Are Automated Blood Pressure Apparatus Reliable? Automated Versus Manual Measurement of Blood Pressure
K Madhan Srinivasan1, K Senthil Kumar2, I Saraswathi3, A Lokeshwar Raaju4, B Vishwanatha Rao5
1 Medical Student, Madha Medical College and Research Institute, Chennai, Tamil Nadu, India.
2 Associate Professor, Department of Physiology, Meenakshi Medical College and Research Institute, Kanchipuram, Tamil Nadu, India.
3 Assistant Professor, Department of Physiology, Madha Medical College and Research Institute, Chennai, Tamil Nadu, India.
4 Medical Student, Madha Medical College and Research Institute, Chennai, Tamil Nadu, India.
5 Professor, Department of Physiology, Madha Medical College and Research Institute, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. K Senthil Kumar, Associate Professor, Department of Physiology, Meenakshi Medical College and Research Institute, Kanchipuram, Tamil Nadu, India.
E-mail: drksk.cool@gmail.com
Introduction
With hypertension becoming a global burden, it is necessary to validate the Blood Pressure (BP) recordings, used to screen and follow-up patients for hypertension. Since three different devices (mercury manometer, aneroid meter, and digital) are commonly used throughout the world, a study was proposed to compare the recordings of the three devices.
Aim
To evaluate the validity of aneroid and digital BP monitors as compared to mercury manometer.
Materials and Methods
BP was measured in 240 healthy subjects of both sex (Male=127, Female=113) using mercury manometer, aneroid and digital BP monitor from the same arm consecutively with five minutes interval between each recording. The data were analysed using SPSS 21, Systolic Blood Pressure (SBP) and Diastolic Blood Pressure (DBP) readings of aneroid and digital monitors were compared with mercury manometer. British Hypertension Society (BHS) protocol, Association for the Advancement of Medical Instrumentation (AAMI) standards and Bland Altman scatter plots were used to validate the aneroid and digital BP monitors.
Results
The difference in SBP measured using mercury manometer and aneroid meter was 0.675±7.12 mmHg and mercury manometer and digital monitor was 1.65±11.08 mmHg. The difference in DBP using mercury manometer and aneroid meter was 1.75±6.3 mmHg and mercury manometer and digital was 2.76±8.8 mmHg. While aneroid meter satisfied the AAMI criteria, digital monitor did not. The BHS grade for aneroid meter was C (poor) and digital D (very poor). According to Bland-Altman plot, the bias in SBP for aneroid was minimal with 0.675 (-13.28-14.63), for digital -1.41 (-21.66-18.84) and in DBP for aneroid was 1.75 (-10.6-14.1), for digital was the highest with 2.76 (-14.47-20.01).
Conclusion
BP measured using aneroid and digital monitors varied significantly from the mercury manometer and showed higher levels of inaccuracy and hence should be used with caution in clinical setting.
Advancement of medical instrumentation, Bland-Altman scatter plots, British hypertension society, Validation
Introduction
Around the globe every year around 9.4 million people die due to hypertension, and it is one of the most important causes of premature death. Complications from hypertension is also growing every year, affecting approximately one billion people, especially in low, lower and middle income countries [1]. Hypertension is a major risk factor for cardiac disease and stroke and the most common cause for mortality throughout the world [2]. BP measurement is an integral part of clinical practice. An accurate measurement is critical in arriving at a diagnosis and hence vital in providing treatment. Inaccurate measurements of false high BP may lead to unnecessary medications and dietary modifications or exposure to adverse effects of drugs in addition to the monetary burden. The false reporting of low BP leads to under diagnosis of hypertension in early stages.
Direct method of BP measurement is invasive and seldom used in daily clinical practice. The indirect methods of measuring BP include use of mercury manometer, aneroid meter and automated oscillometric device like digital BP apparatus. Though BP measurement using mercury manometer is considered to be the gold standard [3], the usage of automated devices is on the rise. With the increase in awareness about mercury being toxic and an environmental hazard, and the digital BP apparatus being convenient for usage, mercury manometer usage is slowly being replaced by automated ones. However, there have been studies questioning the accuracy and reliability of automated BP monitors [4,5]. There are aneroid meters to record BP which do not contain mercury but they need periodic cross checking with mercury manometer.
Poor manual BP measurement techniques could result in imprecise results [6,7]. Inappropriate therapeutic protocol due to an error in recording BP may adversely affect clinical outcome following treatment. Thus, following steadfast precautions while using each device is vital and so is validating the automated BP monitors.
