HNC are malignant tumours which arise above the clavicle within the structures located in the aero-digestive tract of the face and neck including glands, organs, soft tissues and bony structures of head and neck [1]. Head and neck area is placed colossal significance by individuals comparing other part of the body as it reflects our internalised sense of personality [2]. Every treatment options for head and neck cancer such as surgery, radiation therapy, chemotherapy or combination of these can change the structure and function of head and neck and leads to dysfunction and disfigurement. The obvious visibility of signs and symptoms among many HNC patients results in coping problems, inability to adapt to changes and curtails the quality of life [1,2].
Self-image can be described as the way one thinks about self and their abilities or appearance. In other words it’s one’s conception of oneself or of one’s role [3]. Portraying themselves is an innate enthusiasm of human beings. Self-concept possesses convincing impact on one’s life [4]. The belief of “self” is imperative human need and is of major interest [5]. Self-concept is multifaceted [6], unique to individual and changes overtime with context [4]. Development of positive or negative self-concept mainly results from physical, appearance and performance changes, health challenges and from feedback from significant others. Loss of a body part or alteration in health status can also affect the self-concept [4].
Treatment modalities and HNC have effect on functional changes and facial disfigurement. Such in-capabilities directly influence the client’s self-concept [7]. Findings of a study conducted by same authors also show that, suffering from HNC has effect on different domains of self-image such as body image, self-esteem and integrity [8].
Adverse side effects of radiation therapy include dryness of skin, skin reactions, redness or rash which is evidently visible to others. The functional disturbances leads to dysphagia, changes in the consistency of saliva, mucositis, disturbances in the speech and suppression of cell-mediated and humoral immunity [1]. HNC affects the basic functioning of many patients and it is very difficult to conceal the signs and symptoms for many of them. This in term leads to psychological disintegration and varying degrees of facial disfigurement. Thus changes in performance, physical changes associated with HNC affects the self-concept enormously.
HNC patients with disturbed body image have significant association with depressive symptoms at the end of the treatment [9]. However, very little is known about the relationship between self-concept and quality of life of patients with HNC. Hence, researcher carried out a mixed method research on the functional assessment, self-image and lived experiences of head and neck cancer patients. Present study adopted a concurrent triangulation strategy of mixed method design, as the aim of the study was to determine the functional assessment and self-image of HNC patients and to acquire a deeper understanding of lived experiences. This model was selected to confirm and corroborate findings on self-image, functional assessment and lived experiences of patients with HNC in a single study. Both quantitative and qualitative data were collected concurrently by paying equal weight to both methods (QUAN+QUAL). Part of study findings conducted on same set are disseminated [8]. Analysis of factors associated with self-image and quality of life among head and neck cancer patients is presented in this paper.
Materials and Methods
Setting and Subjects: A mixed method research on the functional assessment, self-image and lived experiences of head and neck cancer was conducted between February 2015 and May 2015, at two tertiary care hospitals of Karnataka representing the sample of South India. The findings presented in this paper are part of the study on self-image and quality of life of head and neck cancer patients [8]. In this study, sample included 54 patients with HNC. Sample size was calculated based on the correlation value of self-image and quality of life from pilot study (r=0.37). Subjects were selected from two oncological centers of tertiary care hospitals; Karnataka. Subjects were hospitalized patients who were in the fourth week of radiation therapy and were able to read and write Kannada and English. Subjects previously diagnosed with mental illness, which was identified through the health records were excluded from the study. Following formula was used for sample size calculation.
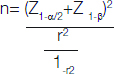
Where:
Z1-α/2= value at specified confidence level of 95% (1.96)
Z1-β=required power 0.84 (80%)
r=0.37, correlation value of self-image and quality of life from pilot study
n=required sample size =49
Final sample size was estimated to be 54 including 10% non-response rate.
The present study was approved by the Institutional Ethics Committee and Institutional Research Committee. The data were collected between 7th February 2015 and 10th May 2015 after obtaining informed written consent from all participants. Data was collected through self-administered demographic and disease related variable tool, self-image scale and FACT; H&N. Self-image scale was a four point Likert scale with 18 declarative items developed by the researcher after extensive literature review [10-12]. The highest possible score was 72 and minimum score was 18. The total score was arbitrarily classified 18-45 as negative self-image and 46-72 as positive self-image. The findings on self-image of a patient with head and neck cancer have already been published [8]. The Functional Assessment of Cancer Therapy –Head and Neck questionnaire is a standardised scale [13] of 39 items and prior permission was obtained from facit.org. The items of the scale were grouped into two subscales: General scale with 27 items and HNC specific scale12 items. Each item is rated from 0 to 4 and is a declarative statement. Since it is a standardised tool, necessary permission was obtained from FACIT.org. Reverse scoring was required for some of the items in both tools. The minimum and maximum possible score was 0-148 and according to the scoring guidelines, higher the score better the quality of life. All statistical analysis applied in this study includes frequency, percentage, Chi-square, Kruskal Wallis and Spearman rho with assistance of SPSS 16.0 software. A p-value was considered significant if it was <0.05.
