Effect of Thyroid Peroxidase Antibody on Pregnancy Outcome among Hypothyroid Women
Shashikala Bhat1, AP Ashwini2, AP Suma3, Shashikiran Umakanth4
1 Professor, Department of Obstetrics and gynaecology, Dr. TMA Pai Hospital, Melaka Manipal Medical College, MAHE, Udupi, Karnataka, India.
2 Senior Resident, Department of Obstetrics and gynaecology, Dr. TMA Pai Hospital, Melaka Manipal Medical College, MAHE, Udupi, Karnataka, India.
3 Research Associate, Department of Statistics, Jain University, Bangalore, Karnataka, India.
4 Professor and Head, Department of Internal Medicine, Melaka Manipal Medical College, MAHE, Udupi, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. AP Ashwini, Senior Resident, Department of Obstetrics and gynaecology, Dr. TMA Pai Hospital, Court Road, Udupi, Karnataka-576101, India.
E-mail: ashwiniap11@gmail.com
Introduction
Thyroid disorders are among the most common endocrine disorders affecting pregnant women. About 2 to 3% of pregnant women are affected by subclinical hypothyroidism and about 0.3%-0.5% by overt hypothyroidism. Thyroid autoantibodies are found in 5-15% of women in childbearing age and have been associated with adverse pregnancy outcomes.
Aim
To compare the pregnancy outcomes in thyroid peroxidase antibody positive and thyroid peroxidase antibody negative hypothyroid women.
Materials and Methods
This was a retrospective study done in Dr TMA Pai Hospital, Udupi, Karnataka, India from January 2015 to December 2016. All singleton pregnant women with hypothyroidism were included and multiple pregnancy, pre-existing hypertensive or diabetic pregnancies were excluded. Serum Thyroid Stimulating Hormone (TSH) levels were estimated during booking visit for all pregnant women and if >2.5μIU/ml, free T3, T4, and Thyroid Peroxidase Antibody (TPO-Ab) levels were done. Data were retrieved from the hospital records and divided into TPO-Ab negative and TPO-Ab positive groups. The analysis was done using SAS v9.3. Chi-square test and Fisher-Exact test were used for testing equality of proportions. The p-value <0.05 was taken as significant.
Results
2385 antenatal women screened with TSH during the booking visit in study period, 169 (7.08%) were hypothyroid. 100 were TPO-Ab negative and 69 were TPO-Ab positive with 40.8% prevalence of TPO-Ab positivity among the hypothyroid pregnant women. The initial TSH and the average Levothyroxine requirement was 37% (p-value 0.206) and 16% (p-value 0.388) higher in the TPO-Ab positive group than in TPO-Ab negative group. Though the odds for having miscarriage was 2.36 (0.94,5.92), gestational hypertension was 2.71 (0.76, 9.69) and gestational diabetes was 2.88 (0.92,9.03) times higher in the TPO-Ab positive group as compared to TPO-Ab negative group, the p-value for miscarriage was 0.061, gestational hypertension was 0.125 and that for gestational diabetes was 0.062 and hence, statistically not significant. However, there was no difference in the preterm delivery rate in our study.
Conclusion
Presence of thyroid peroxidase antibodies may slightly increase the risk of miscarriage, gestational hypertension and gestational diabetes mellitus in pregnancy in the Indian population.
Autoimmune Hypothyroidism, Gestational diabetes mellitus, Gestational hypertension, Levothyroxine, Miscarriage
Introduction
Thyroid disorders are among the most common endocrine disorders affecting pregnant women. Pregnancy may modify the course of thyroid disorders, and pregnancy outcomes can depend on optimal management of thyroid disorders. About 2 to 3% of pregnant women are affected by subclinical hypothyroidism and about 0.3%-0.5% by overt hypothyroidism. Hypothyroidism in pregnancy is associated with increased risk of abortions, prematurity, low birth weight, intrauterine growth restriction, gestational hypertension, pre-eclampsia, abruptio placenta and stillbirth.
Thyroid autoantibodies are found in 5-15% of women of childbearing age [1]. Thyroid autoimmunity may be due to thyroid self-destruction by different mechanisms – activation of innate immunity involving DAMPs (Danger Associated Molecular Patterns by dying cells); hygiene hypothesis which proposes that there is higher chance of developing autoimmunity in those exposed to lesser load of infections during childhood [2]; fetal cells in maternal circulation by 4-5 weeks period of gestation resulting in fetal microchimerism which explains why there is postpartum exacerbation of autoimmune thyroiditis. Thyroid autoimmunity with the presence of antibodies against TPO-Ab and TG-Ab is associated with risk of hypothyroidism, miscarriage and preterm delivery during the antenatal period, thyroid dysfunction postnatally, and impairment in the motor and intellectual development in children [3]. The risk is associated especially with thyroid peroxidase antibody than with thyroglobulin antibody [4].