BHS protocol and the standards given by the AAMI are the internationally recognised criteria for determining the accuracy and reliability of the automated instruments [8,9]. The bias in the readings between the automated measurements and manual ones could be derived using the Bland Altman scatter plots. In the present study, we evaluated the accuracy and reliability of the digital BP monitor and aneroid meter by comparing with the mercury manometer using the BHS protocol, AAMI standards and Bland Altman scatter plots.
Materials and Methods
This cross-sectional study was conducted in a teaching hospital in Chennai, Tamil Nadu, India using 240 subjects who attended the medicine outpatient department.
The participants included were in age group of 20-80 years of both the genders were included in the study. Patients with normal BP and willing to participate in the study were included in the study. Patients who were critically ill, known hypertensives, neurological diseases, renal and endocrine disorders were excluded from the study.
The study was explained to the subjects in their native tongue and consent was obtained. Subjects of both the gender of age group 20-80 years without any neurological, renal or endocrine disorders were selected for the study.
The study was carried out during the months of April to August 2014 in the General Medicine outpatient department of a teaching hospital in Chennai. Approval from the institutional ethical committee was obtained before the beginning of the study.
BP Measurement
BP was measured in the right arm of all the subjects after five minutes rest. DIAMOND Sphygmomanometer (ideal surgical company, India) with Littmann classic II stethoscope (3M, USA), DIAMOND aneroid meter (Ideal surgical company, India) with Littmann classic II stethoscope (3M, USA), and OMRON digital BP monitors (Omron Healthcare Manufacturing Vietnam Company, Singapore) were used to record the resting BP. Five minutes of interval was given between consecutive readings. The subjects were seated comfortably with back supported and right arm bared, with no constrictive clothing and legs uncrossed. The arm of the subjects was supported at the level of the heart and the cuff was chosen so that it covered 80% of the arm circumference. The mercury column was deflated at 2 to 3mm/sec and care was taken that neither the subject nor the observer talk during the measurement. Three trained observers (Two trained second year MBBS students and one physiology assistant professor) recorded the BP independently to avoid observer bias. Each observer recorded the BP thrice with gap of five minutes and the best of the three measurements were documented.
Statistical Analysis
The data were analysed using SPSS version 21.0. The mean and standard deviation of the BP measured using sphygmomanometer was compared with the aneroid measurements and digital measurements using paired t-test. A p-value of <0.05 was taken to be statistically significant. The mean and standard deviation of difference between the sphygmomanometer and aneroid readings and sphygmomanometer and digital readings were used to test the AAMI criteria. The cumulative percentage of absolute difference between the sphygmomanometer and aneroid readings and sphygmomanometer and digital readings were calculated in Microsoft Excel 2010 and tested for the BHS criteria. The Bland-Altman scatter plots were prepared using Microsoft Excel 2010.
Results
Comparison of measurements of both SBP and DBP using sphygmomanometer and aneroid meter showed that the mean difference between the two methods for SBP was 0.675±7.12 mmHg and for DBP it was 1.75±6.3 mmHg [Table/Fig-1]. Thus the measurements done using aneroid meter satisfies the AAMI criteria which specify a mean difference between devices of <5 mmHg with a standard deviation of ≤8 mmHg [10]. While comparing the SBP and DBP measurements using sphygmomanometer and digital methods, the mean difference for SBP was found to be 1.65±11.08 mmHg and for DBP, 2.76±8.8 mmHg [Table/Fig-2]. Thus the measurements using digital method do not satisfy the AAMI criteria for both SBP and DBP where the standard deviation remains higher than the required 8 mmHg.
Comparison of measurements between sphygmomanometer and aneroid methods. Validation using AAMI criteria.
| Manual | Aneroid | Paired t-test | Difference scores |
|---|
| (Mean±SD) | (Mean±SD) | p-value | (Mean±SD) | 95% CI |
|---|
| SBP | 118.63±15.65 | 117.96±15.34 | 0.143 | 0.675±7.12 | -0.23-1.58 |
| DBP | 77.37±9.66 | 75.62±9.53 | 0.000*** | 1.75±6.3 | 0.95-2.95 |
SBP - Systolic Blood Pressure, DBP - Diastolic Blood Pressure. Values are represented in mmHg ***p-value < 0.001 considered high statistical significance
The comparison of measurements between sphygmomanometer and digital methods. Validation using AAMI criteria.
