Ruptured and Inflamed Epidermal Inclusion Cyst of Tongue- A Case Report
Nishant Sagar1, Prerna Arora2, Nita Khurana3, JC Passey4
1 Senior Resident, Department of Pathology, Maulana Azad Medical College, Delhi, India.
2 Assistant Professor, Department of Pathology, Maulana Azad Medical College, Delhi, India.
3 Head of Department, Department of Pathology, Maulana Azad Medical College, Delhi, India.
4 Director Professor, Department of ENT, Maulana Azad Medical College, Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Nishant Sagar, 606 Royal Park, Ramprastha Greens, Sector-9, Vaishali, Ghaziabad-201012, Uttar Pradesh, India.
E-mail: saganishant@gmail.com
Epidermal inclusion cyst (EIC) is rare in head and neck region with incidence in oral cavity being less than 0.01%, presenting as congenital or as acquired lesions. Clinically patient presents with dysphagia, difficulty in breathing and may be associated with various syndromes like Gardner syndrome, basal cell nevus syndrome and pachyonychia congenita. Pathogenesis of EIC includes implantation of ectodermal component along the embryological site of fusion or due to trauma. A case of EIC of tongue in a three year old male child is presented here along with review of literature.
Acquired cysts, Epidermoid cyst, Intraoral cysts
Case Report
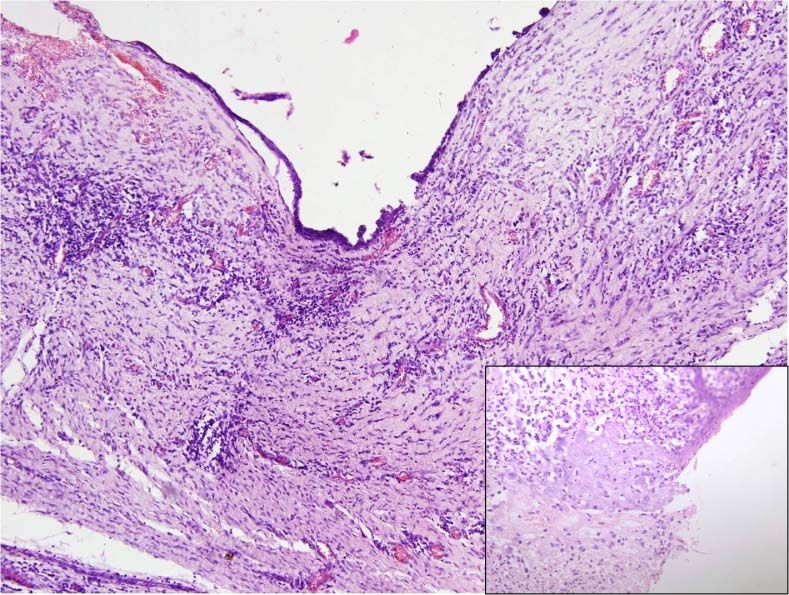
A three-year-old male child presented at the ENT Department of Lok Nayak Hospital, Delhi with a history of diffuse swelling in the tongue since two months. The swelling was progressively enlarging, slightly tender, causing difficulty in mastication. Apart from these no other symptoms were present. The swelling was present over the dorsal aspect involving the anterior half of the tongue measuring approximately 2x2 cm [Table/Fig-1]. No past history of trauma or significant dental complaints was present. On examination, the swelling was cystic and soft in consistency. Magnetic resonance imaging was performed, which revealed a well defined cystic lesion with internal septae and peripheral enhancement in tongue and lower lip [Table/Fig-2]. Differential diagnosis of epidermoid cyst and lymphangioma were considered. The swelling was excised and sent to histopathology department. Grossly, a cyst measuring 2.5cm in diameter was identified with wall thickness of 0.2cm. Microscopic examination showed a cyst lined by stratified squamous epithelium, with keratinous flakes and large areas of surface ulceration; ulcer bed was formed by acute and chronic inflammatory granulation tissue comprised of neutrophils, lymphocytes and occasional plasma cells. No mitosis, necrosis or atypia was present [Table/Fig-3]. No evidence of malignancy was seen. No hair shaft or other dermal appendages were identified. A confirmatory diagnosis of ruptured and inflamed EIC tongue was given.
Cystic swelling involving the anterior part of tongue.

Well defined cystic lesion with internal septae.

Cyst lined by stratified squamous epithelium with keratinous flakes (100X).
