Retroperitoneal Multicystic Mesothelioma in a Young Male
Anshul Singh1, Mamta Bhatt2, Preeti Singh3, Vatsala Misra4
1 Assistant Professor, Department of Pathology, MLN Medical College, Allahabad, Uttar Pradesh, India.
2 Resident, Department of Pathology, MLN Medical College, Allahabad, Uttar Pradesh, India.
3 Resident, Department of Pathology, MLN Medical College, Allahabad, Uttar Pradesh, India.
4 Professor and Head, Department of Pathology, MLN Medical College, Allahabad, Uttar Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Mamta Bhatt, Girls Hostel, MLN Medical College, Allahabad, Uttar Pradesh, India.
E-mail: bhatt.mamtadr88@gmail.com
Multicystic Peritoneal Mesotheliomas (MPMs) are rare tumours characterised by recurrent mesothelial inclusion cysts. Less than 200 cases have been reported worldwide. Only 10 cases have been reported from India. Though they have strong predilection for peritoneum of the pelvic and abdominal organs, few cases have been reported in extraperitoneum and retroperitoneum too. MPMs are mainly a tumour of females of reproductive age group who have had some abdominopelvic pathology/surgery. Very few cases have been reported in men, mostly in the middle to elderly age group and like their female counterparts, associated with a history of some past abdominopelvic pathology/surgery. Only one case has been reported in a young male in the literature till date. We document here a case of multicystic mesothelioma presenting in an 18-year-old young male in the retroperitoneum who had no such significant past history.
Cysts, Intraabdominal, Benign
Case Report
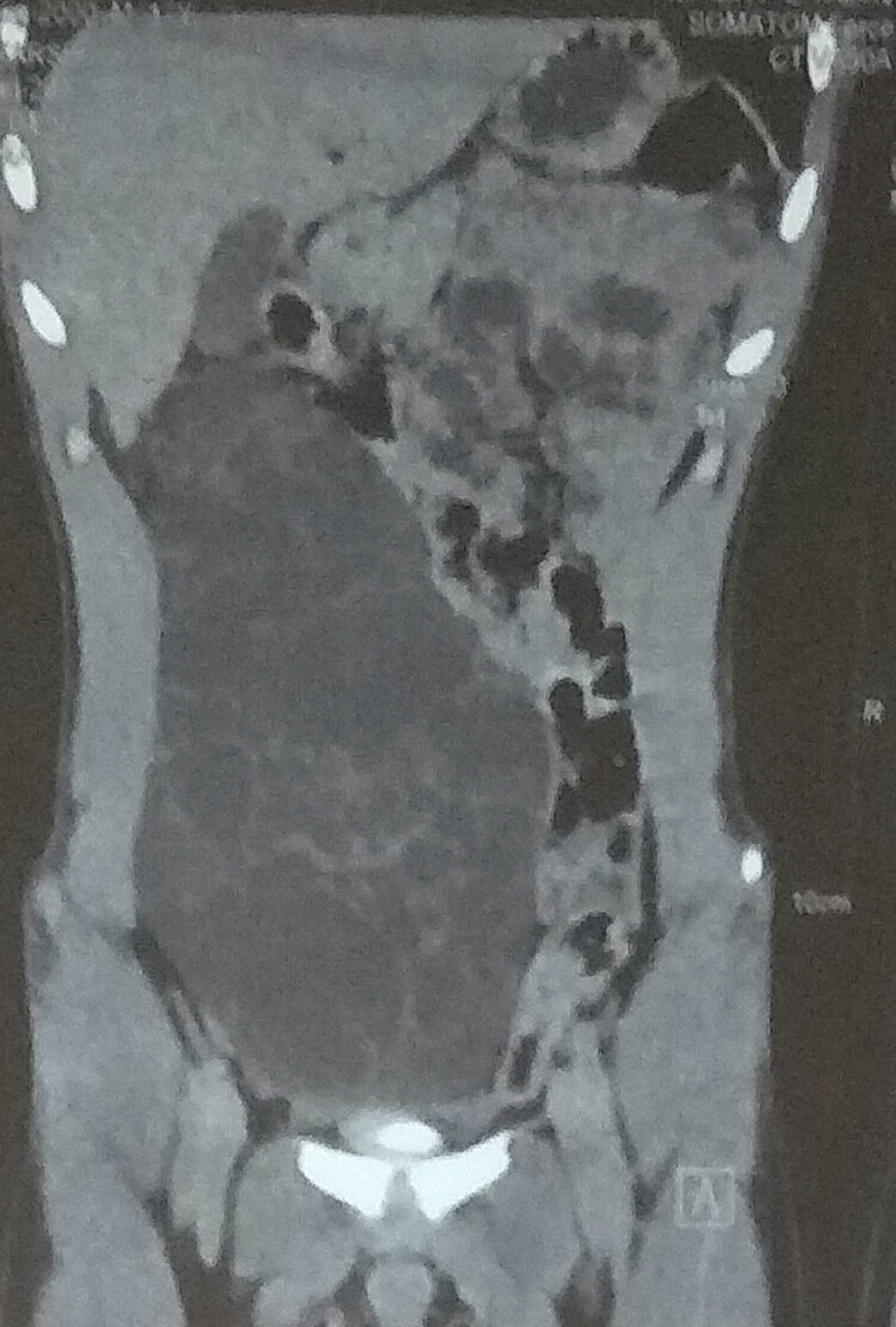
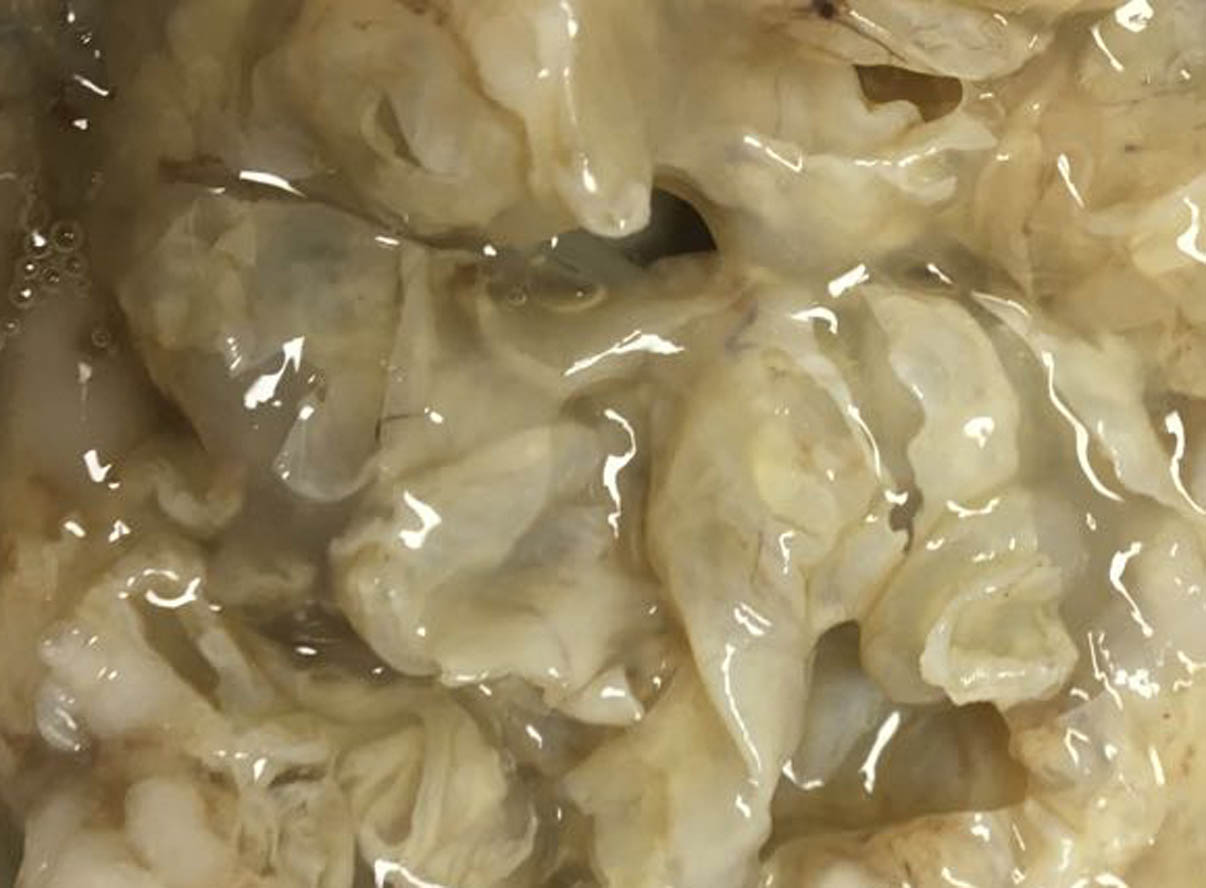
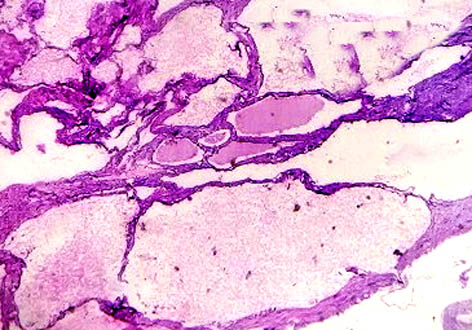
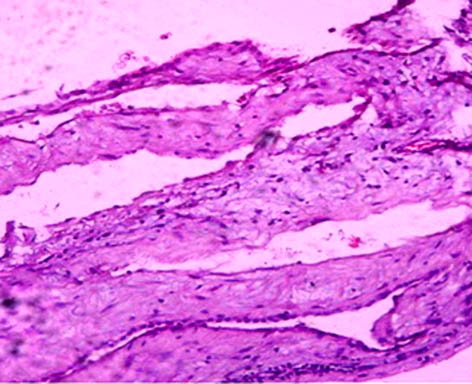
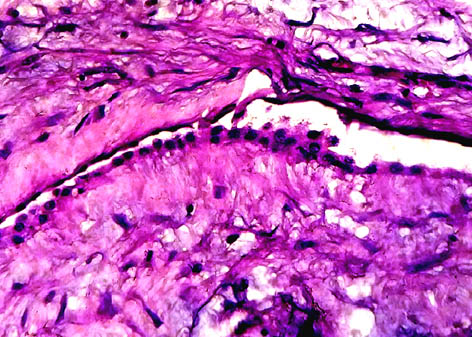
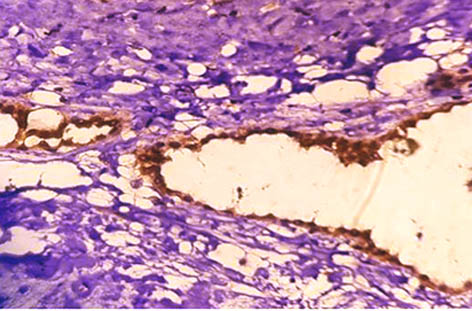
An 18-year-old male presented with complaint of gradually progressive swelling in abdomen since 1 year. His physical parameters and routine haematological investigations were within normal limits. There was no history of past abdominal surgery. CECT revealed a large well-defined multiseptated cystic lesion in the right side of the abdomen extending from the sub-hepatic region to the pelvis, displacing the bowel loops to the left side as well as partially compressing the urinary bladder but with no internal calcifications. The impression given was that of a cystic retroperitoneal neoplasm with internal septations and the differentials suggested were Cystadenoma and Lymphangioma [Table/Fig-1]. The patient underwent surgical excision of the mass. On gross examination, a single, globular, cystic, grey white, soft piece of tissue was received, measuring 20 x 12 x 6 cm. On cutting, 300 ml of clear fluid came out. Cut surface showed multiloculations throughout the specimen. No solid areas were seen [Table/Fig-2]. Multiple sections from various areas were taken and submitted for processing. Histopathological examination showed multiple cystic areas of variable size filled with proteinaceous fluid and lined by a continuous epithelium which was predominanlty cuboidal to low columnar and flat at few foci. Intervening stroma was fibrous with few congested blood vessels and chronic inflammation. No atypia was seen. The histological findings were consistent with a Benign Multicystic Pathology [Table/Fig-3,4 and 5]. IHC for Calretinin and CD 31 was done and calretinin turned out to be positive [Table/Fig-6]. Hence, the diagnosis of Multicystic Mesothelioma was given. The patient has been kept on regular follow-up and was doing fine till the time of writing this paper.
