Vitamin D refers to group of fat soluble secosteroids which is essential for calcium homeostasis, bone maturation and mineralisation [1].
Vitamin D inadequacy and deficiency is a common global problem and their prevalence is high even in developed countries. Particularly pregnant women are considered as a high-risk group with global reports citing that 20-80% of pregnant women may suffer from vitamin D inadequacy and deficiency. There are evidences suggesting that vitamin D-deficient women are at increased risk of gestational diabetes mellitus, bacterial vaginosis and higher rate of caesarean sections which will have potentially adverse effects on the neonate. Hypovitaminosis D in the mother may have important immediate and long-term implications for offspring. Prematurity, low birth weight, low bone density as well as later sequelae such as higher rates of lower respiratory tract infection, asthma, diabetes mellitus, autism and dental problems, are examples of post-neonatal outcomes known to be related to vitamin D deficiency in pregnancy [2-10].
The prevalence of vitamin D deficiency in India is about 70% to 100%. This is unusual in a tropical country like India, where there is abundant sun shine. Cultural and social taboos such as lifestyle patterns such as clothing that may limit sun exposure and vegetarianism which limits vitamin D rich diet, may be the reasons for the prevalence [11,12].
India constitutes a large population of socioeconomically backward people. There is social, environmental, educational difference among the people with different socioeconomic status. These factors are closely linked with the nutrition of that population. Hence the underprivileged usually suffer from overall poor nutrition [11].
This study was done in coastal region of southern India, where sunlight is abundant. There are no studies found in literature which estimate the levels of vitamin D in the mother and her baby in coastal area and also there were limited studies on correlation with respect to their socioeconomic status. Hence, this study was conducted with an aim to study the level of vitamin D in maternal and their newborn in relation to their socioeconomic status in coastal Karnataka.
Materials and Methods
It was a hospital based cross-sectional study done at Government referral hospital, Mangalore and Kasturba Medical College Hospital, Mangalore, Karnataka, India. Study period was for two years (October 2015 to September 2017). Taking prevalence of 15% relative precision, 85% power and 95% confidence level, the sample size was calculated to be 71. Adding 10% as non-responsive a sample size of 80 was determined. Thus sample size was 80 mothers and their newborn. Institutional Ethical Committee clearance was obtained and an informed consent was taken from the participants. They were divided into two groups of 40 each based on their socioeconomic status as Low Socioeconomic Status (LSES) and High Socioeconomic Status (HSES). All pregnant women who were antenatal booked cases at government hospitals have received only calcium supplements (500 mg) and antenatal booked cases from private clinics have received calcium tablets (500 mg) along with 200 IU of vitamin D and we also had mothers without antenatal check-ups who have not received supplements.
Inclusion criteria: All pregnant women delivered by normal vaginal delivery and elective LSCS.
Exclusion criteria: Multiple pregnancy, mother with bronchial asthma and allergic disorders, endocrine disorders like thyroid, parathyroid and diabetes, eclampsia and pre-eclampsia, auto immune disorders, kidney disorders, pregnancy after 35 years, placenta previa, abruptio-placenta, preterm and mothers on drugs like, phenytoin, phenobarbital and glucocorticoid.
The estimation of vitamin D was done after a batch of 160 samples using ELISA kit. Vitamin D levels were defined as per US Endocrine Society classification [13] [Table/Fig-1].
Vitamin D status according to US endocrine society [13].
| Vitamin D status | 25(OH) D Levels |
|---|
| Deficiency | <20 ng/mL |
| Insufficiency | <21-29 ng/mL |
| Sufficiency | >30 ng/mL |
| Toxicity | >150 ng/mL′ |
Socioeconomic status: The socioeconomic status of the mother was assessed using modified kuppuswamy scale [14]. For our study purpose, we had clubbed upper class and upper middle class as HSES and lower middle class and upper lower class as LSES.
