Bilateral Unicondylar Hoffa Fracture Along with Tibial Spine Avulsion Injury in a Patient: Case Report
Sumit Gupta1, Jaswant Kumar2
1 Assistant Professor, Department of Orthopaedics, Lady Hardinge Medical College, New Delhi, India.
2 Assistant Professor, Department of Orthopaedics, Maulana Azad Medical College, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sumit Gupta, 8/3 Gulmohar Road, Shipra Sun City, Indirapuram, Near Regalia Heights, Ghaziabad-201014, Uttar Pradesh, India.
E-mail: docsumitgupta@gm ail.com
Coronal fractures of distal femur are complex intra articular fractures. Various cases of unicondylar and bicondylar Hoffa fractures have been reported in literature. Bilateral unicondylar Hoffa fracture is a very rare injury and it is not reported in literature to best of our knowledge. We report a case of bilateral unicondylar Hoffa fracture associated with tibial spine avulsion in right knee and possible mechanism of injury in same patient.
Bilateral Hoffa, Coronal Fracture, Distal Femur
Case Report
A 45-year-old male patient presented to Emergency Department with complains of pain and swelling of the both knee joints. According to the patient, he fell down from a moving auto rickshaw and got direct impact on both the knees simultaneously. On further evaluation, we inquired that his both the knees were in 900 of flexion at the time of impact. There were no associated injuries and patient was hemodynamically stable. There was no medical history of any other chronic illness.
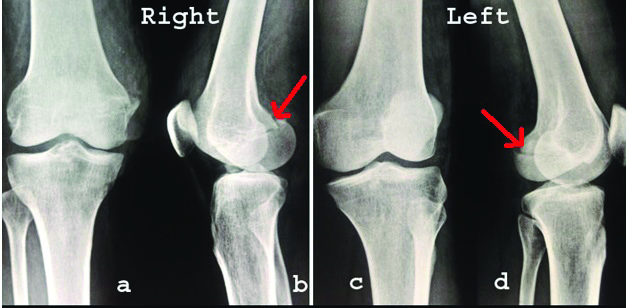
On local examination there was severe tenderness over both the knee joints. Although there were no external wound on both the knees, but on right knee there was superficial abrasion on anteromedial aspect of the knee joint. There were restrictions of knee joints movements and no distal neurovascular deficit in both lower limbs. Anteroposterior radiographs of both the knees were apparently normal except tibial spine avulsion in right knee joint. Lateral radiographs showed displaced medial and lateral condyle Hoffa fracture in right and left knee joints respectively [Table/Fig-1].
Plain anteroposterior radiograph: (a,c) of right and left knee was apparently normal and lateral views: (b,d) of right and left knee showing Hoffa fracture. (marked with red arrow)
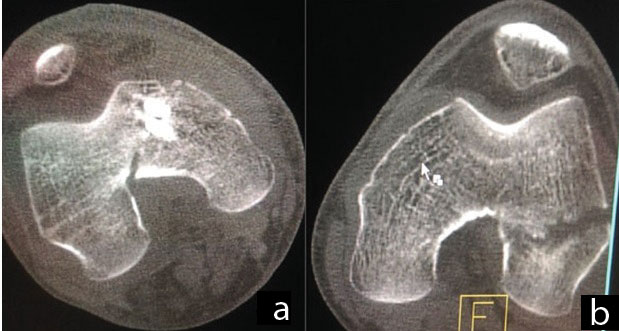
Non-contrast Computed Tomography (CT) of both the knees was performed to assess the exact pattern of fracture and to plan further management of fracture [Table/Fig-2].
Axial CT scan images of rightl (a) and left knee; (b) showing medial Hoffa and lateral Hoffa fracture respectively
Both the knee joints were operated with the patient in supine position. On the right side, arthoscopically assisted fixation with canulated cancellous screw (4.00 mm screw for tibial spine and 7.00 mm screw for Hoffa fracture) of tibial spine and medial Hoffa fracture was done, as there was abrasion on medial aspect of knee joint, which was not suitable for open reduction. On the left knee open reduction internal fixation with 7.00 mm canulated cancellous screw was done through lateral parapatellar approach.