Possible mechanisms of thyroid autoimmunity and miscarriage include both a TSH dependent and TSH independent mechanism [5]. This could be an epiphenomenon resulting from an imbalance in the immune system in general and not specifically thyroid antibodies. Delay in conception itself due to autoimmunity leading to older age at conception, which could also contribute to miscarriage. Subtle deficiency in thyroxine requirement due to the compensatory failure of the gland may be another factor leading to pregnancy wastage [6]. This association has been found true even in euthyroid women [7].
Thyroid Peroxidase (TPO) gene, present on chromosome 2p25 is more TSH dependent than Thyroglobulin (TG) and codes for the membrane protein on thyrocyte surface and responsible for catalyzing the coupling of di-iodotyrosine and mono-iodotyrosine. TPO-Ab, seen more frequently than TG-Ab is present in higher titres and is mostly IgG subclass, also it is against the membrane-bound TPO enzyme which is not secreted and is hence more readily measurable than TG-Ab. A decrease in TPO autoantibodies occurs in pregnancy reaching a nadir in the third trimester; their rebound results in postpartum thyroid disease [8]. TPO positivity also significantly increases the chance of postpartum dysphoric symptoms regardless of the development of thyroiditis [9].
It is intriguing as to why hypothyroidism is prevalent in this coastal district, Udupi, in Karnataka where the majority of the population consumes seafood and therefore less prone to have iodine deficiency disorders. Till date, there is no study published from Southern coastal India regarding the prevalence of thyroid peroxidase antibodies in hypothyroid pregnant women and pregnancy outcomes. We, therefore, set out to compare pregnancy outcome in TPO-Ab positive and TPO-Ab negative hypothyroid women.
Materials and Methods
This was a retrospective record-based study done in the department of OBG, Dr TMA Pai Hospital, Udupi, Karnataka, India after obtaining the institutional ethical committee clearance (IEC341/2017). All singleton pregnant women with hypothyroidism who delivered between January 2015 to December 2016 were included in the study. Multiple pregnancy, pre-existing hypertensive or diabetic pregnancies were excluded.
As per the hospital protocol, serum TSH levels were estimated in the first trimester for all pregnant women. As per American Thyroid Association guidelines, if TSH was found to be >2.5μIU/ml, free T3, T4 and TPO-Ab levels were estimated, and the patient was treated with Levothyroxine [10]. TSH level was checked every 6 weeks, and the dose of Levothyroxine was adjusted to achieve trimester specific target TSH value. Data of these patients were retrieved from the hospital records for this study. The patients were divided into two groups; group 1-TPO Ab negative and group 2-TPO Ab positive.
Pregnancy outcomes in both the groups were compared. The variables studied were the miscarriage, gestational hypertension, pre-eclampsia, gestational diabetes mellitus, preterm delivery and low birth weight. The statistical analysis was performed using SAS 9.3 version. Chi-square test and Fisher-Exact test were used for testing equality of proportions. The p-value <0.05 was taken as significant.
Results
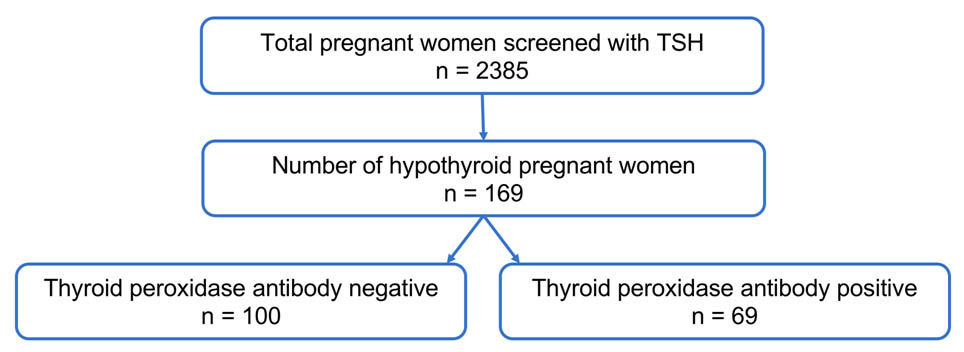
In the study period, 2385 antenatal women in the first trimester were screened with TSH during booking visit, as depicted in [Table/Fig-1]. Of them, 169 (7%) hypothyroid pregnant women were included in the study as per the TSH criteria defined by the ATA guidelines 2011; 100 were TPO-Ab negative, and 69 were TPO-Ab positive. The prevalence of TPO-Ab positivity was 40.8% among the hypothyroid pregnant women. During analysis of data, we found no statistically significant difference between the two groups concerning age and BMI as in [Table/Fig-2].
