6].
Upon examination radiographically and histologically, it shows deviation from usual presentation. In an infected dentigerous cyst, one can find ill-defined borders radiographically, and non-keratinized stratified squamous epithelium with elongated rete pegs histologically [7-9].
Radicular cysts are caused by the proliferation of epithelium residues known as cyst of Malassez of periodontal ligament, pulpal or periapical infection usually causes this proliferation [10]. They are commonly found cyst of the oral cavity, but studies have shown it to be rarely associated with the primary tooth. Lustmann J et al., in their study of 25 years found merely seven cases in a series of 1300 radicular cysts (0.5%) [11].
Over the years, many studies have concluded that the osteolytic lesions related to the unerupted succedaneous tooth, to be dentigerous cysts. They quote it to be inflammatory origin dentigerous cyst originating from the extrafollicular pathway. The pathophysiology of dentigerous cyst could be the stimulus from overlying infected deciduous tooth causing separation of reduced enamel epithelium and enamel resulting in cyst formation.
Benn A et al., performed a clinic-pathologic study of 15 cases, and he classified them as dentigerous cysts of inflammatory origin, [1]. Sometimes this type of cyst may not involve crown of permanent successor. De Castro LA et al., consider that this should not be considered as exclusion criteria [12], this was also supported by Lustmann J et al., [11].
One cannot say indubitably that all lesions illustrated by Benn A et al., Azaz B, Shaw W et al., can be diagnosed as dentigerous cysts [1,13,14]. Some of them shared cases where there were no strong criteria to differentiate between radicular and dentigerous cyst.
Shaw W et al., hypothesized that dentigerous cysts if formed in mixed dentition period, it may be formed by the fusion of periradicular cyst of deciduous tooth and reduced enamel epithelium of permanent succedaneous tooth [14].
Enucleation or marsupialization can treat the dentigerous cyst. Enucleation is a radical treatment comprising of removal of cystic lining along with involved teeth. Nevertheless, the recurrence rate is minimal [7,15]. Marsupialization or decompression is a more conservative approach; it helps by decreasing the intracystic pressure and spontaneous eruption of involved tooth [8]. Marsupialization technique is mostly used to treat dentigerous Cysts in growing children, as it is less invasive, does not harm involved permanent successor, and also teeth with open apices have substantial eruptive potential [4] with a much better prognosis [8].
Conclusion
The case represents the success of a marsupialization technique of a large dentigerous cyst without injuring the involved tooth. The maintenance and eruption of a permanent tooth is essential in establishing the occlusion and for the development of the alveolar process.
In selected cases, this therapeutic approach might be considered as a viable treatment modality to cure bone lesions, spontaneous eruption of the involved tooth and physiological bone growth.
[1]. Benn A, Altini M, Dentigerous cysts of inflammatory origin. A clinicopathologic studyOral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics 1996 81(2):203-09.10.1016/S1079-2104(96)80416-1 [Google Scholar] [CrossRef]
[2]. Pruhs RJ, Olen GA, Sharma PS, Relationship between formocresol pulpotomies on primary teeth and enamel defects on their permanent successorsJ Am Dent Assoc 1977 94(4):698-700.10.14219/jada.archive.1977.0353265330 [Google Scholar] [CrossRef] [PubMed]
[3]. Takiguchi M, Fujiwara T, Sobue S, Ooshima T, Radicular cyst associated with a primary molar following pulp therapy: a case reportInternational Journal of Paediatric Dentistry 2001 11(6):452-55.10.1046/j.0960-7439 .2001.00312.x11759106 [Google Scholar] [CrossRef] [PubMed]
[4]. Delbem AC, Cunha RF, Afonso RL, Bianco KG, Idem AP, Dentigerous cysts in primary dentition: report of 2 casesPediatric Dentistry 2006 28(3):269-72. [Google Scholar]
[5]. Daley TD, Wysocki GP, The small dentigerous cyst. A diagnostic dilemmaOral surgery, Oral Medicine, Oral Pathology, Oral Radiology and Endodontics 1995 79(1):77-81.10.1016/S1079-2104(05)80078-2 [Google Scholar] [CrossRef]
[6]. Bodner L, Woldenberg Y, Bar-Ziv J, Radiographic features of large cystic lesions of the jaws in childrenPediatric radiology 2003 33(1):3-6.10.1007/s00247-002-0816-212497227 [Google Scholar] [CrossRef] [PubMed]
[7]. Chi AC, Neville BW, Odontogenic Cysts and TumorsSurgical Pathology Clinics 2011 4(4):1027-91.10.1016/j.path.2011.07.00326837786 [Google Scholar] [CrossRef] [PubMed]
[8]. Martinez-Perez D, Varela-Morales M, Conservative treatment of dentigerous cysts in children: a report of 4 casesJournal of oral and maxillofacial surgery: official journal of the American Association of Oral and Maxillofacial Surgeons 2001 59(3):331-33.10.1053/joms.2001.2100611243619 [Google Scholar] [CrossRef] [PubMed]
[9]. Ertas U, Yavuz MS, Interesting eruption of 4 teeth associated with a large dentigerous cyst in mandible by only marsupializationJournal of oral and maxillofacial surgery: official journal of the American Association of Oral and Maxillofacial Surgeons 2003 61(6):728-30.10.1053/joms.2003.5014512796888 [Google Scholar] [CrossRef] [PubMed]
[10]. Kramer IR, Pindborg JJ, Shear M, International histological classification of tumors. Histological typing of odontogenic tumorsWorld Health Organization 1992 70(12):2988-94.10.1007/978-3-662-02858-2 [Google Scholar] [CrossRef]
[11]. Lustmann J, Shear M, Radicular cysts arising from deciduous teeth. Review of the literature and report of 23 casesInternational Journal of Oral Surgery 1985 14(2):153-61.10.1016/S0300-9785(85)80087-9 [Google Scholar] [CrossRef]
[12]. de Castro LA, Maia SRC, Maxillary osteolytic lesion in a 10-year-old girl: a dentigerous or radicular cyst? A case report and discussionRevistaportuguesa De Estomatologia E Cirurgiamaxilo-Facial 2012 53(1):24-8.10.1016/j.rpemd.2011.10.004 [Google Scholar] [CrossRef]
[13]. Azaz B, Shteyer A, Dentigerous cysts associated with second mandibular bicuspids in children: report of five casesASDC journal of Dentistry for Children 1973 40(1):29-31. [Google Scholar]
[14]. Shaw W, Smith M, Hill F, Inflammatory follicular cystsASDC Journal of Dentistry for Children 1980 47(2):97-101. [Google Scholar]
[15]. Desai RS, Vanaki SS, Puranik RS, Tegginamani AS, Dentigerous cyst associated with permanent central incisor: a rare entityJournal of the Indian Society of Pedodontics and Preventive Dentistry 2005 23(1):49-50.10.4103/0970-4388.1603015858310 [Google Scholar] [CrossRef] [PubMed]