Asthma and COPD are among the most common chronic diseases requiring hospital admissions worldwide [1,2]. Inhaler therapy using MDI is one of the mainstay of therapy of these disorders; however, the efficacy of drug delivery depends largely on the technique of MDI use. Incorrect use of MDI is common [3]. Even healthcare providers can fail to demonstrate this technique [4]. Faulty technique of inhaler use by the patient is associated with old age, low education status and lack of prior demonstration by healthcare provider [5].
Spacer is an add on device placed between patient’s mouth and MDI, and it’s use has been found to reduce oropharyngeal deposition by as much as 99%, increase inhaled medication fourfold compared to MDI alone, and help in those with poor hand breath coordination [4]. Latest Global Initiative for Asthma (GINA) report 2017 recommends use of spacer with MDI as it will improve drug delivery and reduce the potential for side effects. A study prior to this recommendation had shown that the prescription and strict use of spacer might be as low as 36% [6].
Previous studies have shown that practical demonstration is the best method to educate patients about optimum inhaler use [6-9]. In spite of the established importance of proper MDI technique, studies targeting the applicability and impact of physical demonstration using a standard checklist for MDI, specifically with spacer in a busy healthcare setting like in India are limited. We conducted this prospective study to analyse the current practice of MDI with spacer use, to assess the common errors that occur that occur in using MDI and to study the effect of a practical demonstration using a standardized checklist on these errors. A questionnaire based survey was also done among doctors to know the current practice of MDI education.
Materials and Methods
The study was having an interventional pre and post-test design and was conducted from January 2016 to March 2016. Participants were recruited from a busy Medicine OPD at All India Institute of Medical Sciences (AIIMS), New Delhi, India. Patients of Asthma or COPD were included, if they were already using MDI, were older than 14 years of age and gave written informed consent. Patients who were on other inhaler devices and those who had linguistic difficulty in understanding the education were excluded. Ethical approval was obtained from Institute Ethics Committee and informed written consent was obtained from all participants.
Three doctors who were trained simultaneously regarding the MDI use technique evaluated the patients. The proposed sample size was 100, which was a sample size of convenience. In our study 102 patients were recruited and evaluated for MDI use. At baseline, a predesigned questionnaire regarding the patient’s demographics, their perception regarding whether they knew how to use MDI, whether they were advised regarding spacer and whether there was a history of a prior demonstration by any healthcare provider was administered. Following baseline assessment, patients were asked to demonstrate use of MDI and they were scored according to a standard checklist of recommended steps with each correct step being awarded 1 point for a total of 8 points (Adapted from ADMIT-GINA inhaler guidelines-[Table/Fig-1] [10].
| Step 1-Remove cap and shake inhaler.Step 2-Assemble spacer and insert MDI into it.Step 3-Place mouthpiece in mouth between teeth and close lips without leaving any gap.Step 4-Start breathing in and out slowly and gentlyStep 5-Once breathing is well established depress canisterStep 6-Leave device in same position and continue to breath several more timesStep 7-Remove device from mouthStep 8-Wait about 30 seconds before repeating. |
Following the initial scoring, a practical demonstration of correct MDI use along with spacer, using a placebo canister was done by the doctor with emphasis on the steps, which the patient had performed incorrectly. The instructions were repeated until the patient was found to demonstrate the technique correctly. Along with the technique, holistic information regarding MDI and spacer use was imparted including methods of cleaning, importance of using numbered MDI, and avoidance of exacerbating factors such as pollen, animal dust or cold environment. To ensure repeatability these instructions were also written and kept as a checklist.
The patients were asked to follow up after one month, and their technique was again scored using the same checklist. To ensure that strict follow up was done appointment for the intervention was given in the OPD card along with next OPD visit appointment. Those who didn’t attain full scores were given repeat demonstration and education. Since the proportion of patients lost to follow up was large (46 patients), we telephonically contacted them to find out the causes of lost to follow-up. Along with this study, a questionnaire based survey was done among medical practitioners in the same OPD, focusing on whether they demonstrate MDI technique and whether they reassess on follow-up. In the survey 24 doctors of the age group 24 to 28 years who were doing their residency program responded.
Statistical Analysis
Data were recorded in a pre-designed performa and managed on an excel spreadsheet. Categorical variables were summarized as frequency (percentage). Continuous variables were summarized as mean and Standard Deviation (SD) or median and range (when SD was >50% of mean). Normalcy of data was assessed using Shapiro-Wilk test. Paired t-test was used to compare the total score pre- and post-intervention to judge the efficacy of the intervention. Statistical analysis was performed using Stata 12 software (StataCorp. 2011. College Station, TX).
Results
In the study, 102 patients were recruited and evaluated for the MDI technique as well as educated according to the checklist. However, 46 were eventually lost to follow-up and finally 56 patients were included in the analysis according to per protocol analysis. Although, we had many dropouts as elucidated, the final sample size was adequate and the study was adequately powered to meet its primary objective (power >99.9%).