Sample Collection: About 2 mL of blood sample had been collected from each mother during cannulation and 2 mL cord blood of newborn was collected under aseptic conditions during labour in vacutainers. The serum was extracted and stored in lab at -20° centigrade. Vitamin D levels were estimated by ELISA method which is an in-vitro determination of 25 hydroxy vitamin D levels in serum.
Statistical Analysis
Results were assessed using SPSS version 17.0. Results were derived using Student’s paired t-test, chi-square/Fishers test and Pearsons correlation. A p-value of <0.05 was considered significant.
Results
Among the 40 participants in LSES group 92.5% were of lower middle class, 7.5% were of upper lower class and in 40 participants in HSES group 5.0% were of upper class and 95% are from upper middle class [Table/Fig-2].
Demographic variables of the study population (n=80).
| Variables | Categories | LSES Group | HSES Group |
|---|
| n (%) | n (%) |
|---|
| Age of mother | < 24 | 14 (35.0) | 4 (10.0) |
| 25-30 | 18 (45.0) | 28 (70.0) |
| 31-35 | 8 (20.0) | 8 (20.0) |
| Total | 40 (100.0) | 40 (100.0) |
| Obstetric details | Multi | 29 (72.5) | 19 (47.5) |
| Primi | 11 (27.5) | 21 (52.5) |
| Total | 40 (100.0) | 40 (100.0) |
| Supplements | N | 18 (45.0) | 0 (0.0) |
| P | 13 (32.5) | 5 (12.5) |
| Y | 9 (22.5) | 35 (87.5) |
| Total | 40 (100.0) | 40 (100.0) |
| SES | UC | 0 (0.0) | 2 (5.0) |
| UMC | 0 (0.0) | 38 (95.0) |
| LMC | 37 (92.5) | 0 (0.0) |
| ULC | 3 (7.5) | 0 (0.0) |
| Total | 40 (100.0) | 40 (100.0) |
| Mode of delivery | LSCS | 11 (27.5) | 6 (15.0) |
| NVD | 29 (72.5) | 34 (85.0) |
| Total | 40 (100.0) | 40 (100.0) |
*N: No supplementation; P: Partial supplementation; Y: Complete supplementation during pregnancy
Vitamin D deficiency was observed in 41.3% (33) of the mother and 70% (56) of the newborn, insufficiency in 33.8% (27) of the mothers and 22.5% (18) of the newborn and normal level of vitamin D in 25% (20) of the mother and 7.5% (6) of the baby.
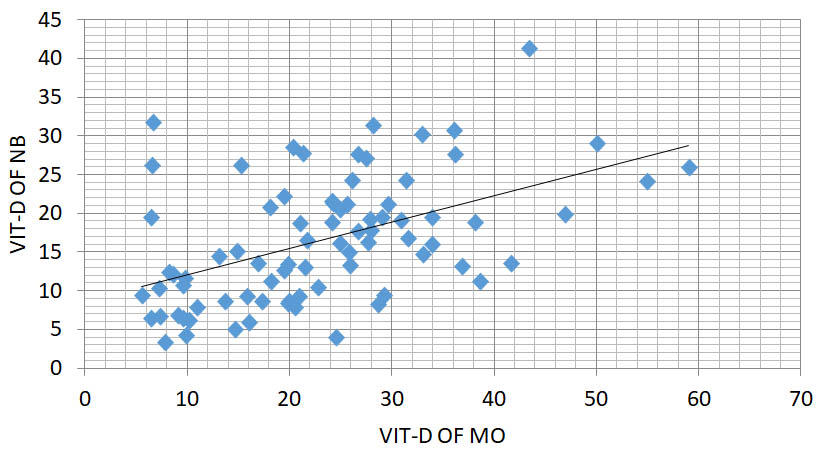
There was a strong positive correlation between the vitamin D levels in maternal and cord blood (r=0.492; p<0.001) [Table/Fig-3].
Correlation of vitamin D levels of mother and child.
