Case Report
A 35-year-old systemically healthy non-smoker male patient was referred to the Department of Periodontics for management of broken front teeth. He gave history of trauma due to fall injury one year back. Clinical examination revealed oblique fracture of right and left central incisors (#11, #21) with fracture line extending subgingivally on the palatal aspect and the coronal fragment was mobile [Table/Fig-1].
The clinical photograph before the surgical removal of teeth which shows oblique fracture in central incisors involving incisal edge and hence two incisal edges are seen.

The plaque index score indicated good oral hygiene, but bleeding on probing was present in the palatal gingiva of #11 and #21 due to inflammation between the broken segments of tooth. He had low smile line, thick gingival biotype, and the Jemt Papilla index (1997) score was 3 between the central incisors as gingival papilla filled the entire interdental space [1].
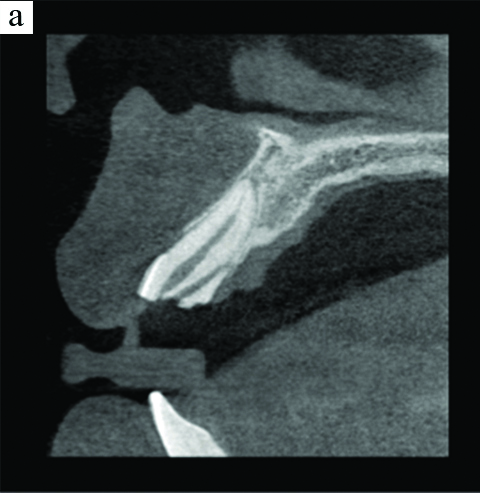
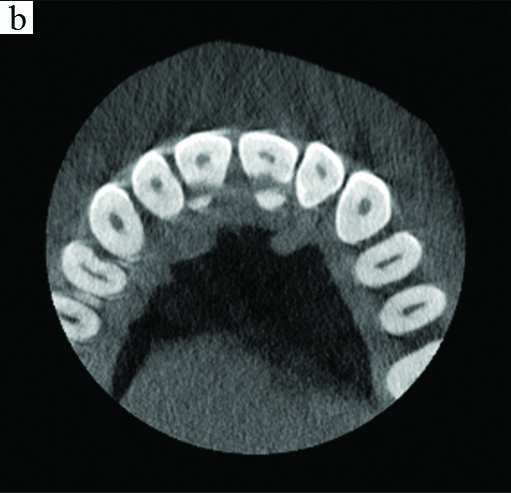
Since this was the fracture involving the incisal edges and oblique fracture, to determine the exact extent of fracture line, Cone Beam Computed Tomography (CBCT) was performed [2]. CBCT imaging revealed oblique fracture line in 11 and 21 extending from incisal edge to palatally up to middle 3rd of the root surface and hence two incisal edges were seen. Also there was thin labial cortical bone covering the root surface which makes placement of immediate implant complicated [Table/Fig-2a,b].
Cone Beam Computed Tomography (CBCT) sagittal view. Thin labial bone plate covering the incisor and the extent of the oblique fracture extending from the incisal edge to the middle third of the root palatally.
CBCT axial view. The two central incisors having fractured segments separated by soft tissue is seen.
Various interdisciplinary treatment options including endodontic management to save the tooth and prosthetic replacement if tooth is extracted were discussed [3]. The aesthetics, time duration of treatment and predictability of results were the concern of the patient.
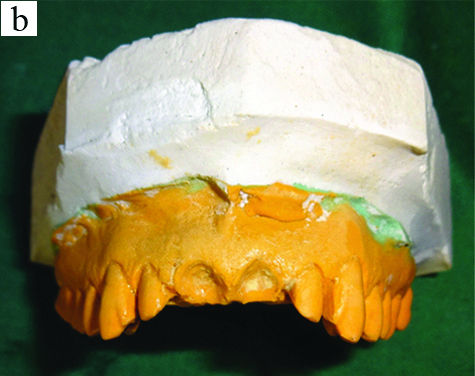
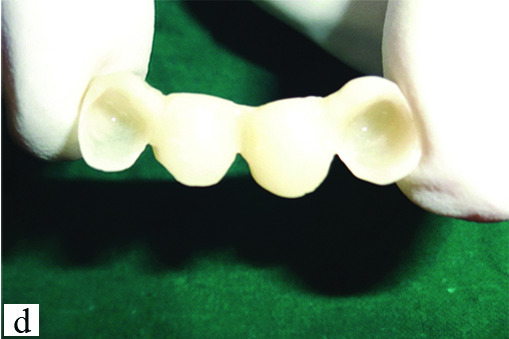
Hence, the designed treatment plan included phase 1 therapy initially to restore the gingival health followed by atraumatic extraction of #11 and #21, preservation of extracted socket with autologous Platelet Rich Fibrin (PRF) and alloplast β-Tricalcium Phosphate (β-TCP) and immediate replacement of teeth with fixed prosthesis. The abutment teeth were prepared and temporary prosthesis was fabricated prior to the surgical procedure from the model [Table/Fig-3a,b,c and d].
Prosthesis lab fabrication. Model prepared from impression of the tooth prior to surgical procedure.