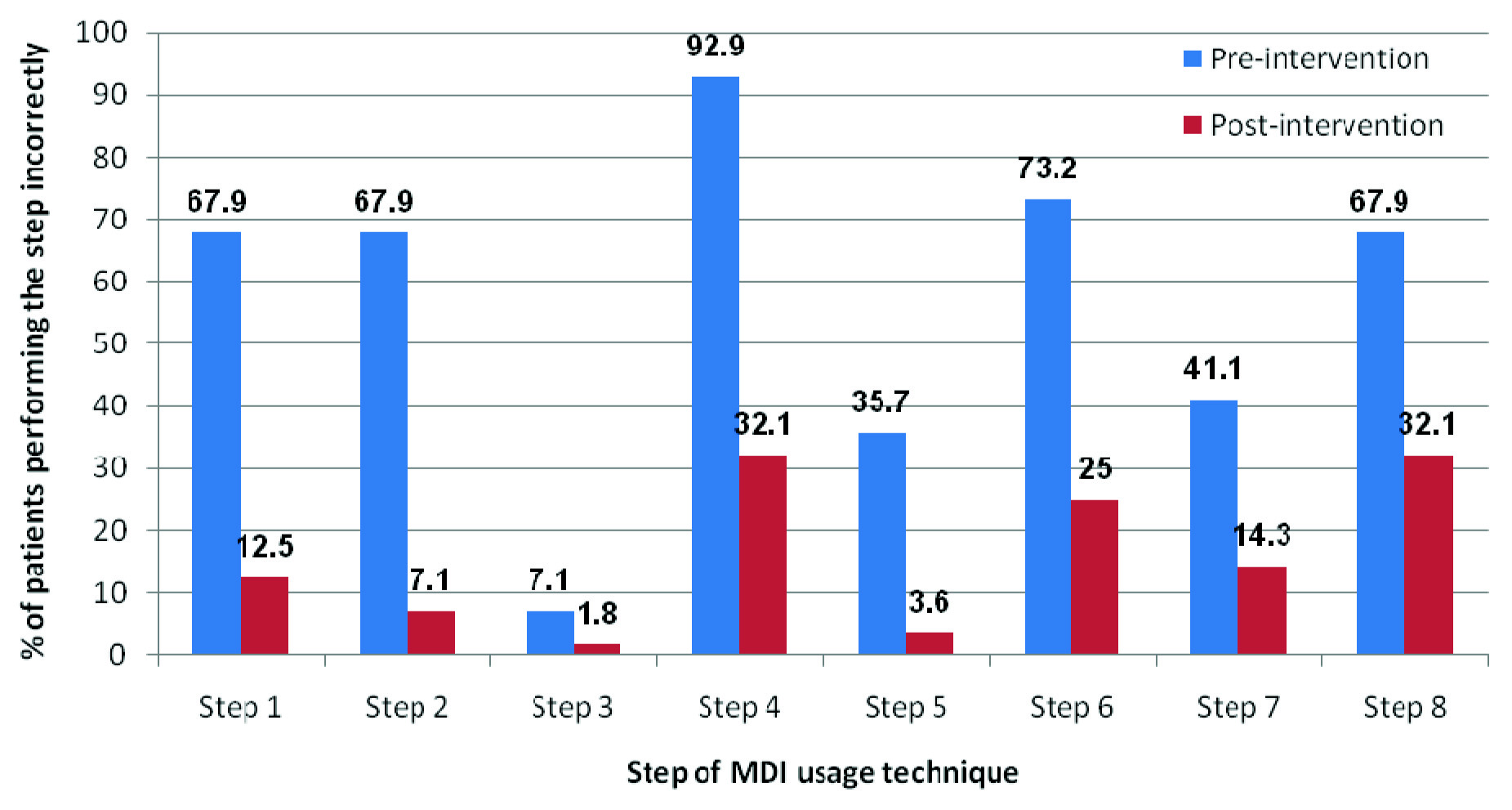
The study population was well distributed across all age groups, mimicking the distribution in the national population. There were 37 males (66.1%). The mean age of the study population was 37.3 (±13) years; none of the participants were below 18 years. Forty two patients suffered from bronchial asthma whereas 14 had COPD. Only slightly less than half of patients (48.2%, n=27) had received any prior MDI use instructions. Only 22 (39.3%) patients were advised regarding spacer use. An enquiry on patient perception at baseline revealed that 80.4 % (n=45) patients felt that they knew how to use MDI correctly. None of the subjects could perform all steps correctly at baseline. Most (92.9%) of the patients performed step 4 (breathing in and out slowly after keeping the spacer inside mouth) of the technique incorrectly. Maximum percentage improvement with intervention was also noted in this step [Table/Fig-2].