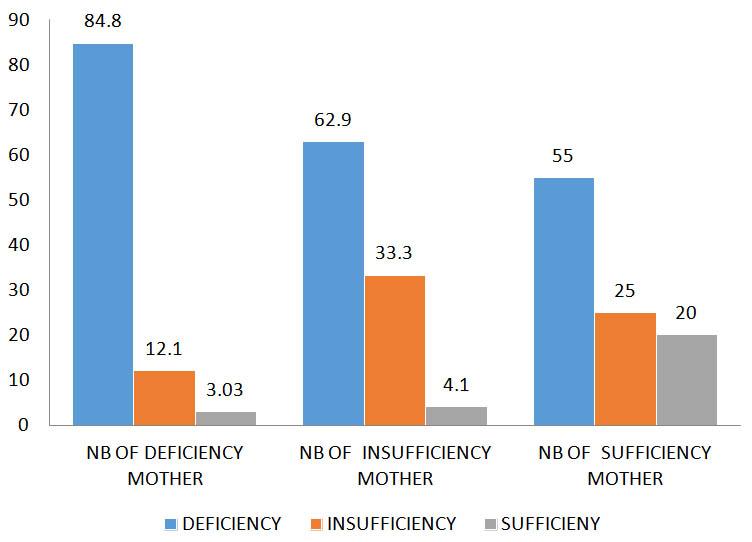
Out of 80 subjects, 33 mothers had vitamin D deficiency of which 84.84% of newborns had vitamin D deficiency 12.1% of newborns had vitamin D insufficiency and 3.03% of newborns had vitamin D sufficiency, 27 mothers had vitamin D insufficiency of which 62.9% of newborns had vitamin D deficiency 33.3% of newborns had vitamin D insufficiency and 4.1% of newborns had vitamin D sufficiency and 20 mothers had vitamin D sufficiency of which 55% of newborns had vitamin D deficiency 25% of newborns had vitamin D insufficiency and 20% of newborns had vitamin D sufficiency [Table/Fig-4].
Vitamin D status of mother according to new-born vitamin D levels.
In the present study, it was found that age of the mother, obstetric details and mode of delivery had no significant correlation with the vitamin D levels of mother. The supplements taken by the mother during pregnancy (p<0.001) and socioeconomic status of the mother (p<0.001) had high statistically significant effect on vitamin D levels of mother. There was a statistically significant (p=0.033) correlation of vitamin D levels of mother on their newborn [Table/Fig-5].
Correlation of vitamin D levels of mother with various demographic variants using Chi-Square tests.
| Demographic variants | DeficiencyCount % | InsufficiencyCount % | SufficiencyCount % | Chi-square value |
|---|
| Age of mother (years) | <24 | 11 | 61.1% | 3 | 16.7% | 4 | 22.2% | 0.335 |
| 25-30 | 17 | 37.0% | 17 | 37.0% | 12 | 26.1% |
| 31-35 | 5 | 31.3% | 7 | 43.8% | 4 | 25.0% |
| Total | 33 | 41.3% | 27 | 33.8% | 20 | 25.0% |
| Obstetric details | Multi | 23 | 47.9% | 17 | 35.4% | 8 | 16.7% | 0.094 |
| Primi | 10 | 31.3% | 10 | 31.3% | 12 | 37.5% |
| Total | 33 | 41.3% | 27 | 33.8% | 20 | 25.0% |
| Supplements | N | 18 | 100.0% | 0 | 0.0% | 0 | 0.0% | <0.001 (HS) |
| P | 12 | 66.7% | 4 | 22.2% | 2 | 11.1% |
| Y | 3 | 6.8% | 23 | 52.3% | 18 | 40.9% |
| Total | 33 | 41.3% | 27 | 33.8% | 20 | 25.0% |
| SES | HSES | 5 | 12.5% | 18 | 45% | 17 | 42.5% | <0.001(HS) |
| LSES | 28 | 70% | 9 | 22.5% | 3 | 7.5% |
| Total | 33 | 41.25% | 27 | 33.75 | 20 | 25.0% |
| MOD | LSCS | 9 | 52.9% | 7 | 41.2% | 1 | 5.9% | 0.121 |
| NVD | 24 | 38.1% | 20 | 31.7% | 19 | 30.2% |
| Total | 33 | 41.3% | 27 | 33.8% | 20 | 25.0% |
| VIT-D OF NB | Deficiency | 28 | 50.0% | 17 | 30.4% | 11 | 19.6% | 0.033(SIG) |