Patient grouping based on TPO antibodies.
Sample characteristics – Age, BMI and Parity in both groups.
| TPO-Ab negative(n=100) | TPO-Ab positive(n=69) |
|---|
| Prevalence | 59.2% | 40.8% |
| Age (years)- mean±SD | 28.15±3.75 | 28.18±4.03 |
| BMI- mean±SD | 23.47±4.14 | 22.96±4.7 |
| Primigravida | 57 (57%) | 40 (58%) |
| Multigravida | 43 (43%) | 29 (42%) |
The initial average TSH was 37% higher in TPO-Ab positive as compared to TPO-Ab negative group (p-value 0.206). The average Levothyroxine requirement was 16% higher in TPO-Ab positive group as compared to TPO-Ab negative group (p-value 0.388) as shown in [Table/Fig-3]. The cases with a past history of hypothyroidism (23 in the TPO-Ab negative group and 15 in TPO-Ab positive group) needed an increase in Levothyroxine dose during pregnancy. The TPO-Ab positive group needed 37.8% increase (66 to 91mcg) in dosage whereas in TPO-Ab negative group this increase was 22.7% (81.5 to 100mcg).
Average TSH and Levothyroxine dose in both groups.
| TPO-Ab negative(n=100) | TPO-Ab positive(n=69) |
|---|
| TSH (μIU/ml)- mean±SD | 4.58±2.28 | 6.31±3.99 |
| Levothyroxine dose (mcg)- mean±SD | 49.8±45.34 | 57.9±36.22 |
The rates of miscarriage, gestational hypertension and gestational diabetes mellitus were 9%, 4% and 5% in TPO-Ab negative group and 18.84%, 10.14% and 13.04% in the TPO-Ab positive cases; though these were higher in the TPO-Ab positive group, the difference was not statistically significant, as depicted in [Table/Fig-4]. No cases of pre-eclampsia were seen in both groups.
Adverse pregnancy outcomes in TPO Ab negative and TPO Ab positive groups.
| TPO-Ab negative(n=100) | TPO-Ab positive(n=69) | p-value |
|---|
| Miscarriage | 9 (9%) | 13 (18.84%) | 0.061 |
| Gestational hypertension | 4 (4%) | 7 (10.14%) | 0.125 |
| Gestational diabetes mellitus | 5 (5%) | 9 (13.04%) | 0.062 |
| Preterm delivery | 9 (9%) | 5 (7.2%) | 0.684 |
| Low birth weight | 8 (8%) | 6 (8.7%) | 0.871 |
Concerning mode of delivery, in TPO-Ab negative cases, 45% had a vaginal delivery, 48.4% had a Caesarean delivery, and 6.6% had instrumental delivery. Among TPO-Ab positive cases, 41% had a vaginal delivery, 57.1% had a Caesarean delivery, and 1.9% had instrumental delivery. The mean±SD for birth weight was 3.05±0.43kg in TPO-Ab negative and 3.06±0.50kg in TPO-Ab positive cases. There were no significant differences in the rates of preterm delivery, low birth weight, mode of delivery and average birth weight in both the groups.
On calculating the odds ratio, it was found the odds of having miscarriage was 2.36, gestational hypertension was 2.71, and gestational diabetes was 2.88 times higher in TPO-Ab positive group as compared to TPO-Ab negative group, as shown in [Table/Fig-5]. The p-value for miscarriage was 0.061, for gestational hypertension was 0.125 and that for gestational diabetes was 0.062, and was not statistically significant.
| Odds ratio | 95% Confidence interval |
|---|
| Miscarriage | 2.36 | (0.94-5.92) |
| Gestational hypertension | 2.71 | (0.76-9.69) |
| Gestational diabetes mellitus | 2.88 | (0.92-9.03) |
Discussion
The higher prevalence of 40.8% TPO-Ab positivity in present study may be because it was tested only in hypothyroid women and not in all pregnant women irrespective of TSH as in other Indian studies [11–15]. Bhattacharyya R et al., studied the influence of TPO-Ab on pregnancy outcomes and postpartum maternal dysfunction. They studied 400 pregnant women and found that 11.5% of them were positive for TPO-Ab with a TSH level of 2.31 IU/ml, which was significantly (p- 0.0001) higher than pregnant women negative for TPO-Ab (mean TSH 1.73 IU/ml). Increased incidence of miscarriage was seen in TPO-Ab positive mothers. This was seen in present study too. Postpartum thyroid dysfunction developed in 4.7%, of whom 81.25% were positive for TPO antibodies. They concluded that the presence of thyroid antibodies in early pregnancy, seems to predict pregnancy complications and maternal thyroid disease in the postpartum period [11].