Results
Sample characteristics: Among HNC patients, majority i.e., 36 out of 54 (66.7 %) were above 50 years, 43 (79.6%) were men, 47 (87%) were married and living with spouse, 47 (87%) had education till primary level, 25 (46.3%) had family income less than Rs. 5000/- per month. Regarding personal habits, 26 (48.15%) had a habit of smoking, 35 (64.81%) of them were chewing tobacco and 16 (29.63%) were consuming alcohol [Table/Fig-1].
Association between self-image and demographic variables.
| Variable | Negative self-image(Score between 18-45) | Positive self-image(score between 46-72) | df | Chi-square (χ2) | p-value |
|---|
| Age in years |
| <50 years | 7 | 11 | 1 | 0.337 | 0.561 |
| >50 years | 17 | 19 |
| Gender |
| Male | 20 | 23 | 1 | 0.006 | 0.940 |
| Female | 4 | 7 |
| Marital Status |
| Married and living withSpouse | 20 | 27 | 1 | 0.525 | 0.687 |
| Widow/Widower | 4 | 3 |
| Educational qualification |
| Primary | 22 | 25 | 1 | 0.821 | 0.443 |
| High school and above | 2 | 5 |
| Family income in Rs per month |
| < 5000 | 16 | 9 | 1 | 7.210 | 0.013* |
| 5001 And Above | 8 | 21 |
| Smoking |
| Yes | 11 | 15 | 1 | 0.093 | 0.761 |
| No | 13 | 15 |
| Tobacco chewing |
| Yes | 17 | 18 | 1 | 0.686 | 0.407 |
| No | 7 | 12 |
| Alcohol |
| Yes | 8 | 8 | 1 | 0.284 | 0.594 |
| No | 16 | 22 |
N=54; *=significant; p<0.05
Regarding disease related variables 19 out of 54 (35.19%) of them were suffering from cancer of oral cavity, 25 (46.3%) were with cancer of pharynx remaining 10 (18.51%) were suffering from other types of cancers such as cancer of larynx and thyroid. In relation to stage of cancer, 30 (55.5%) were suffering from stage III and stage IV of cancer, 46 (85.18%) were suffering from the disease for the duration of less than six months, 43 (79.6%) were receiving both radiation therapy and chemotherapy as a mode of treatment, 44 81.5%) were receiving radiation dose of 70 Gy/35#/7 weeks, 49 (90.7%) of them did not have any co morbidity, 16 (29.6%) had a mode of feeding other than oral (ryles tube and PEG feeding) and six (11.1%) had tracheostomy [Table/Fig-2].
Association between self-image and disease related variables.
| Variable | Negative self-image(Score between 18-45) | Positive self-image(Score between 46-72) | df | Chi-square (χ2) | p-value |
|---|
| Site of cancer |
| Oral cavity | 11 | 8 | 2 | 3.085 | 0.214 |
| Pharynx | 8 | 17 |
| Others | 5 | 5 |
| Stage of cancer |
| Stage I & II | 11 | 13 | 1 | 0.034 | 0.854 |
| Stage III & IV | 13 | 17 |
| Duration of illness |
| < six months | 21 | 25 | 1 | 0.183 | 0.720 |
| >Six months | 3 | 5 |
| Treatment modality |
| Only radiation therapy | 5 | 6 | 1 | 1.0 | 0.006* |
| Radiation &chemotherapy | 19 | 24 |
| Radiotherapy dose |
| 70 Gy/35#/7 weeks | 23 | 21 | 2 | 6.167 | 0.046* |
| 66Gy/33#/6.5 weeks | 1 | 5 |
| 60 Gy/30#/6 weeks | 0 | 4 |
| Co morbidities |
| Yes | 2 | 3 | 1 | 0.44 | 0.607 |
| No | 22 | 27 |
| Mode of feeding |
| Per oral | 14 | 24 | 1 | 3.002 | 0.083 |
| Ryle’s tube and PEG feeding | 10 | 6 |
| Tracheostomy |
| Yes | 3 | 3 | 1 | 1.00 | 0.084 |
| No | 21 | 27 |
N=54; *=significant; p<0.05
Association between self-image and demographic and disease related variables: In order to find the association between self-image and demographic and disease related variables Chi-square was computed. Fisher’s-exact test value was considered for frequencies less than five [Table/Fig-1].
Data presented in the [Table/Fig-1] shows that the α2 value for monthly income (7.210) was found to be statistically significant (α2 = 0.013) at 0.05 level of significance.