| Insufficiency | 4 | 22.2% | 9 | 50.0% | 5 | 27.8% |
| Suffi-ciency | 1 | 16.7% | 1 | 16.7% | 4 | 66.7% |
*N: No supplementation; P: Partial supplementation; Y: Complete supplementation during pregnancy
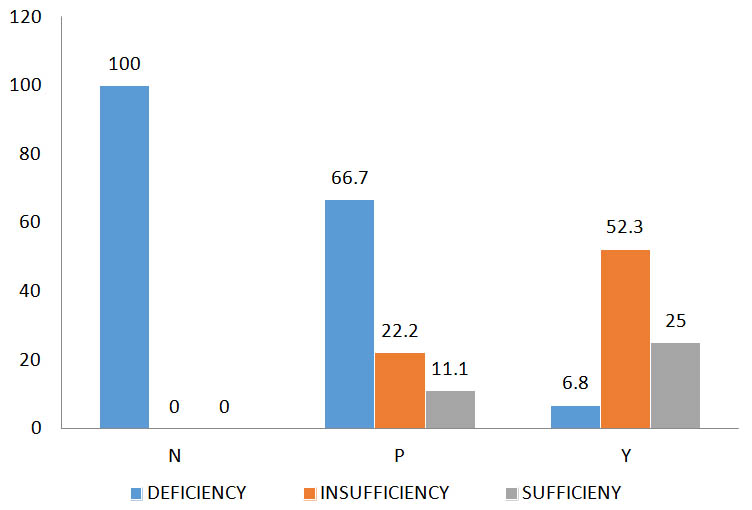
Out of 80 subjects, 18 mothers had not taken any supplement that is all the mother (100%) had deficiency, 18 mothers had taken only partial supplements of which 66.7% had deficiency, 22.2% had insufficiency and 11.1% had sufficient vitamin D levels and 44 mothers had taken complete supplementation of which 6.8% had deficiency, 52.3% had insufficiency and 25% had sufficient vitamin D levels [Table/Fig-6].
Vitamin D status of mother according to supplementation.
The mean value of vitamin D levels in mother with complete supplementation were 30.584, with partial supplementation were 18.706 and without supplementation were 9.067. The p-value is <0.001 which is highly significant. Supplementation helps in improving the vitamin D levels in the mothers [Table/Fig-7].
Mean value of vitamin D of mother based on supplements taken.
| Supplements | N | Mean | Std. deviation | 95% Confidence Interval for Mean | ANOVA F | p-value |
|---|
| Lower Bound | Upper Bound |
|---|
| Yes | 44 | 30.584 | 9.3540 | 27.740 | 33.428 | 54.976 | <0.001HS |
| Partial | 18 | 18.706 | 5.4691 | 15.986 | 21.425 |
| No | 18 | 9.067 | 3.2617 | 7.445 | 10.689 |
| Total | 80 | 23.070 | 11.6969 | 20.467 | 25.673 |
Discussion
The finding in present study indicates that vitamin D deficiency was observed in 41.3% (33) of the mother and 70% (56) of the newborn, insufficiency in 33.8% (27) of the mothers and 22.5% (18) of the new born and normal level of vitamin D in 25% (20) of the mother and 7.5% (6) of the baby.
Kamal S et al., in their study done at Jharkhand observed the prevalence of maternal hypovitaminosis D to be 77.9% and neonatal hypovitaminosis D to be 83.1% [15]. Also, in the study done by Sachan A et al., it was noted that 84% of mother and 95.7% newborn were deficient of vitamin D where the deficiency of vitamin D value was taken as 22.5 ng/mL [16]. If we relate this value to present study, the total mothers with deficiency has been noted to be 75% and deficiency among newborn to be 92.7%, which is similar to our study. These studies indicate that the prevalence of vitamin D deficiency is very high among pregnant women in India.