| Manual | Digital | Paired t-test | Difference scores |
|---|
| (Mean±SD) | (Mean±SD) | p-value | (Mean±SD) | 95% CI |
|---|
| SBP | 118.63±15.65 | 120.28±16.87 | 0.02** | 1.65±11.08 | -3.06-0.24 |
| DBP | 77.37±9.66 | 74.61±11.44 | 0.000*** | 2.76±8.8 | 1.64-3.88 |
SBP: Systolic Blood Pressure; DBP: Diastolic Blood Pressure; Values are represented in mmHg
***p-value <0.001 considered high statistical significance
While focusing on the BHS criteria [Table/Fig-3], the absolute difference in the measurements using sphygmomanometer and aneroid meter falls under grade C for both SBP and DBP which is considered to be poor validation [Table/Fig-4] and in case of digital measurements, it falls under grade D for SBP and DBP which is considered to be very poor validation [Table/Fig-5]. The grades represent the cumulative percentage of the absolute difference between the readings falling within 5, 10, 15 mmHg of the standard sphygmomanometer readings. Grade A and B are acceptable for the usage of the devices while grades C and D are not recommended [8].
British hypertension society criteria.
| Grades | Cumulative percentage of absolute difference |
|---|
| ≤5 mmHg | ≤10 mmHg | ≤15 mmHg |
|---|
| Grade A (very good) | 60% | 85% | 95% |
| Grade B (good) | 50% | 75% | 90% |
| Grade C (poor) | 40% | 65% | 85% |
| Grade D (very poor) | Worse than C |
BHS grades for sphygmomanometer versus aneroid measurements.
| Cumulative percentage of differences | Grades |
|---|
| ≤5 mmHg | ≤10 mmHg | ≤15 mmHg | |
|---|
| SBP | 42% | 70% | 86% | C |
| DBP | 40% | 75% | 87% | C |
BHS grades for sphygmomanometer versus digital measurements.
