There is an increased prevalence of heart disease has been found in pregnant women, due to increase age at first pregnancy, increasing the prevalence of diabetes, hypertension, obesity and also due to marked improvement in the treatment of congenital heart disease. [1-3]. Prevalence of heart disease in pregnancy is found to vary between 0.3-3.5% [4]. Heart diseases are now the leading cause of indirect maternal deaths accounting for 20.5% of all cases [5,6].
In western world, congenital heart disease is most common (75% to 82%) with shunt lesions predominating in around 20% to 65% [2]. In developing countries like India, RHDs, despite its declining trend still accounts for majority of such cases comprising 56% to 89% of all cardiovascular disease in pregnancy [2]. Congenital heart disease which comprised only 5% of pregnant women with heart disease in the past, now majority of the pregnant women with heart disease are having congenital heart disease in developed world [7,8].
In pregnancies complicated with cardiac disorders, maternal and perinatal mortality and morbidity depends on the type of disorder, the functional status of the patient and the complications associated with the pregnancy [9,10]. Maternal morbidity includes chances of cardiac failure, pulmonary oedema, shock (cardiogenic), arrhythmia, thromboembolism and even maternal mortality. Perinatal outcome includes low birth weight baby, intrauterine growth retardation, preterm birth and foetal congenital heart disease etc.
There are no studies done in the Northeastern India on pregnancy associated with cardiac disease, inspite of the increasing number of the same. Hence the current study is designed to provide an insight into the changing patterns and outcome of this ever increasing and life threatening condition at a tertiary care centre of Northeastern India with an aim to find out prevalence, spectrum of disorder and outcome in pregnancy with heart disease.
Materials and Methods
This prospective, hospital based, time bound study was done in the Department of Obstetrics and Gynaecology of a Teaching Institute of Northeastern India from January 2016 to August 2017. We included all the pregnant women or puerperia with heart disease who delivered during that time period. Institutional Ethics Committee approval was taken for the study. A written consent was obtained from all participants and they were fully informed about the study. The inclusion criteria was pregnant patient or puerperia presenting with signs and symptoms of heart disease and further confirmed by diagnostic tests, known case of heart disease during routine antenatal checkup, previously diagnosed with heart disease who are treated either medically or surgically, and chronic hypertension with structural heart changes. The exclusion criteria was patients presenting with signs and symptoms suggestive of heart disease but excluded after evaluation, patients with cardiac failure due to non cardiac cause. The present study included 55 pregnant women or puerperia having heart diseases who delivered during study period and pregnancy outcome was compared with 55 pregnant women without heart disease admitted during the same period as control group. A detailed antenatal workup was done including detailed obstetric and cardiac history, thorough clinical examination. All women were subjected to routine antenatal tests and Echocardiogram (ECG) and Electrocardiography (ECHO). Based on the symptoms all the patients were classified according to New NYHA functional classification [11]. Patients were advised to have regular antenatal check-up and compulsory institutional delivery. Patients were evaluated for development of any cardiac complication like arrhythymia, congestive cardiac failure and atrial fibrillation. Any obstetrical complication like preterm labour, foetal growth restriction, oligohydramnios and perinatal outcomes like intrauterine death, low birth weight, prematurity and respiratory distress syndrome etc. The results of the study were compared with feto-maternal outcome of equal number of pregnancies without heart disease, which were taken as controls.
Statistical Analysis
For demographic and obstetric variables descriptive statistics was used to calculate the Mean±SD. To compare the means of parameters of both the groups’ independent student test was performed and 95% limit and 5% level of significance were adopted. A p-value <0.05 was considered significant. Statistical analysis was performed using the SPSS software package (SPSS for window, version 16.0 SPSS, Inc Chicago, IL, USA).
Results
Prevalence of Heart Disease
The total number of deliveries during the study period was 2029 and total number of abortions was 344. The prevalence of heart disease in pregnancy was 2.32%. Out of the total 55 cases 15 (27.27%) were referred, 25 (45.45%) were booked and 15 (27.27%) were unbooked.
Age and Parity Distribution
The mean age of women with heart disease was 27.58±5.6 years and the mean age of controls were 25.14±4.825 years (p-value >0.05). The maximum number of cases were multigravida 50.91% and 52.73%, followed by primigravida 38.18% and 40% both in the cases and the control group respectively (p-value>0.05).
Spectrum of Heart Disease-In Present Study
Congenital heart disease was the most common encountered type 49.09% followed by RHD 41.82% [Table/Fig-1].
