Jategaonkar’s Modification of Brooke’s End-Ileostomy
Priyadarshan Anand Jategaonkar1, Smita Priyadarshan Jategaonkar2, Sudeep Pradeep Yadav3
1 Professor, Department of General Surgery, Mahatma Gandhi Institute of Medical Sciences, Wardha, Maharashtra, India.
2 Assistant Professor, Department of Pediatrics, Mahatma Gandhi Institute of Medical Sciences, Wardha, Maharashtra, India.
3 Senior Resident, Department of Plastic and Reconstructive Surgery, Grant’s Government Medical College & Sir J.J. Group of Hospitals, Mumbai, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Priyadarshan Anand Jategaonkar, E-4, Senior Staff Quarter, MGIMS, Medical Square, Sewagram-442102, Wardha, Maharashtra, India.
E-mail: jategaonkarpa@gmail.com
Ileostomy, Surgery, Stoma, Modification
Sir,
Since its inception in the year 1952, Brooke’s ileostomy has remained a standardised and widely practiced method of faecal diversion [1]. However, despite all the precautions, as high as 76% ileostomies develop long-term morbid complications (skin excoriation being significantly common) which adversely affect the quality of life of these individuals [2,3]. At times, this may even necessitate stoma relocation [4]. Thus, for improvised outcomes, some efficient and robust modification in the hitherto-used technique seems the need of the hour. In that context, we propose some modifications in the conventional Brooke’s end-ileostomy.
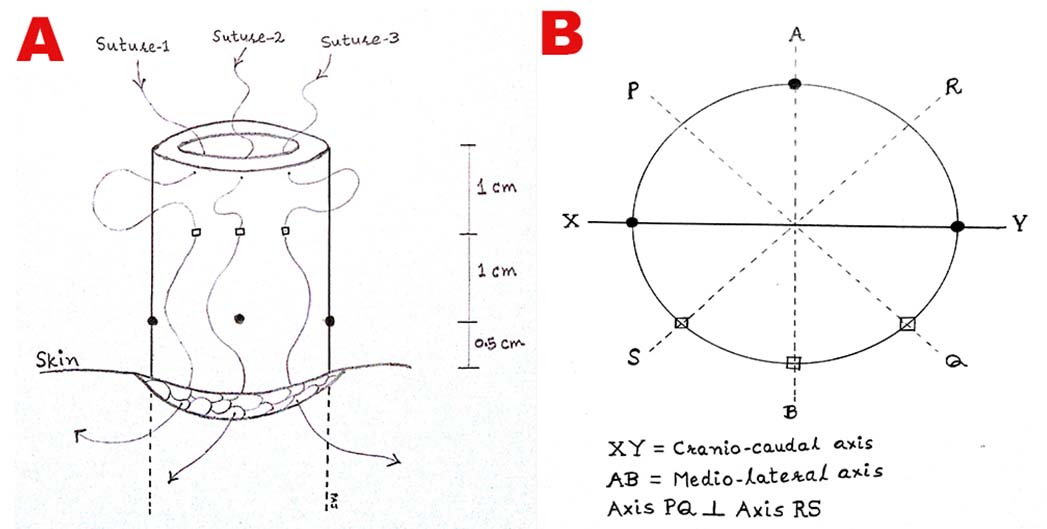
While the initial steps remain the same, our technique commences at maturing the ileostomy per-operatively. Herein, three 3/O absorbable sutures are passed sequentially through the lateral cut-edge of the ileum (full-thickness), the corresponding ileal wall (sero-muscular, 1 cm proximal to the cut-margin) and then via subcuticular tissue of the stoma incision. Remaining sutures remain as for the standard Brooke’s ileostomy [Table/Fig-1]. Once tied, these sutures evert the bowel wall around its circumference in a peculiar fashion to achieve lateral bowing of the stoma [Table/Fig-2]. Now, the external stoma device may be secured as usual.
Schematic representation of constructing Jategaonkar’s modified end-ileostomy: (a) Suture-pathways. Note that, in modified approach, the sero-muscular bytes (□) are taken half-way between the cut-margin of the bowel and the conventional byte-points (•) in order to accomplish an outwardly angulated spigot; (b) Geometry of the circumferential bytes. Note that the modified bytes (□) are segregated in the lateral 45 degrees and the conventional bytes (•) are spread over the remaining 315 degrees of the bowel circumference; this minimises the peristomal skin area amenable to excoriation.
Final appearance of modified ileostomy. Note that, the direction of the effluent ejection from the traditional ileostomy (vertical white arrow) differs largely from that of the modified ileostomy (horizontal white arrow). The projectile (upper oblique arrow) and the non-projectile (lower oblique arrow) intestinal effluents produce a resultant horizontal vector that leads to effective drainage of the stoma-output; 2) Stoma at post-operative day-7. Note that the typical “stooping” nature of the ileostomy keeps the surrounding skin totally free of chemical dermatitis. And, the flange-imprint of the stoma appliance denotes complete dryness of the peristomal skin. Further note that, the healthy stoma indicates preserved vascularity post modified bytes.

Our technique has several advantages: 1) It ensures effective drainage of projectile as well as non-projectile components of typically voluminous enteric effluent, thereby keeping the peristomal skin free of chemical excoriation, especially in early post-operative period when patient remains mostly bedridden; 2) It avoids under-seepage of enteral contents, thereby dislodgement of stoma appliance that could lead to further leakage and multiple bag exchanges; 3) On long run, it is potentially cost-effective; this is particularly crucial for resource-limited countries; 4) Unlike traditional stoma, its non-dependant bowing configuration tends to prevent mucosal prolapsed; 5) Its simple to learn even by the junior-most member of surgical team; the learning curve for our postgraduates is just 3 cases; 6) It continues to maintain these benefits even when patient is fully ambulatory; 7) It may be similarly employed in emergency settings; 8) It is a fail-safe method for ill-fitting devices; 9) It could be favourably implemented in obese individuals; 10) It can be applied to colostomies as well as loop ileostomies; 11) Overall, it likely improves patient’s self-image, removes social stigma and enhances quality of life. We have used this method in 110 cases without any complications. It has received encouraging positive feedback from stoma-nurses and therapists locally. Therefore, we recommend it for regular use.
[1]. Marsh P, Clark JS, The spouted colostomyAnn R Coll Surg. Engl 2007 89(1):7810.1308/rcsann.2007.89.1.78PMC1963527 [Google Scholar] [CrossRef] [PubMed]
[2]. Jayarajah U, Samarasekara AM, Samarasekera DN, A study of long-term complications associated with enteral ostomy and their contributory factorsBMC Res Notes 2016 9(1):50010.1186/s13104-016-2304-z27919277 [Google Scholar] [CrossRef] [PubMed]
[3]. Schiergens TS, Hoffmann V, Schobel TN, Englert GH, Kreis ME, Thasler WE, Long-term quality of life of patients with permanent end ileostomy: results of a nationwide cross-sectional surveyDis Colon Rectum 2017 60(1):51-60.10.1097/DCR.000000000000073227926557 [Google Scholar] [CrossRef] [PubMed]
[4]. Dodd BR, Mccallion K, Iieostomy efferent limb prolapse: a temporising measureAnn R Coll Surg Engl 2007 89(5):534-35.10.1308/rcsann.2007.89.5.53418170935 [Google Scholar] [CrossRef] [PubMed]