Prosthesis lab fabrication. The tooth to be extracted was knocked out from the model prior to surgical procedure.
Prosthesis lab fabrication. Temporary prosthesis fabricated buccal view.

Temporary Prosthesis lab fabrication.
Surgical Procedure
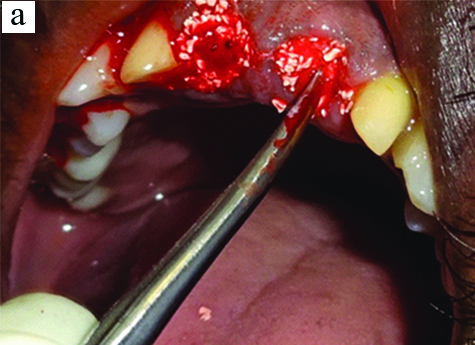
Informed consent was taken before the surgical procedure. Under aseptic conditions #11, #21 region was anesthetised using 2% lignocaine hydrochloride. Atraumatic extraction of fractured #11, #21 was performed with periotome [Table/Fig-4] and the fragments of teeth were removed from socket [Table/Fig-5]. The socket was carefully curetted for any residual pathologic tissue and copiously irrigated with normal saline.
After atraumatic flapless extraction of teeth using periotome, the intact extraction socket of 11.

Fragments of teeth extracted.

To prepare the PRF, peripheral venous blood was collected from the antecubital vein of the patient under sterile conditions and dispensed into a sterile 10 mL glass tube. The procedure was carried out as per the protocol developed by Choukroun J et al., with no anticoagulants. The blood sample was immediately centrifuged for 10 minutes at 3000 rpm leading to the initiation of the coagulation cascade [4].
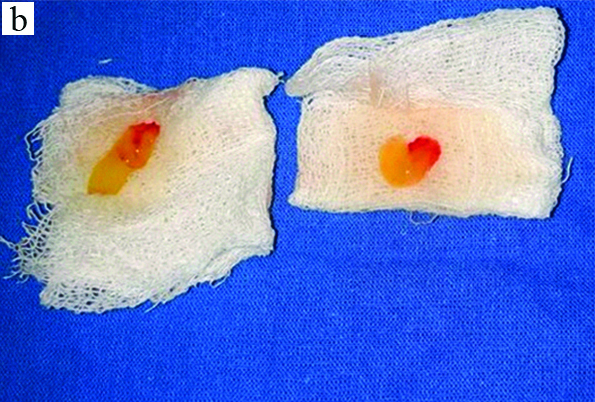
After centrifugation, the blood separated into three layers: acellular platelet poor plasma on top, a PRF clot in the middle and RBC’s at the bottom of the test tube [Table/Fig-6a]. The PRF clot was removed from the tube; the attached RBC’s were scraped off and discarded. PRF clot was squeezed in wet gauze and PRF membrane was obtained [Table/Fig-6b].
Platelet Rich Fibrin (PRF) formed in the test tubes after centrifugation of the blood.
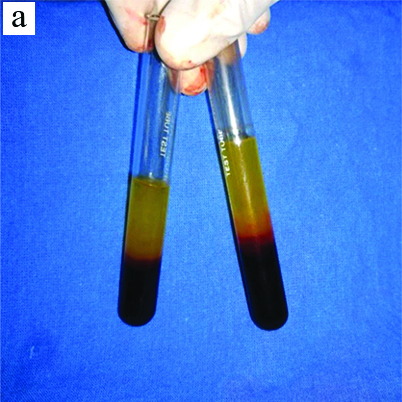
PRF placed over sterile wet gauze.
The prepared autologous PRF was mixed with β-TCP (SYBOGRAFTTM-PLUS-Eucare Pharmaceuticals Pvt. Ltd.,) and placed in the socket [Table/Fig-7a] and PRF membrane was used for socket closure [Table/Fig-7b]. The fibrin glue like property of PRF helps in adhesion of wound margins without use of suturing and hence minimal trauma to the tissues. Teeth were then replaced immediately by temporary pontic prosthesis with the gingival margin of the pontic extending 1 mm subgingivally [Table/Fig-8a,b].
Mixture of PRF and alloplast placed inside the extraction socket for socket preservation.
After socket preservation of the two central incisors extraction socket, PRF membrane was used to cover the wound.