Meena M et al., studied 1000 pregnant women and compared pregnancy outcomes between TPO-Ab positive and TPO-Ab negative pregnancies. They found that the prevalence of TPO-Ab positivity was 11% (n=110), 6.5% of them had elevated TSH. The prevalence of euthyroid women who were TPO-Ab positive was 4% (n=40). Anti-TPO positive, euthyroid females had a higher prevalence of infertility, anemia and preterm delivery as compared to the controls (p<0.0001). They found no difference between the two groups concerning abruption, recurrent abortions, intrauterine growth restriction, postpartum haemorrhage, symptomatic hypoth-yroidism, hypertensive disorders of pregnancy and fetal problems. They concluded that the results indicate that anti-TPO screening in pregnancy may aid in early identification of the women at risk [12].
Pradhan M et al., studied the prevalence of hypothyroidism and TPO-Ab positivity and found 7.9% hypothyroidism and 40% TPO-Ab positivity. In their study too, abortions, preterm delivery, fetal malformations, fetal growth restriction, poor Apgar scores and prolonged nursery admissions were higher [13].
Nambiar V et al., studied the prevalence and the effect of thyroid dysfunction on pregnancy outcomes in the Asian-Indian population. The study cohort comprised of 483 consecutive pregnant women attending the antenatal clinic during the first trimester. Serum TSH levels and anti-TPO antibody levels were estimated, and the patient treated accordingly. They reported that the prevalence of hypothyroidism (4.8%) and thyroid autoimmunity (12.4%) were high and both were significantly associated with abortion [14].
Kumru P et al., recruited 395 pregnant women to study the effect of thyroid dysfunction and autoimmunity on pregnancy and neonatal outcome. They found a 2.5 fold and 4.8 fold increase in preterm delivery in the isolated anti-TPO positivity and subclinical hypothyroidism with anti-TPO positivity groups respectively [15]. Meta-analysis showed that the combined RR of preterm delivery risk for pregnant women with positive TPO-Ab compared with the reference group was 1.69 (95% CI 1.19–2.41, P=0.003) [4]. Our study did not show an increase in preterm delivery in the Anti-TPO positive group, perhaps because of the beneficial effect of early initiation with Levothyroxine therapy.
Strength
This may be the largest Indian study with TSH screening of 2385 antenatal women in the first trimester and TPO-Ab status tested in hypothyroid pregnant women.
Limitation
In this study, TPO-Ab positivity was not assessed in euthyroid pregnant women with a normal range of initial TSH due to cost concerns. Selenium supplementation in the form of Selenomethionine 200 μg/d during pregnancy and the postpartum period known to reduce hypothyroidism [16] or Glucocorticoid therapy was not given to TPO-Ab positive women. Postpartum thyroid status was only followed up with TSH levels and dose adjusted based on non-pregnant criteria; a repeat TPO-Ab titer was not done. This study was done following the ATA 2011 guidelines.
Conclusion
Presence of thyroid peroxidase antibodies may slightly increase the risk of miscarriage, gestational hypertension, and gestational diabetes mellitus during pregnancy in Indian population. Larger multicentric Indian studies are needed to explore the definite association between thyroid peroxidase antibody positivity and adverse pregnancy outcome and postpartum thyroid dysfunction.