Spectrum of heart disease.
| Type of heart disease | Number (%) |
|---|
| Congenital | 27 (49.09%) |
| RHD | 23 (41.82%) |
| Cardiomyopathy | 4 (7.27%) |
| Arrhythmia | 1 (1.82%) |
| Grand Total | 55 (100.00%) |
[Table/Fig-2] depicts the different heart lesion found among the cases. The most frequently involved valve in RHD was mitral valve (47.27% of all cases) followed by aortic 21.81%. The most widespread congenital lesion was Ventricular Septal Defect (VSD) (16.36%). A total of 10 (18.18%) patients had undergone corrective cardiac surgery. Atrial Septal Defect (ASD) closure was most common corrective surgery done (9.09%).
Distribution of different heart lesions among cases.
| Types of heart disease | Number (%) |
|---|
| Valvular lesion (RHD) | Mitral | 26 (47.27) |
| Aortic | 12 (21.81) |
| Tricuspid | 5 (9.09) |
| Pulmonary | 0 (0) |
| Congenital lesions | VSD | 9 (16.36) |
| ASD | 8 (14.55) |
| PDA | 3 (5.45) |
| Ebstein anomaly | 1 (1.82) |
| Tetralogy of fallot | 1 (1.82) |
| Corrected cardiac lesion | Post ASD closure | 5 (9.09) |
| Post mitral valve replacement | 1 (1.82) |
| Post mitral valvotomy | 1 (1.82) |
| Post PDA closure | 1 (1.82) |
| Post VSD closure | 2 (3.64) |
| Peripartum cardiomyopathy | 4 (7.27) |
| Wolf parkinson white syndrome | 1 (1.82) |
| Eisenmenger syndrome | 1 (1.82) |
RHD: Rheumatic heart disease; VSD: Ventricular septal defect; ASD: Atrial Septal Defect; PDA: Patent ductus arteriosus
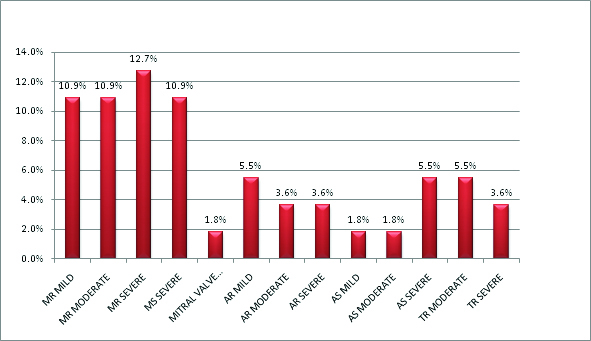
As shown in [Table/Fig-3], the most common valvular lesion was found to be mitral regurgitation (34.5%), followed by mitral stenosis (10.91%).
Spectrum of valvular heart disease (cases).
NYHA Status
The cases were divided on the basis of their NYHA status in four classes. Maximum patients belonged to Class 1 and 2 (69.09%), 9.09% were classified as NYHA Class 3 and 21.82% as Class 4.
Cardiac Complications
In the present study out of 55 cases 10 (18.18%) had cardiac complications. Most common cardiac complication was congestive cardiac failure (80%) [Table/Fig-4]. Five patients (50%) developed cardiac failure during intrapartum period, while 30% during postpartum period and 20% in antenatal period.
Cardiac complications among the cases.
| Cardiac complications | Cases |
|---|
| Number (% of total cases) |
|---|
| Congestive Cardiac Failure (CCF) | 8 (14.5%) |
| Atrial Fibrillation (AF) | 1 (1.8%) |
| CCF+AF | 1 (1.8%) |
Obstetric Events and Outcome
Period of gestation at delivery: In present study, mean gestational age at delivery among cases was 36.8±5.64 weeks and among controls it was 38.52±2.37 weeks. Maximum number of patients had term delivery i.e., 65.45% and 87.27% in cases and controls respectively. As shown in [Table/Fig-5], there is higher incidence of preterm labour in women with heart disease (25% vs. 7.27%, p-value=0.0326).
Period of gestation at delivery.
| Pregnancy outcome | Cases:Number (%) | ControlsNumber (%) | p-value |
|---|
| Term | 36 (65.45) | 48 (87.27) | - |
| Preterm | 13 (23.63) | 4 (7.27) | 0.0326 |
| Postdated | 3 (5.45) | 3 (5.45) | 1 |
Data on the period of gestation at delivery for only 52 women out of 55 women were available because 3 women aborted and only 52 women delivered.