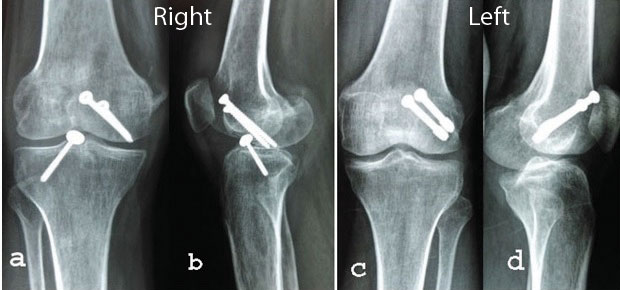
Postoperatively both knee joints were splinted with posterior above knee Plaster of Paris (POP) slab with 300 knee flexion for two weeks. After two weeks isometric muscles strengthen exercise and intermittent knee range of motion exercises were started. Patient was kept non weight bearing for six weeks after that partial weight bearing was started for next six weeks. Patient was allowed full weight bearing at three months of postoperatively after fracture had united radiologically [Table/Fig-3].
Follow up radiograph anteroposterior: (a,c) and lateral views; (b,d) of right and left knee joints respectively showing good union and no sign of avascular necrosis, osteoarthritis
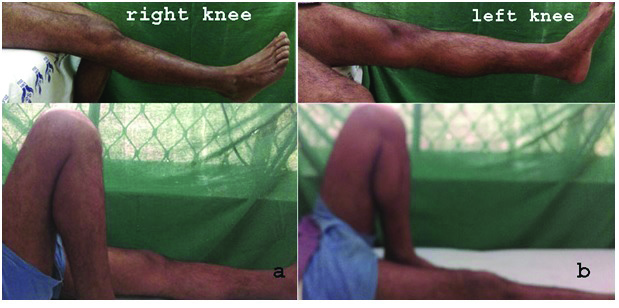
After one year of follow up, patient was having full range of motion of both the knee joints without any instability. There was no sign of avascular necrosis till last follow up [Table/Fig-4].
Clinical photograph at one year follow up showing range of motion of right knee (a) and left knee (b)
Discussion
Coronal fractures of femoral condyles are usually associated with high velocity trauma [1]. Lateral femoral condyle Hoffa fractures has been reported to be more common than medial condyle; probably as a result of physiological valgus of knee and greater anteroposterior diameter of lateral condyle than medial femoral condyle [2]. The specific mechanisms of injury of Hoffa fracture are unknown. However, lateral Hoffa fracture occurred due to anteroposterior directed force at the flexed abducted knee and medial condyle Hoffa fracture are due to direct force over medial side of the flexed knee [3].
AO/OTA (Orthopaedic Trauma Association) has classified the coronal fracture of distal femur as 33.B3.2, but these provide little insight about prognosis and treatment plan of the fracture [4]. Letenneur J et al., had classified Hoffa fracture in three types, based on distance of fracture line from posterior cortex of shaft of femur. Type I is vertical fracture of condyle parallel to posterior cortex of the femur, type II is variable size horizontal to condyle and type III is the oblique fracture of the condyle. This classification was to predict the prognosis for avascular necrosis of coronal fragments [5]. Ul Haq R et al., even proposed a sub classification of bicondylar fracture (AO/OTA 33-B3.3) into type B3.3a (conjoint bicondylar Hoffa) and type B3.3b (non conjoint bicondylar Hoffa) [6].
In our case, presentation was unique as there was lateral Hoffa fracture on left side and medial Hoffa fracture along with tibial spine avulsion on right side. This type of presentation has not been reported in literature to best of our knowledge.
The aim of treatment in Hoffa fracture is to obtain anatomical reduction and rigid fixation in order to allow early mobilization and restoration of function. These fractures are susceptible to displacement on flexion of knee and axial loading. There is little evidence to support non-operative management for these fractures [7,8]. There are various surgical approaches to access these fractures that include anterior midline, medial or lateral approaches with/without ancillary procedures like Gerdy’stubercule osteotomy to enhance exposure. All these surgical approaches have been used by various authors to achieve good functional results in Hoffa fracture [9-11].
With the advancement of arthroscopic procedures in knee joint, a few authors have also reported good early results with arthroscopic assisted fixation of Hoffa fracture [12]. However, arthoscopically assisted reduction of fracture and internal fixation is technically demanding. Advantages of arthoscopically assisted management in distal femur fracture include faster recovery as compared to standard open procedure, minimal soft tissue injury, less blood loss and evaluation of associated chondral and ligamentous injury.
Jarit GJ et al., had done a biomechanical study to assess the relative strength and stability of AP directed and PA directed screw fixation in the displaced coronal fracture of distal femur and concluded that PA screw fixation provide mechanical advantage than AP screw fixation. He also commented that surgical approach used to fix PA screw is more difficult and has risk of neurovascular injury [13]. However, there is still consensus to be reached in method of fixation (in terms of anterior/posterior direction of screw insertion and type/size/number of screws to be used).