Photograph after the cementation of the temporary fixed prosthesis immediately after socket preservation-Labial view.

Photograph after the cementation of the temporary fixed prosthesis immediately after socket preservation-Palatal view.

Fabrication of Pontic
The ovate pontic can be fabricated either by direct method or indirect method. In this case for indirect technique, the abutment teeth were prepared and an impression was made prior to extraction of teeth and poured with fast setting stone [Table/Fig-3a]. On the model, the tooth to be extracted was knocked down to create the appearance of an edentulous region [Table/Fig-3b]. Then the model was carved with an acrylic bur to simulate the profile and depth of the ideal pontic. Then the provisional restoration was processed using the heat cured acrylic [Table/Fig-3c,d] and positioned.
Post-Op Instruction
Patient was prescribed Amoxicillin 500 mg Tid and Paracetamol 500 mg Tid for three days and was advised to follow the oral hygiene measures meticulously.
Post-Surgical Follow Up
The healing was uneventful and post-operative follow up was done in 1 week, 1 month and 6 months. Post treatment Jemt interdental papilla score was 3 at 1 month [Table/Fig-9a,b]. But unfortunately the patient met with a fall injury at six months and lost his prosthesis for one week before replacement by permanent prosthesis. Hence, papilla score reduced to 2 [Table/Fig-10a] and there was bluntness of the tip and reduction of height of the papilla about 1 mm at the end of 6 months [Table/Fig-10b]. Follow-up radiograph showed that healing of socket bone was good after the socket preservation procedure.
Photograph one month after the extraction and immediate prosthesis replacement. Jemt interdental papilla score was 3 at 1 month.

Note the excellent healing of the soft tissue and aesthetics due to presence to sharp tip of the interdental papilla between two central incisors.

Photograph six months after the extraction and immediate prosthesis replacement. Jemt interdental papilla score was 2.

The healing of the soft tissue is excellent and but there is blunting of tip of the interdental papilla between two central incisors as the patient was without prosthesis for few days.