Associated Obstetric Complications
In present study, most common antenatal complication among cases was preterm labour (23.63%) followed by hypertensive disorder of pregnancy (18.18%) [Table/Fig-6]. Although rate of hypertension, Intrauterine Growth Restriction (IUGR) and abortion were high among cases than control but it was not statistically significant. There were 6 (11.53%) intrauterine foetal death cases among cases and none in control group (p-value 0.0113).
Associated obstetric complications among cases and controls.
| Obstetrical complication | Cases: Number (%) | Control:Number (%) | p-value |
|---|
| Preterm labour | 13 (23.63) | 4 (7.27) | 0.0326 |
| Hypertensive disorders of pregnancy | 10 (18.18) | 5 (9.09) | 0.2662 |
| Oligohydramnios | 9 (16.36) | 5 (9.09) | 0.3916 |
| Previous Lower segment caesarean section | 5 (9.09) | 6 (10.91) | _ |
| Intrauterine growth restriction | 4 (7.27) | 1 (1.82) | 0.3634 |
| Cholestasis | 3 (5.45) | 1 (1.82) | _ |
| Malpresentation | 3 (5.45) | 1 (1.82) | _ |
| Gestational Diabetes Melitus | 2 (3.64) | 0 (0.00) | _ |
| Hypothyroidism | 2 (3.64) | 0 (0.00) | _ |
| Rh negative | 2 (3.65) | 0 (0.00) | _ |
| Bad obstetric history | 1 (1.82) | 0 (0.00) | _ |
| Postdated | 1 (1.82) | 5 (9.09) | _ |
| Cephalopelvic disproportion | 1 (1.82) | 2 (3.64) | _ |
| Antepartum haemorrhage | 0 (0.00) | 2 (3.64) | _ |
| Preterm Premature rupture of membrane | 1 (1.82) | 0 (0.00) | _ |
| Post partum Haemorrhage | 3 (5.45) | 1 (1.82) | _ |
| Retained placenta with shock | 1 (1.82) | 0 (0.00) | _ |
| Abortion | 3(5.45) | 0(0.00) | 0.243 |
| Anaemia (Hb <11gm%) | 30 (54.55) | 18 (32.73) | 0.0339 |
| Grand total | 49 (89.09) | 29 (52.73) | _ |
Obstetrical complication occurred in 49 women among case group and 29 women among control group.
Mode of Delivery
There was no significant association found between the two groups in term of mode of delivery (p-value=0.4415). However, the proportion of instrumental delivery was higher among the cases than in the controls with p-value=0.0296 [Table/Fig-7].
Showing the mode of delivery.
| Mode of delivery | Sub Category | Cases:Number (%) | Controls:Number (%) | p-value |
|---|
| Vaginal | | Vaginal delivery | 15 (28.84) | 21 (38.18 | 0.4415 |
| Instrumental | Ventouse | 9 (17.30) | 3 (5.45) |
| Forcep | 3 (5.76) | 1(1.82) |
| Assisted breech | 1 (1.92) | 0.00 |
| LSCS | | Postmortem | 2 (3.84) | 0 (0.00) | - |
| Elective CS | 9 (17.30) | 9 (16.36) |
| Emergency CS | 13 (25.00) | 21 (38.18) |
| Grand Total | 52 (100.00) | 55 (100.00) | |
Foetal and Neonatal Outcome
In the present study out of 52 pregnancies among cases only 88.46% had live birth. This is in contrast to controls where 100% had live birth. The foetal outcome was better in controls and showed a statistical significance with p-value of 0.0113.
Birth Weight
In present study, average birth weight among case and control groups was 2760±772 gm and 2903±543 gm respectively. Low birth weight was found in 34.61% babies among cases which is significantly higher than control (12.73%) (p-value=0.0112).
Neonatal Morbidity and Mortality
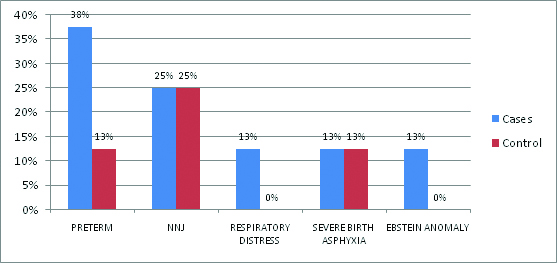
There was more Neonatal Intensive Care Unit (NICU) admission among the cases (15.38%) vis-a-vis controls (7.27%), (p-value 0.2284). The most common indication for NICU admission was prematurity (38%) among the case and Neonatal jaundice (25%) in the controls [Table/Fig-8]. There was no neonatal mortality.