| Cumulative percentage of differences | Grades |
|---|
| ≤5 mmHg | ≤10 mmHg | ≤15 mmHg | |
|---|
| SBP | 32% | 66% | 62% | D |
| DBP | 28% | 45% | 79% | D |
To evaluate the agreement between the manual and automated devices, Bland-Altman scatter plots were used, where the mean of the readings taken by the two methods is plotted against the difference in the readings [11]. The Limits Of Agreement (LOA) are calculated using the formula:,
LOA=Mean±1.96xStandard deviation.
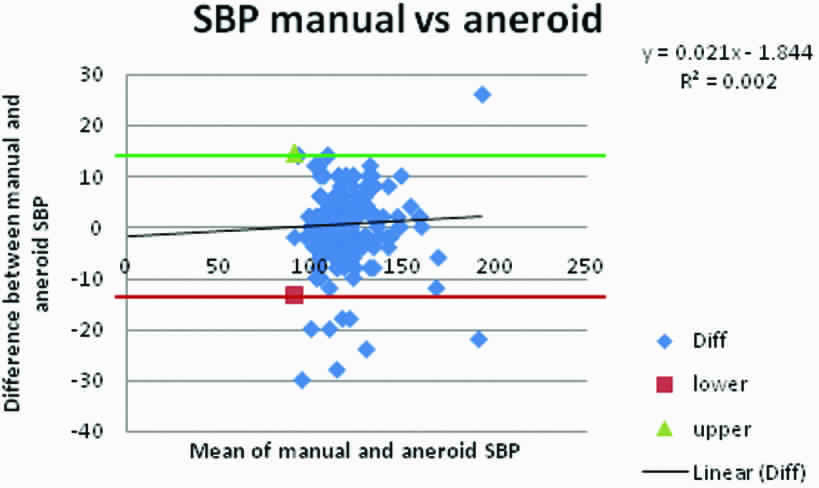
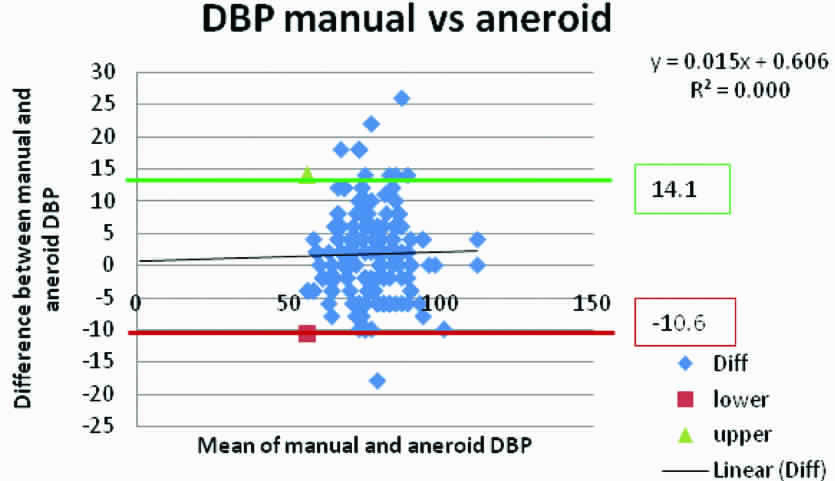
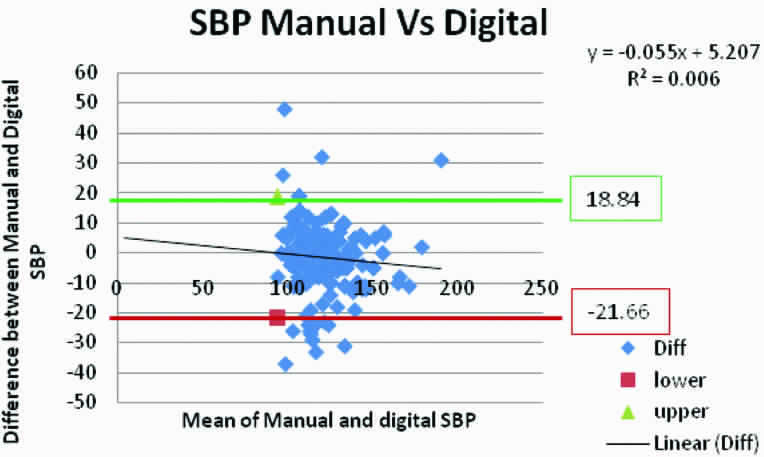
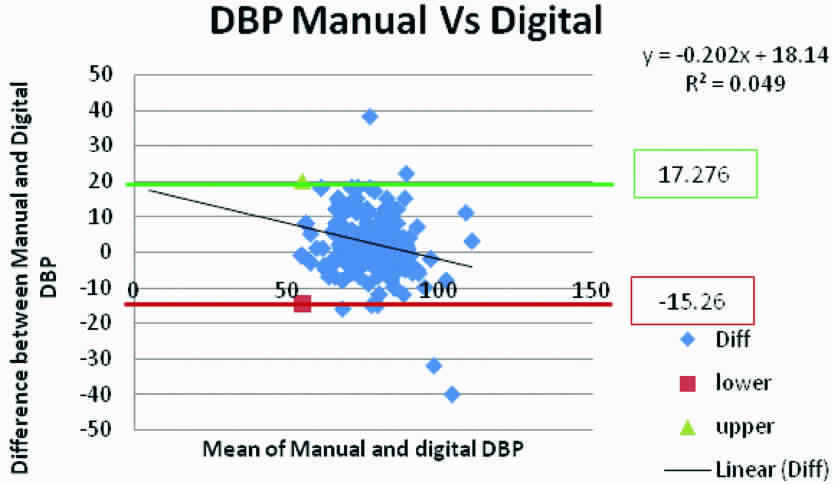
[Table/Fig-6] shows the Bland-Altman scatter plots where mean of the SBP readings from sphygmomanometer and aneroid are plotted against difference in the readings between the two. The bias (average variation in the readings from standard) was 0.675 with the limits of agreement from -13.28 to 14.63. The bias in DBP readings between sphygmomanometer and aneroid was 1.75 (-10.6-14.1) [Table/Fig-7]. Bland Altman plot of sphygmomanometer versus digital readings show a bias of -1.41 with the limits of agreement from -21.66 to 18.84 for SBP [Table/Fig-8] and 1.008 (-15.26 – 17.276) for DBP [Table/Fig-9]. Most of the readings in all the plots lie with the limits of agreement.
Bland-Altman plot of SBP measured by manual and aneroid method of BP measurement.
Correlation R=0.04514 (p=0.48); Slope=0.0213 (p=0.487); Intercept=-1.844 (p=0.61); Bias=0.675 (-13.28-14.63); The upper and lower limits of agreement are given in boxes
Bland-Altman plot of DBP measured by manual and aneroid method of BP measurement.