In our patient, right knee underwent arthroscopic assisted fixation and left knee was operated with open reduction, and at one year follow up there was no loss of fixation or any sign of avascular necrosis of fragments and ROM of right and left knee are 00-1200 and 00-1300 respectively [Table/Fig-4].
Conclusion
Finally we conclude that if soft tissue condition is not allowed for open reduction of Hoffa fracture, arthroscopic assisted reduction and fixation provide good early clinical outcome. However, early open reduction and rigid internal fixation provide best result.
[1]. Nork SE, Segina DN, Aflatoon K, Barei DP, Henley MB, Holt S, The association between supracondylar-intercondylar distal femoral fractures and coronal plane fracturesJ Bone Joint Surg Am 2005 87(3):564-69.10.2106/JBJS.D.0175115741623 [Google Scholar] [CrossRef] [PubMed]
[2]. Dhillon MS, Mootha AK, Bali K, Prabhakar S, Dhatt SS, Kumar V, Coronal fractures of the medial femoral condyle: a series of 6 cases and review of literatureMusculoskelet Surg 2012 96(1):49-54.10.1007/s12306-011-0165-021904943 [Google Scholar] [CrossRef] [PubMed]
[3]. Calmet J, Mellado JM, GarcíaForcada IL, Giné J, Open bicondylar Hoffa fracture associated with extensor mechanism injuryJ Orthop Trauma 2004 18(5):323-25.10.1097/00005131-200405000-0001215105758 [Google Scholar] [CrossRef] [PubMed]
[4]. Muller ME, Nazarian S, Koch P, Schatzker J, The comprehensive classification of fracture of long bone 1990 BerlinSpringer-Verlag:144-145.10.1007/978-3-642-61261-9 [Google Scholar] [CrossRef]
[5]. Letenneur J, Labour PE, Rogez JM, Lignon J, Bainvel JV, Hoffa’s fractures. Report of 20 cases (author’s transl)Ann Chir 1978 32(3-4):213-19. [Google Scholar]
[6]. Ul Haq R, Modi P, Dhammi I, Jain AK, Mishra P, Conjoint bicondylar Hoffa fracture in an adultIndian J Orthop 2013 47(3):302-06.10.4103/0019-5413.11150923798763 [Google Scholar] [CrossRef] [PubMed]
[7]. Manfredini M, Gildone A, Ferrante R, Bernasconi S, Massari L, Unicondylar femoral fractures: therapeutic strategy and long-term results. Areview of 23 patientsActa Orthop Belg 2001 67(2):132-38. [Google Scholar]
[8]. Papadopoulos AX, Panagopoulos A, Karageorgos A, Tyllianakis M, Operative treatment of unilateral bicondylar Hoffa fracturesJ Orthop Trauma 2004 18(2):119-22.10.1097/00005131-200402000-0001214743034 [Google Scholar] [CrossRef] [PubMed]
[9]. Holmes SM, Bomback D, Baumgaertner MR, Coronal fractures of the femoral condyle: a brief report of five casesJ Orthop Trauma 2004 18(5):316-19.10.1097/00005131-200405000-0001015105756 [Google Scholar] [CrossRef] [PubMed]
[10]. Lewis SL, Pozo JL, Muirhead-Allwood WF, Coronal fractures of the lateral femoral condyleJ Bone Joint Surg Br 1989 71(1):118-20.10.1302/0301-620X.71B1.29149792914979 [Google Scholar] [CrossRef] [PubMed]
[11]. Garofalo R, Wettstein M, Fanelli G, Mouhsine E, Gerdy tubercle osteotomy in surgical approach of posterolateral corner of the kneeKnee Surg Sports Traumatol Arthrosc 2007 15(1):31-35.10.1007/s00167-006-0121-y16951979 [Google Scholar] [CrossRef] [PubMed]
[12]. Atesok K, Doral MN, Whipple T, Mann G, Mei-Dan O, Atay OA, Arthroscopy-assisted fracture fixationKneeSurg Sports Traumatol Arthrosc 2011 19(2):320-29.10.1007/s00167-010-1298-721082166 [Google Scholar] [CrossRef] [PubMed]
[13]. Jarit GJ, Kummer FJ, Gibber MJ, Egol KA, A mechanical evaluation of two fixation methods using cancellous screws for coronal fractures of the lateral condyle of the distal femur (OTA type 33B)J Orthop Trauma 2006 20(4):273-76.10.1097/00005131-200604000-0000716721243 [Google Scholar] [CrossRef] [PubMed]