Showing indications of NICU admission.
Maternal Mortality among Heart Disease Patients
Total number of maternal mortalities during the study period were 29 out of which 3 (10.34%) were attributed to cardiac causes.
The percentage of maternal mortalities was 5.45% among those having heart disease. There was no maternal mortality among the controls (p-value-0.0281). From the [Table/Fig-9], we conclude that all three mothers who expired belonged to NYHA Class 4 and were anaemic. Mortality were high when left ventricular ejection fraction was <45% (20% mortality). All had RHD with mitral valve involvement. Two (66.67%) expired during the intrapartum period and one during the antenatal period. Two (66.67%) of the mothers who died had hypertensive disorder of pregnancy.
Maternal mortality details.
| Mortaliy | Type of heart disease | NYHA class | Period of gestation (weeks) | Associated complications | Time of death |
|---|
| Case 1 | severe MS* | 4 | 39 | Anaemia, HDP*** | Intrapartum |
| Case 2 | severe MS | 4 | 32 | Anaemia, HDP | Antenatal |
| Case 3 | severe MR** | 4 | 20 | Anaemia | Intrapartum |
*MS-Mitral Stenosis, **MR-Mitral Regurgitation, *** HDP- Hypertensive Disorder of Pregnancy
Discussion
The number of women with heart disease, who reach childbearing age in a good functional state, has increased due to the improved facilities for diagnosis and treatment. As a result, pregnancy becomes a realistic option for many of these young women.
The prevalence of heart disease in pregnancy in present study was 2.32%. Prevalence among various studies done in India and abroad was from 1.3 to 4.3% [4,10,12,13]. On the contrary, study in Nepal showed a prevalence of 0.6% only [14]. The mean age of women with heart disease was 27.58±5.6 years which was comparable to other studies [12,15]. Similar to other studies; maximum number of women were multigravida, (50.91%) followed by primigravida 38.18% [3,16].
In comparison to previous Indian studies on the topic, interesting finding of this study is that congenital heart disease constituted the most commonly encountered lesion (49.09%) followed by RHD (41.83%). Peripartum cardiomyopathy was observed in 7.27% of cases and arrhythmia (Wolff-Parkinson-White syndrome) was present in 1.82%. However there were no patients with ischaemic heart disease.
In the western population, various studies proved that the principal cardiac lesion was congenital. Siu SC et al., recorded congenital lesions in 445 pregnancies (74%), acquired in 127 pregnancies (22%), and arrhythmic in 27 pregnancies (4%) [Table/Fig-10] [17]. However, in developing countries like India the scenario is different with all studies showing the predominant cardiac lesion to be RHD (69%) followed by congenital heart disease (21%) and the ratio of patients with congenital heart disease relative to patients with RHD was 1:3 [Table/Fig-10] [9,12-14,16].
Spectrum of heart disease in various studies.
| Study | Congenital | Acquired |
|---|
| Siu SC et al., [17] | 74% | 22% |
| Stangl V et al., [15] | 81.7% | 10.8% |
| Konar H et al., [16] | 21% | 69% |
| Khursheed R et al., [9] | 24.24% | 71.96% |
In developing countries, the incidence of RHD for years has continued to be higher, as most of the patients belonged to low socioeconomic class where poverty, poor nutrition, low level of sanitation and hygiene and inaccessibility to health services are common. Contrary to this, present study reveals most common cardiac lesion to be congenital followed by rheumatic. This signifies a paradigm shift in the spectrum of heart disease which can be attributed to improved health services, better antibiotic prophylaxis for streptococcal disease, better standard of living, and better diagnostic facilities leading to diagnosis of conditions which perhaps were under diagnosed previously. Also, increasing number of surgeries done for congenital heart lesions in the recent years have enabled these women to reach reproductive age and conceive. Our institute being the only tertiary care centre of the region with a well established cardiothoracic vascular surgery and cardiology department, we receive patients at various stages including those who are referred for various surgical interventions and also those who underwent corrective surgeries at our institute (as follow-up).