Data presented in the [Table/Fig-2] shows that the α2 values for treatment modality (1.0) and radiotherapy dose (6.167) which is found statistically significant (0.006 and 0.046) respectively at 0.05 level of significance.
Association between quality of life and demographic and disease related variables:
In order to find the association between quality of life and demographic and disease related variables Kruskal Wallis test was computed.
Data in [Table/Fig-3] shows that there was statistically no significant association between quality of life and demographic variables.
Association between quality of life and demographic variables.
| Variables | n | Mean rank | Kruskal Wallis test value | df | p-value |
|---|
| Age in years |
| <50 years | 18 | 30.75 | 1.155 | 1 | 0.283 |
| >50 years | 36 | 25.88 |
| Gender |
| Male | 43 | 27.63 | 0.014 | 1 | 0.906 |
| Female | 11 | 27 |
| Marital Status |
| Married and living with spouse | 47 | 28.95 | 3.073 | 1 | 0.080 |
| Widow/Widower | 7 | 17.79 |
| Educational qualification |
| Primary | 47 | 27.48 | 0.001 | 1 | 0.979 |
| High school and above | 7 | 27.64 |
| Family income in Rs per month |
| < 5000 | 25 | 24.12 | 2.154 | 1 | 0.142 |
| 5001 and above | 29 | 30.14 |
| Smoking |
| Yes | 26 | 26.13 | 0.379 | 1 | 0.538 |
| No | 28 | 28.77 |
| Tobacco chewing |
| Yes | 35 | 26.54 | 0.369 | 1 | 0.544 |
| No | 19 | 29.26 |
| Alcohol |
| Yes | 16 | 23.06 | 1.813 | 1 | 0.178 |
| No | 38 | 29.37 |
N=54; p<0.05
Data presented in the [Table/Fig-4] shows that the test values for mode of feeding (4.881) which is found statistically significant (0.027) at 0.05 level of significance.
Association between quality of life and disease related variables.
| Variables | n | Mean rank | Kruskal Wallis test value | df | p-value |
|---|
| Site of cancer |
| Oral cavity | 19 | 28.18 | 0.104 | 2 | 0.949 |
| Pharynx | 25 | 26.76 |
| Others | 10 | 28.05 |
| Stage of cancer |
| Stage I & II | 24 | 28.75 | 0.273 | 1 | 0.601 |
| Stage III & IV | 30 | 26.50 |
| Duration of illness |
| < Six months | 46 | 27.89 | 0.193 | 1 | 0.661 |
| >Six months | 8 | 25.25 |
| Treatment modality |
| Only radiation therapy | 11 | 31.82 | 1.043 | 1 | 0.307 |
| Radiation &chemotherapy | 43 | 26.40 |
| Radiotherapy dose |
| 70 Gy/35#/7 weeks | 44 | 25.05 | 7.054 | 2 | 0.029 |
| 66Gy/33#/6.5 weeks | 6 | 33.75 |
| 60 Gy/30#/6 weeks | 4 | 45.12 |
| Co morbidities |
| Yes | 5 | 20.60 | 1.062 | 1 | 0.303 |
| No | 49 | 28.20 |
| Mode of feeding |
| Per oral | 38 | 30.57 | 4.881 | 1 | 0.027* |
| Ryle’s tube and PEG feeding | 16 | 20.22 |
| Tracheostomy |
| Yes | 6 | 18.17 | 2.381 | 1 | 0.123 |
| No | 48 | 28.67 |
N=54; *=significant; p<0.05
Relationship between the quality of life and self-image of the patients with head and neck cancer:
Spearman rho was computed to find the relationship between quality of life and self-image. In order to assess the relationship between quality of life and self-image of patients with head and neck cancer following null hypothesis was stated.
H03→There will be no significant relationship between quality of life and self-image of the patients’ with head and neck cancers.
Data in the [Table/Fig-5] shows a positive correlation (r=0.613, p=0.001) between self-image and quality of life of head and neck cancer patients. Hence it can be inferred that as the quality of life of the head and neck cancer patient improves, better the self-image or vice versa. Hence, null hypothesis is rejected and research hypothesis is accepted.
Relationship between quality of life and self-image of patients with head and neck cancer.
| Variable | Spearman rho (r) value | p-value |
|---|
| Self-image | 0.613 | 0.001* |
| Quality of life |
N=54; *=significant; p<0.05
Discussion
The study intended to discover major socio-demographic and clinical characteristics that have a bearing on self-image and QOL of patients with head and neck cancer. Analysis of these characteristics showed statistically significant positive correlation between monthly income and mode of treatment with self-image. Quality of life was also significantly associated with mode of feeding. Findings of a study conducted by Asha S et al., among HNC patients showed that the subjects for whom the treatment had not yet started, showed better quality of life than those who were on treatment (P <0.001). Subjects undergoing palliative intent of treatment had poorer quality of life than others (P<0.001) [14]. The review on economic burden of cancer reported that in India, families of cancer patients cope with the financial distress by reducing the expenditure for other members or other aspects of life [15].