Proportion of patients with incorrect steps in MDI use technique, at each step, at baseline and post-intervention.
Around one third patients (30.3%, n=17) could perform all steps correctly post intervention, reflected by a score of 8, while just three patients had no change in scores despite intervention. The pre-intervention score showed a weak positive correlation with previous training experience (r=0.17) (CI -0.093 to 0.418) and showed a trend towards weak correlation with the duration of MDI use (r=-0.025 (CI-0.287 to 0.239), although the CI crossed zero, probably because of low sample size. The mean (SD) score (by paired t-test) at baseline was 3.5 (±1.5), which increased to 6.7 (±1.2) after intervention. To compare the efficacy of our intervention, the post intervention score was compared with the baseline score using paired t-test and a statistically significant improvement in mean scores was noted with intervention (6.7 versus 3.5, p<0.001).
An attempt to understand the reason for loss to follow up was made via telephonic contact. Ten patients found it inconvenient to visit the hospital for the sole purpose of follow up because of considerable distance between their place of residence and the hospital. Four patients cited improvement in their disease as the reason for not following up. In 31 (67%) out of the total 46 losses, the telephone numbers provided by the patients were found to be incorrect or not reachable.
The survey among medical practitioners revealed that as high as 70.84% did not demonstrate MDI use in OPD setting, and only one third of them (37.5%) assessed the technique on subsequent follow up visits, possibly due to work burden and time constraints.
Discussion
In the present study, to assess the usual errors while using MDI with spacer and to assess the impact of a practical demonstration on these errors. It was observed that patient’s perception regarding their knowledge of MDI use was falsely high with around 80.4% of patients feeling they knew how to correctly use MDI, but none of them demonstrated the technique correctly prior to intervention. Therefore in an OPD, asking the patient to demonstrate MDI use will be more informative for physicians than inquiring about their perception of use. The prolonged use of MDI might be one factor which gives a false confidence to the patient regarding the correctness of their technique, and we should realize that duration of use does not ensure correctness and regular assessment and education sessions are necessary. Only 39.3% of the patients were previously advised regarding using spacer which was similar to the figures in the study by Jolly GP et al., [6]. This is of concern as it has been recommended for wider use in GINA guidelines 2017 [11].
Each clinician should know how to select an inhaler, its advantages, limitations and technique of MDI use and ideally should educate the patient regarding this when given an opportunity. In our survey of physicians it was seen that only 37.5% doctors assess MDI technique on follow-up. The history of prior MDI education by a health care provider was seen only in 48% patients, which corresponds to results of a previous study [6]. The busy OPD setting and time constraints might be the main factor behind this low numbers. If doctors themselves are unable to do this due to time concerns, nurses and pharmacists also can equally help in this regard [12-14]. In our context we plan to utilize the services of the nursing staff posted in the PFT lab which is inside our medical OPD to ensure the sustainability of this intervention.
In the present study, intervention showed a statistically significant improvement in MDI technique knowledge (6.7 versus 3.5, p<0.001) and around 17 patients could perform all steps correctly on follow-up, proving that systematic education including practical demonstration is the best way for MDI education. Patients most commonly erred on step 4 of the technique where they were supposed to establish a slow in and out breathing pattern before pressing the MDI canister [Table/Fig-2]. As maximum errors were seen in this step, specific stress should be given to this step during demonstration. Failure to recognize empty canisters will lead to ineffective drug intake, hence this aspect was included in the present study MDI education [4]. Even after fully learning the technique, temporal decline in knowledge requiring repeated demonstrations had been seen among our patients and in some previous studies [6,15]. Studies have shown that correcting the MDI use technique will lead to better asthma control, lesser need for rescue medications, and fewer night waking and the present study will also contribute to better disease control [13,14].
Limitation
The effective sample size is small, mainly because of the high rate of loss to follow up, which we found to be mostly due to pragmatic errors of not being able to communicate with patients via telephone and patient unwillingness to travel long distances. The study being conducted in a tertiary care center which is depended upon by almost the whole of north India might have contributed to this. The level of education given by the three instructors might vary, as might the patient’s reception to education regarding MDI technique. In spite of these shortcomings, this study gave useful information regarding defects in MDI use in a busy OPD setting and also regarding ways to correct them. This study uses the MDI with spacer as advised in the latest guidelines. The study also assessed the reason for loss to follow up, and also checked the physician’s practices related to MDI in brief.
Conclusion
There was high prevalence of incorrect MDI use and false assurance about the correctness of use among patients. Errors in MDI use technique improved significantly after imparting systematic educational intervention and practical demonstration of all steps using a standardized checklist. Re-evaluation and repeat demonstration of MDI use technique is advisable on every follow up visit. Existing medical options for chronic respiratory patients should be used optimally through patient education based on practical demonstration.