Discussion
Epidermal Inclusion Cyst (EIC), also known as epidermoid cyst is commonly seen in face, neck and trunk [1]. Epidermoid cysts were first described by Roser in 1859, and are lined by epidermis with granular layer and filled with keratinous debris [2]. Dermoid cysts are similar histologically and contain dermal appendages within the lining. EIC are rare in oral cavity, and further rarer in tongue. EIC can present as congenital lesion or acquired later in life [3]. Patient in the present case was a three-year-old child, with short duration of swelling.
The pathogenesis of congenital lesion is failure of separation of ectodermal component from underlying neural tube, or due to implantation of ectodermal component along the embryological site of fusion during 3rd and 5th weeks of gestation. Acquired EIC occur due to implantation of epidermis in dermal tissue either post trauma, or iatrogenic [3]. However, clinically and histologically they are not different. In the present case no history of trauma was present.
EIC is seen most commonly in 15 to 35 year old, with strong predilection for males [4]. They may be associated with various syndromes like Gardner syndrome, basal cell nevus syndrome and pachyonychia congenita. Our patient had no signs or symptoms associated with any of the above syndromes. The patient may remain asymptomatic with a mere cystic swelling, or symptoms like dysphagia, difficulty in breathing or speech may be seen [5]. Our patient had painless swelling with difficulty in eating. EIC needs to be differentiated from common lesions such as lymphangioma, ranula, duplication cyst, mucocele, lymphoepithelial cyst and thyroglossal duct cyst involving the tongue [6]. Rare cases of squamous cell carcinoma, basal cell carcinoma, bowens disease and mycosis fungoides developing in EIC have been reported [7]. Literature search reveals that 0.011 to 0.045% EIC cases may undergo malignant changes, with majority being reported in skin involving head, neck or limb, with large variability in size, mean being 5cm [8]. However, presence of malignancy in EIC tongue has not been previously described.
Asymptomatic EIC may be left untreated, while local inflammation may be controlled by injection of steroids. Complete excision may be required for symptomatic cases. Recurrence is rare following excision. Very large cysts may be treated with marsuplisation [5]. Our patient is on follow up, with no signs of recurrence.
Conclusion
The present case highlights the occurrence of EIC at a rare site which is tongue. Syndromes associated with the lesions should be ruled out by proper clinical examination. Although rare, careful microscopic examination is essential to look for coexisting malignant changes.
[1]. Kini YK, Kharkar VR, Rudagi BM, Kalburge JV, An unusual occurrence of epidermoid cyst in the buccal mucosa: A case report with review of literatureJ Maxillofac Oral Surg 2013 12:90-93.10.1007/s12663-011-0188-y24431820 [Google Scholar] [CrossRef] [PubMed]
[2]. Shivakumar MS, Yogesh TL, Nagaraj T, Sinha P, Epidermal inclusion cyst of buccal mucosa: A rare case reportInt J Med Dent Case Rep 2015 :1-3. [Google Scholar]
[3]. Abhishek V, Arpit S, Jyoti D, Abhijit R, An unusual case of epidermal inclusion cyst of maxillaInt J Head Neck Surg 2010 1:43-47.10.5005/jp-journals-10001-1009 [Google Scholar] [CrossRef]
[4]. Retnakumar K, Packiaraj I, Gen Morgan K, Alaguvel Rajan M, Abdul Rahman SM, Unusual case of epidermoid cyst - A case reportUnique J Med Dent Sci 2014 2:80-81. [Google Scholar]
[5]. Lakshmi S, Somashekara KG, Priya NS, Epidermoid cyst of tongueOtorhinolaryngol Clin 2011 3(2):122-24.10.5005/jp-journals-10003-1069 [Google Scholar] [CrossRef]
[6]. Walstad WR, Solomon JM, Schow SR OM, Midline cystic lesion of the floor of the mouthJ Oral Maxillofac Surg 1998 56:70-74.10.1016/S0278-2391(98)90919-3 [Google Scholar] [CrossRef]
[7]. López-Ríos F, Rodríguez-Peralto JL, Castaño E, Benito A, Squamous cell carcinoma arising in a cutaneous epidermal cyst: case report and literature reviewAm J Dermatopathol 1999 21:174-77.10.1097/00000372-199904000-0001210218680 [Google Scholar] [CrossRef] [PubMed]
[8]. Ziadi S, Trimeche M, Hammedi F, Squamous cell carcinoma arising from an epidermal inclusion cyst: A case reportNorth American Journal of Medical Sciences 2010 2(1):46-47. [Google Scholar]