[1]. De Groot L, Abalovich M, Alexander EK, Amino N, Barbour L, Cobin RH, Management of thyroid dysfunction during pregnancy and postpartum: an Endocrine Society clinical practice guidelineJ Clin Endocrinol Metab [Internet] 2012 97(8):2543-65.10.1210/jc.2011-280322869843 [Google Scholar] [CrossRef] [PubMed]
[2]. Cogni G, Chiovato L, An overview of the pathogenesis of thyroid autoimmunityHormones (Athens) [Internet] 2013 12(1):19-29.0.1007/BF0340128323624128 [Google Scholar] [CrossRef] [PubMed]
[3]. Mehran L, Tohidi M, Sarvghadi F, Delshad H, Amouzegar A, Soldin OP, Management of thyroid peroxidase antibody euthyroid women in pregnancy: comparison of the American thyroid association and the endocrine society guidelinesJ Thyroid Res [Internet] 2013 2013:542-692.10.1155/2013/54269223738229 [Google Scholar] [CrossRef] [PubMed]
[4]. He X, Wang P, Wang Z, He X, Xu D, Wang B, Thyroid antibodies and risk of preterm delivery: a meta-analysis of prospective cohort studiesEur J Endocrinol [Internet] 2012 167(4):455-64.10.1530/EJE-12-037922826476 [Google Scholar] [CrossRef] [PubMed]
[5]. Twig G, Shina A, Amital H, Shoenfeld Y, Pathogenesis of infertility and recurrent pregnancy loss in thyroid autoimmunityJ Autoimmun [Internet] 2012 38(2–3):J275-81.10.1016/j.jaut.2011.11.01422218218 [Google Scholar] [CrossRef] [PubMed]
[6]. Kaprara A, Krassas GE, Thyroid autoimmunity and miscarriageHormones (Athens) [Internet] 2008 7(4):294-302.10.14310/horm.2002.121019121990 [Google Scholar] [CrossRef] [PubMed]
[7]. Chen L, Hu R, Thyroid autoimmunity and miscarriage: a meta-analysisClin Endocrinol (Oxf) [Internet] 2011 74(4):513-19.10.1111/j.1365-2265.2010.03974.x21198746 [Google Scholar] [CrossRef] [PubMed]
[8]. Balucan FS, Morshed SA, Davies TF, Thyroid autoantibodies in pregnancy: their role, regulation and clinical relevanceJ Thyroid Res [Internet] 2013 2013:182-472.10.1155/2013/18247223691429 [Google Scholar] [CrossRef] [PubMed]
[9]. Groer MW, Vaughan JH, Positive thyroid peroxidase antibody titer is associated with dysphoric moods during pregnancy and postpartumJ Obstet Gynecol Neonatal Nurs JOGNN [Internet] 2013 42(1):E26-32.10.1111/j.1552-6909.2012.01425.x23167615 [Google Scholar] [CrossRef] [PubMed]
[10]. Stagnaro-Green A, Abalovich M, Alexander E, Azizi F, Mestman J, Negro R, Guidelines of the American Thyroid Association for the diagnosis and management of thyroid disease during pregnancy and postpartumThyroid [Internet] 2011 21(10):1081-125.10.1089/thy.2011.008721787128 [Google Scholar] [CrossRef] [PubMed]
[11]. Bhattacharyya R, Mukherjee K, Das A, Biswas MR, Basunia SR, Mukherjee A, Anti-thyroid peroxidase antibody positivity during early pregnancy is associated with pregnancy complications and maternal morbidity in later lifeJ Nat Sci Biol Med [Internet] 2015 6(2):402-05.10.4103/0976-9668.16002126283839 [Google Scholar] [CrossRef] [PubMed]
[12]. Meena M, Chopra S, Jain V, Aggarwal N, The effect of anti-thyroid peroxidase antibodies on pregnancy outcomes in euthyroid womenJ Clin Diagn Res [Internet] 2016 10(9):QC04-QC07.10.7860/JCDR/2016/19009.840327790523 [Google Scholar] [CrossRef] [PubMed]
[13]. Pradhan M, Anand B, Singh N, Mehrotra M, Thyroid peroxidase antibody in hypothyroidism: it’s effect on pregnancyJ Matern Fetal Neonatal Med [Internet] 2013 26(6):581-83.10.3109/14767058.2012.74549823211129 [Google Scholar] [CrossRef] [PubMed]
[14]. Nambiar V, Jagtap VS, Sarathi V, Lila AR, Kamalanathan S, Bandgar TR, Prevalence and impact of thyroid disorders on maternal outcome in Asian-Indian pregnant womenJ Thyroid Res [Internet] 2011 2011:429-497.10.4061/2011/42909721789274 [Google Scholar] [CrossRef] [PubMed]
[15]. Kumru P, Erdogdu E, Arisoy R, Demirci O, Ozkoral A, Ardic C, Effect of thyroid dysfunction and autoimmunity on pregnancy outcomes in low risk populationArch Gynecol Obstet [Internet] 2015 291(5):1047-54.10.1007/s00404-014-3533-925388918 [Google Scholar] [CrossRef] [PubMed]
[16]. Negro R, Greco G, Mangieri T, Pezzarossa A, Dazzi D, Hassan H, The influence of selenium supplementation on postpartum thyroid status in pregnant women with thyroid peroxidase autoantibodiesJ Clin Endocrinol Metab 2007 92(4):1263-68.10.1210/jc.2006-182117284630 [Google Scholar] [CrossRef] [PubMed]