Among the RHD the most commonly involved valve was mitral valve (47.27%) followed by aortic (21.27%). The most common valvular lesion was found to be mitral regurgitation (34.5%). Other studies also mentioned mitral valve was the commonest valve involved and mitral stenosis in RHD was the most common lesion [3,12,13,16]. In present study, a total of 10/55 (18.18%) patients had undergone corrective cardiac surgery. ASD closure was most common corrected heart lesions (9.09%). In another study, a total of 1321 cases were studied and 65.85% of the patients, had surgical intervention done (579 for congenital lesion and 291 valvular interventions) [3].
In the present study, 10 (18.18%) had cardiac complications. The most common complication was congestive cardiac failure (80%). About 50% developed congestive cardiac failure during intrapartum and 30% developed during postpartum alike our study. Siu SC et al., recorded cardiac event in 13% of study subjects but in contrast to the present study 55% occurred in the antepartum period [17]. Another study in west estimated severe maternal complications in 12.9% out of which 50% had heart failure, 25% had arrhythmias, and 2.2% thrombotic complications [15]. Other studies from India, revealed similar findings where most cases had cardiac failure during labour [16], and the most frequent cardiac event was congestive cardiac failure in 43.9% [9].
Preterm delivery was significantly higher (24%) in present study which is similar to other study [15]. In present study, 53.84% of cases delivered vaginally and 46.15% by LSCS. The percentage of instrumental vaginal deliveries (23.06%) was higher among cases which are fairly justified in an attempt to cut short second stage of labour. Though some studies showed a lower rate of vaginal delivery in 45.2% cases and caesarean delivery in 54.8% [15]; two other studies mentioned a higher rate of vaginal delivery (53% and 46.6%) [14,16].
In the present study, 88.46% had live birth while 11.53% had intrauterine foetal demise. There were no neonatal mortalities in present study population. Similar results were concluded by Puri S et al., where 86% had live birth and 14% had stillbirth [13]. On the contrary western literature showed lower foetal mortality due to better antepartum and intrapartum care. Moutquin JM et al., reported that foetal/neonatal mortality rate (2%) was higher than that reported in general obstetric population (0.3%) [18]. Roos Hessellink JW et al., also stated foetal and neonatal mortality occurred in 1.7% and 0.6% cases respectively, both higher than in the normal population [3].
Low birth weight was found statistically higher. On the contrary, in a study done in developed country, mean birth weight was better (2957±621 gm) and LBW (Birth weight <2500 gm) was seen only in 16.7% cases [15]. The better outcome in western countries can be associated with better standard of care provided to the antenatal mothers. Whereas other studies in Indian show a higher proportion of LBW and a lower mean birth weight [13,14,16]. Bangal VB et al., got an incidence of LBW as high as 60% in heart disease cases and 42% in women without heart disease [12].
The maternal mortality is used as a measure of the quality of a healthcare system. With the increase in prevalence of heart diseases in pregnant women, it has emerged as an important cause of maternal mortality especially so in the developing countries. In present study heart disease was attributed in 10.34% of cases of maternal mortality. Konar H et al., stated that heart diseases associated with pregnancy accounted for 15% of pregnancy related mortality [16]. Multidisciplinary approach with careful monitoring of high risk cases which is apparently the reason for lesser number of women dying due to cardiac related causes at our institute.
On evaluating the three maternal deaths we conclude that all three mothers who died belonged to NYHA Class 4 and were anaemic. All had RHD with mitral valve involvement. About 66.67% of the mothers who died had hypertensive disorder of pregnancy. Siu SC et al., also stated in their study that mitral stenosis is the most common valvular lesion in pregnant women with RHD and patient does not performed well with this lesion [17,19]. Even moderate mitral stenosis is one of the predictor of poor outcome and intervention should be done preconceptionally [2,17]. Like in present study, Sawhney H et al., concluded that pregnant women with severe symptoms have a mortality risk up to 5-15% [20]. In contrast to this study, a lower maternal mortality of 1.1%, 3.09% and 4% was recorded in a study by three other authors [12-14].
Limitation
Limitations of present study lie in the fact that all the neonates born to women with congenital heart disease were not routinely followed up for inheritance of congenital cardiac lesions.
Conclusion
The prevalence of heart disease among pregnant women was found to be 2.32%. Congenital heart disease is the predominant lesion followed by RHD. This indicates a significant change in trends and spectrum of heart disease in present study. Increase accessibility of treatment for congenital cardiac disease, more and more women reaching to child bearing age with relative lower incidence of RHD, congenital heart disease will continue to rise and hence expertise in management of such conditions is imperative in times to come.