In studies done by Sachan A et al., Kumar P et al., and Sharma S et al., It was seen that the maternal vitamin D levels correlate with vitamin D of cord blood [16-18]. This was also well documented internationally; studies done in countries like Greece and Egypt also reported that there is a statistically significant correlation between mother cord vitamin D levels [19,20]. The same was noted in present study where the correlation of maternal vitamin D of mother with their newborn was (r=0.49, p=0.01), which is statistically significant. This indicates that the vitamin D levels of mother during pregnancy had a significant effect on vitamin D of newborn.
Further in present study we had studied the values of vitamin D deficiency in mother and their newborn of different socioeconomic status to find out its effects on vitamin D deficiency and found to be statistically significant, p<0.001. We observed vitamin D deficiency in 70% (28) of mothers and 77.5% (31) newborns in LSES group and 12.5% (5) of mothers and 62.5% (25) in newborn in HSES which indicates the prevalence of vitamin D deficiency is more prevalent in LSES than HSES group, which is in concurrence with studies done by Sharma S et al., and Satish P et al., [18,21]. They also observed similar vitamin D deficiency among low socioeconomic pregnant women and their newborn and was found to be statistically significant, p=0.0001 and p=0.000 respectively. This difference can be attributed to the socioeconomic status, difference in education of the parent, dietary habits, environmental factors and cost of vitamin D supplements and fortified foods.
In India, fortification of food with vitamin D is uncommon. The fortification of food with vitamin D is only partially effective even in developed countries like USA and Canada. Unfortunately, there is very less awareness on the need of vitamin D supplements among Indians and also the cost of these fortified foods and supplements is prohibitive.
Calcium and vitamin D supplementation in the mother had statistical significance on maternal vitamin D status (p<0.001). We observed even though 55% (44) of pregnant mothers took regular supplementation of calcium, only 40% of the mother had normal vitamin D level and vitamin D deficiency was found in 6.8% and insufficiency was found in 52.3%. This was probably due to the calcium tablet provided to the mother by healthcare providers, sometime had only 500 mg of elemental calcium and sometime received 500 mg of elemental calcium with 200 IU of vitamin D3 which is significantly lesser compared to recommended dose (recommended dose 1.5-2.0 gm of elemental calcium [22] and vitamin D 600 IU [23]. Similar to present study, study done by Maghbooli Z et al., found vitamin D deficiency among mothers who were on supplemental calcium and vitamin. However, dose of supplements was not mentioned [24]. Hossain N et al., in his Randomised Control Trail done at Karachi compared between routine supplementation of vitamin D and higher dose of vitamin D during pregnancy and results showed that neonatal 25(OH)D levels were significantly higher in those received high dose vitamin D compared to normal supplementation and there was positive correlation between maternal and neonatal 25(OH)D levels (r=0.83, p=0.001) [25]. This suggests that adequate vitamin D supplementation will have positive impact on mothers and newborn baby’s vitamin D status.
Limitation
The study included only 80 mothers, however larger study group over longer period will give a better picture. There was no uniformity in vitamin D supplementation among the mother.
Conclusion
Vitamin D is essential for calcium homeostasis, bone maturation and mineralisation. Hypovitaminosis D in the mother has important immediate and long-term implications on both mother and her offspring. Maternal vitamin D levels have positive correlation with vitamin D levels of newborn. Adequate vitamin D supplements in the mother have a positive correlation with vitamin D levels in both mother and newborn. LSES of the mother has negative impact on vitamin D levels of both mother and newborn. Adequate vitamin D supplements for all pregnant mothers are recommended for achieving healthy mother and a healthy baby.
*N: No supplementation; P: Partial supplementation; Y: Complete supplementation during pregnancy
*N: No supplementation; P: Partial supplementation; Y: Complete supplementation during pregnancy