CECT showing a well-defined multiseptated cystic lesion in right side of abdomen with displacement of bowel loops.
Gross examination showing a single globular piece of tissue with multiloculations.
Scanner view showing multiple proteinaceous fluid-filled spaces lined by epithelium (4X H&E).
Low power view showing cystic spaces lined by flat to cuboidal epithelium (10X H&E).
High power view showing a cystic space lined by cuboidal epithelium (40X H&E).
Immunohistochemistry showing positive staining for Calretinin in the lining epithelial cells (40X IHC).
Discussion
MPM is a rare intra-abdominal tumour with a strong predilection for the peritoneum of pelvic and abdominal organs but can also involve extraperitoneal space and omentum [1]. MPM was first described in 1928 by Plaut, who during an operation for uterine leiomyoma, incidentally observed loose pelvic cysts, the mesothelial origin of which was confirmed later [2]. The first paper was published by Mennemeyer and Smith in 1979 [3]. Since then, less than 200 cases have been reported worldwide with only around 10 cases reported from India [4]. MPMs are characterised by recurrent peritoneal mesothelial inclusion cysts occurring predominantly in young females, with very few studies reporting in men [2,5-7]. Rare cases have also been reported in children as well as in extra-abdominal sites [8]. Peritoneal mesotheliomas are classified into three subtypes: Malignant, Cystic and well-differentiated Papillary Mesothelioma, wherein cystic mesotheliomas which are generally referred to as benign have potential for locoregional invasion, as well as distant nodal and serosal metastases, hence, the term “benign” should be used with caution [9]. If symptomatic, the classic presenting features are abdominal or pelvic mass, abdominal pain, and tenderness. But in most cases, MPM remains silent in abdominal cavity and more rarely, the retroperitoneum. Sometimes, it can manifest as acute abdomen [8].
The pathogenesis of MPM is controversial with some studies suggesting it to be a neoplastic lesion due to its tendency to recur after surgical resection, some others believing it to be a reactive process to underlying chronic inflammation and some suggesting a hormonal involvement due to the response shown to hormonal therapy [10].
The tumour has a female preponderance, with a female:male ratio of 5:1, with most patients having a history of a previous abdominopelvic operation, endometriosis or pelvic inflammatory disease. In females, the majority of cases have been reported in those who were in reproductive age group [1,4,8-10]. There are a few reports of the disease diagnosed in men, mostly middle-aged to elderly [2,5,6], but apart from our case , there is only one case reported in the literature where it was diagnosed in a 19-year-old male [7]. Cases in children as well as in rare extra-abdominal locations such as spermatic cord, tunica vaginalis and rectus sheath have also been reported [1,8].
Diagnosis of cystic peritoneal mesothelioma is challenging. Lesions can be demonstrated by ultrasonography, CT and MRI but they cannot differentiate them from other cystic lesions. Fine needle aspiration of the lesion is also not absolutely diagnostic, with the features being mimicked by several other conditions. To add to this pathos, there are no specific tumour markers [10].
Exploratory laparoscopy with histopatholgical examination is said to be the most accurate method of diagnosing. Differential diagnosis includes a number of lesions, with cystic lymphangioma being the closest differential in a young male [8]. In our case also, cystic lymphangioma was suspected on radiology. However, in cystic lymphangioma, the fluid is chylous and on microscopy, flattened endothelial cells in single layer line the cystic space, are immunoreactive to vascular markers (CD31, CD34, factor VIII, and VEGFR3) and also show smooth muscle and lymphoid aggregates present in their walls [8,10].
There are no evidence-based treatment strategies for cystic peritoneal mesothelioma. Though mostly MPMs have an excellent prognosis, an aggressive surgical approach including cytoreductive surgery with peritonectomy is recommended because of the few cases where malignant transformation of this tumour has been reported [9].