Correlation R=0.021 (p=0.74); Slope=0.015 (0.74); Intercept=0.607 (p=0.86); Bias=1.75 (-10.6-14.1); The upper and lower limits of agreement are given in boxes
Bland-Altman plot of SBP measured by manual and digital method of BP measurement.
Correlation R=0.0817 (p=0.21); Slope=-0.12 (p=0.20); Intercept=119.17 (p<0.00***); Bias=-1.41 (-21.66-18.84); The upper and lower limits of agreement are given in boxes
Bland-Altman plot of DBP measured by manual and digital method of BP measurement.
Correlation R=0.249 (p <0.00***); Slope=-0.213 (p <0.00***); Intercept=17.052 (p<0.00***); Bias=1.008 (-15.26-17.276); The upper and lower limits of agreement are given in boxes
Discussion
This study was conducted to assess the reliability and accuracy of the aneroid meter and digital BP monitors which are off late used in an increasing level in clinical practice to measure BP. The readings produced by aneroid and digital monitors are compared with that of the manual mercury manometer technique and their validity is tested against three well recognised criteria for the usage of medical devices viz., AAMI criteria, BHS protocol and Bland Altman plots. Aneroid meter satisfied the AAMI criteria while digital did not and both aneroid and digital showed minimal bias with a majority of reading lying between the limits of agreement in the Bland Altman plots. But on focussing on the BHS protocol both the aneroid and digital methods got poor validation. The devices used were pre-validated before the beginning of the study despite which the aneroid meter showed poor reliability according to one of the criteria and the digital monitor showed poor reliability according to two out of the three criteria.
For more than two centuries, mercury sphygmomanometer was considered synonymous to BP measurement. But mercury manometers pose a threat where they are the main source of mercury pollution and WHO considers it to be a serious occupational hazard [12]. Mercury is a neurotoxin and produces severe health hazards. It is prohibited in some parts of the world and the European Union is suggesting a more widespread ban [13]. Many countries have completely moved on from manual mercury manometers to record BP and rely on automated ones [14]. The automated devices can be recorded by anyone without proper training and were also proven to have less of white coat effect on patients [8,15].
Separate protocols and criteria are available to validate the automated devices. There are studies with evidence to limit the usage of automated devices on normotensives and not on hypertensives [15,16]. In our study we found that digital monitor and aneroid too either over read or under read the BP and this tendency of the automated devices was reported by a few studies, irrespective of whether readings were taken from healthy children [17], children with diabetes [18], or adult patients attending a hospital emergency department [19] or day surgery clinic [16]. In case of trauma or in patients with deteriorating conditions, inaccurate reading from automated BP monitors could have grave consequences.
Aneroid meter showed far more reliability than digital BP monitors but nevertheless there were discrepancies. But as mentioned earlier they need periodic calibration requiring sphygmomanometers and their preference over sphygmomanometer taking in to account of the mercury hazards overweighs its relative diminished reliability. Since both sphygmomanometers and aneroid meters need trained professionals to record BP, their white coat effect is also comparatively more than digital monitors [8, 15]. With the increased usage of automated devices to measure BP, physician’s awareness of the variations in their readings is vital.
Limitation
Limitations of the study are the age group included were of wider range. Recording were done at different times rather than being simultaneous.
Conclusion
Automated BP measurements were found to produce discrepancies in reading in clinical settings. The reliability and accuracy of the automated devices are questionable. Though, digital BP monitors have more convenience based advantages over manual methods, their usage should be done with increased caution. Mentioning of the type of instrument which was used to measure the BP should be included in patient’s data.