Discussion
In recent years, aesthetic demand in dentistry has experienced fruition, driven by an enhanced consciousness of beauty. Pink aesthetics refers to the soft tissues of the oral cavity including the interdental papilla. Absence of papilla, present as black triangles in the interdental region is accompanied by both aesthetic and functional hitches [5]. White aesthetics is the natural teeth or the restored dentition. The definitive aim of reinstating an aesthetically imperative zone is to accomplish pink and white aesthetics and it requires a well-balanced interdisciplinary approach [6].
This patient had good oral hygiene, low smile line, thick gingival biotype which favoured easy aesthetic management. The fracture line extended beyond the gingival margin and hence biological width preservation should be taken care to prevent future gingival inflammation and gingival recession. To preserve the tooth, treatment options were endodontic treatment followed by raising mucoperiosteal flap and surgical ostectomy, orthodontic extrusion or post preparation and reattachment of fragments [7,8].
Extraction of tooth followed by prosthetic replacement was also suggested. Due to thin labial plate and labially curved roots in the tooth as revealed by CBCT immediate implant treatment was complicated and needed either socket shield technique or guided bone regeneration. Also, socket preservation and delayed implant placement needed two surgical treatments. Moreover, there is more chance for loss of interdental papilla between the two implants if they are not widely placed.
Adhesive, resin-bonded cantilever bridge with natural tooth pontic treatment is commonly used nowadays to restore the aesthetics and function [9]. But, it was not done in this case due to oblique fracture of tooth splitting the incisal edge. And frequent re-attachment may be needed for resin bonded cantilever bridges. Hence conventional fixed partial denture replacement was decided.
According to Van der Velden U, the factors which influence the existence of interdental papilla are the presence of adjacent teeth contact, the size of the gingival embrasure and the level of interproximal bone [10]. Tarnow DP et al., in his classical study in 1992, found that the interdental space was filled with tissues in 100% of cases, when the distance between the contact point of the teeth and the interproximal bone crest is less than or equal to 5 mm [11].
Socket preservation is a procedure to reduce bone loss after tooth extraction to preserve the dental alveolus in the alveolar bone. This procedure was first described in 1985 [12]. Various biomaterials including autograft, allograft, alloplast and xenograft along with resorbable or non-resorbable membrane are used.
In this case PRF, a second generation platelet concentrate, was used for socket preservation to maintain the soft tissue and bone level, and Immediate Pontic Technique to maintain the adjacent teeth contact and gingival embrasure.
PRF was first developed by Choukroun J et al., in France [4]. It is a viable and biocompatible autologous biologic material with growth factors and cytokines. PRF also has the advantage of easiness to procure, display adhesive properties and enhances angiogenesis. The release of growth factors like PDGF, TGF β, ILGF, EGF which occurs for a minimum of 7 days is very favourable for regeneration [13,14].
Along with PRF, β-TCP was used in this case where the function of β-TCP is to stabilise the coagulum within the socket and avoid possible reduction of hard tissue volume required for bone regeneration. Further, it provides a scaffold for the growth of cellular and vascular tissues in the process of new bone formation [15].
The proper support for the gingival tissues by a well-designed pontic is equally important. In 1999, Spear suggested “Immediate Pontic Technique” to maintain the interdental papilla with ovate pontic following anterior teeth removal [16]. With the sustenance of PRF, we have extended the gingival margin only by 1 mm instead of 2.5 mm beyond gingival margin. The pontic should stretch in a straight line from the cervical third of the tooth on the labial surface and should not be rolled palatally under the free gingival margin so as to obviate the loss of support to the gingival margin.