However, the recurrence rate of BMPM remains high, more so in females, even after complete cytoreduction. For surveillance, some authors suggest repeating CT scan every 3 months for the first year after resection and then annually for the next 5 years, which may result in early detection of relapse. However, the impact of this strategy on overall survival is not yet established [5].
Conclusion
MPM is an unusual lesion, the diagnosis of which is challenging because of the absence of specific imaging features, tumour markers and definitive cytology. Histopathology with a supporting role of immunohistochemistry is the only way of establishing a definitive diagnosis. Though most of the cases have been reported in females, few cases have been reported in males, mostly of elderly age and with a prior history of some kind of abdominal surgery. Only one case has been reported in a young totally asymptomatic male apart from this case. Hence, we would like to suggest that even in young males with a non-significant past history, a high index of suspicion for cystic mesotheliomas should be kept while reporting multicystic tumours. Unfortunately, there are no established protocols of management. Even though its prognosis is quite good, long-term follow-up is mandatory due to high incidence of recurrence and occasional episodes of malignant transformation reported.
[1]. Debnath S, Misra V, Singh PA, Singh M, Low grade cystic mesothelioma of rectus sheathJCDR 2007 1:173-76. [Google Scholar]
[2]. Soon DSC, Shilton H, Andrabi A, Mesothelial inclusion cyst: a rare occurrenceJ Surg Case Rep 2016 2016(12):rjw21310.1093/jscr/rjw21327994008 [Google Scholar] [CrossRef] [PubMed]
[3]. Mennemeyer R, Smith M, Multicystic, peritoneal mesothelioma: a report with electron microscopy of a case mimicking intra-abdominal cystic hygroma (lymphangioma)Cancer 1979 44:692-98.10.1002/1097-0142(197908)44:2<692::AID-CNCR2820440242>3.0.CO;2-6 [Google Scholar] [CrossRef]
[4]. Gupta A, Rao HK, Pande R, Gupta S, A rare case of benign multicystic peritoneal mesothelioma: a clinical dilemmaIndian J Surg 2013 75:27-29.10.1007/s12262-011-0314-624426503 [Google Scholar] [CrossRef] [PubMed]
[5]. Khurram MS, Shaikh H, Khan U, Edens J, Ibrar W, Hamza A, Benign multicystic peritoneal mesothelioma: a rare condition in an uncommon genderCase Rep Pathol 2017 2017:975290810.1155/2017/975290828607791 [Google Scholar] [CrossRef] [PubMed]
[6]. Somasundaram S, Khajanchi M, Vaja T, Jajoo B, Dey AK, Benign multicystic peritoneal mesothelioma: a rare tumour of the abdomenCase Reports in Surgery 2015 2015:61314810.1155/2015/61314825866695 [Google Scholar] [CrossRef] [PubMed]
[7]. Khuri S, Gilshtein H, Abboud W, Assalia A, Kluger Y, Benign cystic mesothelioma of the peritoneum: a rare case and review of the literatureCase Rep Oncol 2012 5:667-70.10.1159/00034618723341809 [Google Scholar] [CrossRef] [PubMed]
[8]. Safioleas MC, Constantinos K, Michael S, Konstantinos G, Constantinos S, Alkiviadis K, Benign multicystic peritoneal mesothelioma: A case report and review of the literatureWorld J Gastroenterol 2006 12:5739-42.10.3748/wjg.v12.i35.573917007034 [Google Scholar] [CrossRef] [PubMed]
[9]. Singh A, Chatterjee P, Pai MC, Chacko RT, Multicystic peritoneal mesothelioma: not always a benign diseaseSingapore Med J 2013 54:e76-e78.10.11622/smedj.201308523624458 [Google Scholar] [CrossRef] [PubMed]
[10]. Tagore KR, Kumar RSA, Bhavani N, Ramachander S, A case of multicystic peritoneal mesotheliomaAnn Nigerian Med 2012 6:41-43.10.4103/0331-3131.100223 [Google Scholar] [CrossRef]