SBP - Systolic Blood Pressure, DBP - Diastolic Blood Pressure. Values are represented in mmHg ***p-value < 0.001 considered high statistical significance
SBP: Systolic Blood Pressure; DBP: Diastolic Blood Pressure; Values are represented in mmHg
***p-value <0.001 considered high statistical significance
[1]. Tesfaye T, Assessment of the prevalence of hypertension and associated factors among Ethiopian Federal Police Officers Addis Ababa, Ethiopia: A community based cross-sectional studyEC Cardiology 2017 2(6):278-86. [Google Scholar]
[2]. Lawes CM, Vander Hoorn S, Rodgers A, International Society of Hypertension. Global burden of blood-pressure-related diseaseLancet 2008 371:1513-18.10.1016/S0140-6736(08)60655-8 [Google Scholar] [CrossRef]
[3]. Ogedegbe G, Pickering T, Principles and techniques of blood pressure measurementCardiology Clinics 2010 28(4):571-86.10.1016/j.ccl.2010.07.00620937442 [Google Scholar] [CrossRef] [PubMed]
[4]. Carney S.L, Gillies A H, Green S L, Paterson O, Taylor M. S, Smith A J, Hospital blood pressure measurement: staff and device assessmentJournal of Quality in Clinical Practice 1999 19:95-98.10.1046/j.1440-1762.1999.00308.x10408749 [Google Scholar] [CrossRef] [PubMed]
[5]. O’Brien E, Waeber B, Parati G, Staessen J, Myers M G, Blood pressure monitoring devices: Recommendations of the European Society of HypertensionBritish Medical Journal 2001 322:531-36.10.1136/bmj.322.7285.53111230071 [Google Scholar] [CrossRef] [PubMed]
[6]. Reeves RA, Does this patient have hypertension? How to measure blood pressureJAMA 1995 273:1211-16.10.1001/jama.1995.035203900710367707630 [Google Scholar] [CrossRef] [PubMed]
[7]. O’Brien E, Asmar R, Beilin L, Imai Y, Mallion J-M, Mancia G, European Society of Hypertension recommendations for conventional, ambulatory and home blood pressure measurementJournal of Hypertension 2003 21:821-48.10.1097/00004872-200305000-0000112714851 [Google Scholar] [CrossRef] [PubMed]
[8]. O’Brien E, Petrie J, Littler W, de Swiet M, Padfield P, Altman D, The British Hypertension Society protocol for the evaluation of blood pressure measuring devicesJournal of Hypertension 1993 11(Suppl 2):S43-S62. [Google Scholar]
[9]. White W B, Berson A S, Robbins C, National standard for measurement of resting ambulatory blood pressure with automated sphygmomanometersHypertension 1993 21:504-09.10.1161/01.HYP.21.4.5048458649 [Google Scholar] [CrossRef] [PubMed]
[10]. Association for the Advancement of Medical Instrumentation. American national standard. Electronic or automated sphygmomanometers. ANSI/AAMI SP 10- 1992. AAMI: Arlington, VA, 1993, Pp.40 [Google Scholar]
[11]. Bland JM, Altman DG, Statistical methods for assessing agreement between two methods of clinical measurementLancet 1986 1:307-310.10.1016/S0140-6736(86)90837-8 [Google Scholar] [CrossRef]
[12]. World Health Organization. Department of Protection of the Human Environment Water, Sanitation and Health. Mercury in Health Care. August 2005 [Google Scholar]
[13]. Hospitals for a Healthy Environment. Regulated Medical Waste Reduction. http://www.h2e-online.org [Google Scholar]
[14]. Shahbabu B, Dasgupta A, Sarkar K, Sahoo SK, Which is more accurate in measuring the blood pressure? aA digital or an aneroid sphygmomanometerJ Clin Diagn Res 2016 10(3):LC11-LC14.10.7860/JCDR/2016/14351.745827134902 [Google Scholar] [CrossRef] [PubMed]
[15]. Myers MG, McInnis NH, Fodor GJ, Leenen FHH, Comparison between and Automated and manual sphygmomanometer in a population surveyAm J Hypertens 2008 21(3):280-83.10.1038/ajh.2007.5418219304 [Google Scholar] [CrossRef] [PubMed]
[16]. Coe T R, Houghton K, Comparison of the automated Dinamap blood pressure monitor with the mercury sphygmomanometer for detecting hypertension in the day case pre assessment clinicAmbulatory Surgery 2002 10:9-15.10.1016/S0966-6532(01)00112-3 [Google Scholar] [CrossRef]
[17]. Barker M E, Shiell A W, Law C M, Evaluation of the Dinamap 8100 and Omron M1 blood pressure monitors for use in childrenPaediatric and Perinatal Epidemiology 2000 14:179-86.10.1046/j.1365-3016.2000.00250.x10791663 [Google Scholar] [CrossRef] [PubMed]
[18]. Jin R Z, Donaghue K C, Fairchild J M, Chan A, Silink M, Comparison of Dinamap 8100 with sphygmomanometer blood pressure measurement in a prepubertal diabetes cohortJournal of Paediatric Child Health 2001 37:545-49.10.1046/j.1440-1754.2001.00752.x11903832 [Google Scholar] [CrossRef] [PubMed]
[19]. Chong W F, Tan C H P, Yeo S L R, Ching S S, Cheng L, A study on reliability and accuracy of digital and manual sphygmomanometersSingapore Nursing Journal 2000 27:28-35. [Google Scholar]