Treatment modality like immediate implant is highly technique sensitive and in this case it may necessitate either socket preservation or guided bone regeneration. Two stage implant placement takes time and may result in loss of papilla if not ideally placed. Adhesive bonded prosthesis may require frequent reattachment. Natural pontic replacement is not possible in split tooth.
In this case with two fractured central incisors, the diagnosis of extent of fracture line using CBCT, usage of atraumatic flapless technique for extraction of tooth, use of autologous PRF aided healing, socket preservation, adhesion of wound margin without suture by acting like fibrin glue and use of immediate ovate pontic has resulted in maintaining pink and white aesthetics.
Conclusion
Interdental papilla plays a vivacious role in determining the aesthetics. Retaining interdental papilla after tooth extraction is always a defying task, when related to restoration of multiple anterior teeth. Albeit there are vivid ways for preserving pink and white aesthetics, the technique which we have described here with the use of atraumatic extraction, socket preservation using PRF and Immediate Pontic Technique is simple, cost effective, provides tangible benefits and is not technique sensitive.
Declaration of Patient Consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
[1]. Jemt T, Regeneration of gingival papilla after single-implant treatmentInt J Periodontics Restorative Dent 1997 17:326-33. [Google Scholar]
[2]. Cohence N, Silberman A, Contemporary imaging for the diagnosis and treatment of traumatic dental injuries: a reviewDental traumatology 2017 33:321-28.10.1111/edt.1233928317333 [Google Scholar] [CrossRef] [PubMed]
[3]. Malhotra N, Kundalala Acharaya S, A review of root fractures: diagnosis, treatment and prognosisDent update 2011 38:615-28.10.12968/denu.2011.38.9.61522238994 [Google Scholar] [CrossRef] [PubMed]
[4]. Choukroun J, Adda F, Schoeffler C, Vervelle A, An opportunity in paro-implantology: PRFImplantodontie 2001 42(55):e62[translated from: French] [Google Scholar]
[5]. Zeter L, Wang HL, Management of interdental papillaJ Periodontal 2005 32:831-39. [Google Scholar]
[6]. Cochman C, Calamita M, The reconstruction of pink and white aestheticsInt Dent SA 2010 12:88-93. [Google Scholar]
[7]. Narayanan Kutty SK, Mohamed SC, Janam P, Gopinath AS, Interdisciplinary approach for the management of complicated crown-root fracture of anterior teeth-a case reportIJSS Case reports & Reviews 2017 3:05-09. [Google Scholar]
[8]. Raju IR, Sreedev CP, Mathew S, Deepa NT, Karthick K, Boopathi T, Biological rehabilitation of complex oblique crown-root fracture segment reattachmentJ Pharm Bioall Sci 2017 9:S292-94.10.4103/jpbs.JPBS_152_1729284983 [Google Scholar] [CrossRef] [PubMed]
[9]. Aspalli S, Sanikop MV, Nagappa G, Desai A, Gaddale R, Esthetic provisional replacement of a hopeless anterior tooth by natural pontic: A case seriesJ Adv Clin Res Insights 2017 4:21-23.10.15713/ins.jcri.150 [Google Scholar] [CrossRef]
[10]. Van der Velden U, Regeneration of the interdental soft tissues following denudation proceduresJ Clin Periodontol 1982 9:455-59.10.1111/j.1600-051X.1982.tb02106.x6960021 [Google Scholar] [CrossRef] [PubMed]
[11]. Tarnow DP, Magner AW, Fletcher P, The effect of the distance from the contact point to the crest of bone on the presence or absence of the interproximal papillaJ Periodontol 1992 63:995-98.10.1902/jop.1992.63.12.9951474471 [Google Scholar] [CrossRef] [PubMed]
[12]. Cohen ES, Atlas of cosmetic and reconstructive periodontal surgery 2007 3rd editionItalyBC Decker Inc:347 [Google Scholar]
[13]. Sharma A, Pradeep AR, Treatment of 3 wall intrabony defects in patients with chronic periodontitis with autologous platelet rich fibrin: a randomized clinical trialPeriodontol 2011 82:1705-12.10.1902/jop.2011.11007521513477 [Google Scholar] [CrossRef] [PubMed]
[14]. Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, Platelet-Rich Fibrin (PRF): A second-generation platelet concentrate. Part II: Platelet-related biologic featuresOral Surg Oral Med Oral Pathol Oral Radiol Endod 2006 101:e45-50.10.1016/j.tripleo.2005.07.00916504850 [Google Scholar] [CrossRef] [PubMed]
[15]. Muñoz-Corcuera M, Bascones-Martínez A, Ripollés-de Ramón J, Post-extraction application of beta tricalcium phosphate in alveolar socketJ Osseointegration 2015 7:8-14. [Google Scholar]
[16]. Spear FM, Maintenance of the interdental papilla following anterior tooth removalPract Periodontics Aesthet Dent 1999 11:21-28. [Google Scholar]