The results of this study also provide the relationship between quality of life and self-image of the patients among head and neck cancer. There was a significant positive correlation between the quality of life and self-image. Researchers couldn’t find any published researches in the field of association between self-image and quality of life among HNC patients, in data bases including PubMed, CIHNAL, Proquest and Google scholar.
HNC patients are having high potential for disturbance in body image because of visible location of the disease and targeted treatments. The findings corresponding to the present study were found in a study conducted to assess the body image and depressive symptoms in patients with HNC. There was a statistically significant relationship between body image and depressive symptoms at the end of six weeks and 12 weeks of post treatment (r-0.32 to -0.56, p<0.05) [9] .
Different level of disfigurement due to surgery, treatment or disease condition resulted negative body image which was highly correlated among the psychological aspects such as anxiety; communication etc., was reported in several research studies. Anticipation in facial disfiguration followed by surgery is highly associated with anxiety with decline in coping effectiveness. Reintegration of body image is critical for subsequent quality of life among HNC patients [16].
Living with visibly disfiguring body is not an easy experience for head and neck cancer patients. A study was conducted among 120 cancer patients by Arunachalam D et al., with the aim of evaluating the effect of disfigurement because of cancer and its treatment on quality of life. Stigma showed a significant difference in its means for the quality of life (F = 4.018, P < 0.05). For both genders disfigurement clearly was a stressful experience but substantially more distressing for women. Poor quality of life was experienced in all dimensions of quality of life and sociodemographic variables among majority of HNC patients [17].
Dissatisfaction with body image and more negative body image is observed among HNC patients with advanced stage of cancer, tumour on the facial area and undergoing reconstructive surgeries. Interventions are very much essential for facilitating positive body image [18]. Radical surgery for HNC patients, especially for that undergoing facial bone destructive surgery has a significant impact on their body image. In a study conducted by Hung et al., showed that Body Image Scale (BIS) scores strongly impacted by radical surgery. Significantly worse BIS scores were found among patients treated surgically than the patients without surgery (p< 0.001) [19].
One of the challenges faced by HNC patients is loss of confidence due to the felt changes in their appearance. HNC patients were also treated differently due to their speech deficits which have heightened the perception of change in the self-image. Changes in the functions such as eating, drinking, hearing along with the appearance had a great impact on their confidence. Loss of dignity is also experienced by most of them due to disfigurement of image [7].
Deterioration in basic functions such as breathing, chewing, speaking, salivation and swallowing are most frequently determined by the diagnosis and treatment. Aesthetic changes and sensory impairment such as smell, taste and hearing promotes negative impact on HRQOL among patients with HNC and their relatives. Hence, head and neck cancer is undoubtedly related to a decrease in HRQOL [20].
Various qualitative researches conducted in the field of HNC to assess the quality of life also revealed similar findings. In a qualitative study conducted in Atlanta, to assess the Communicating suffering in primary stage of HNC emerged with a theme of “hopelessness and the loss of meaning in life” after squamous cell carcinoma of the head and neck [21]. Patients with head and neck cancer could experience life threatening effect on vital functions and visible disfigurement. This could lead to more emotional trauma than any other type of cancer. Lifestyle changes such as working everyday tasks, social function, interpersonal relationships and physical functions are often the consequences of long term illness. A qualitative and explorative longitudinal study conducted among HNC patients in Sweden to illuminate what it means to live with head and neck cancer showed that the participants were living ‘in captivity’ in the sense that their symptoms were constant reminders of the disease. Thus, living with HNC involves emotional and existential vulnerability [22].
Limitation
The study was cross-sectional design and recall bias, changes in self–image and quality of life across the time cannot be evaluated. The study was conducted in the inpatient environment. In this type of studies, data are limited to inpatient environment such as availability of private rooms, noise level, patient and family interactions etc.
Conclusion
In summary, there is a preliminary research elucidated the relationship between quality of life and self-image of the patients with HNC. However, there was no association between many of the demographic and disease related variables with self-image and quality of life.
Declaration
This is to certify that this manuscript is original research carried out by the authors. This study has been presented at the Indian Cancer Congress held at Bangalore, India during November 08-12, 2017 and the conference abstract is published in the Journal of Cancer Research and Therapeutics (JCRT) as supplement.
N=54; *=significant; p<0.05
N=54; *=significant; p<0.05
N=54; p<0.05
N=54; *=significant; p<0.05
N=54; *=significant; p<0.05