Stroke burden in India has been rising since last few decades, in contrast to developed countries, where stroke prevalence has decreased or plateaued [1,2]. Recent studies have shown that vitamin D deficiency could be a cause of thrombus formation, and it has been suggested that vitamin D has anti-thrombotic properties that include “up-regulation of thrombomodulin” and “down-regulation of Tissue Factor (TF)”, which play an important role in thrombus formation mechanism [3-5].
Ischaemic stroke as well as cardiovascular disease has been shown to have a strong association with vitamin D status [6,7]. However, the opinion on this issue is highly divided as far as Indian population is concerned, with a recent study indicating the existence of no such association while other studies have indicated a strong association between vitamin D levels and ischaemic stroke [8,9].
Most of the studies have evaluated the independent associations of vitamin D levels and CIMT with acute ischaemic stroke or an association between vitamin D levels and CIMT, there is only one study that has studied the relationship between vitamin D levels and CIMT in acute ischaemic stroke patients, thus indicating that this relationship needs to be studied in this specific context [10].
Materials and Methods
This case-control study was performed at a tertiary care centre from February 2014 to August 2015 after approval from the ethics committee. The study included adults aged more than 40 years, of either sex, attending Department of General Medicine. Based on a previous study, 110 consecutive subjects with acute ischaemic stroke were selected as cases and 55 healthy age and gender match subjects were included as controls [10]. Subjects with haemorrhagic and embolic strokes were excluded from the study.
Stroke suspected on the basis of history and clinical examination were further investigated to confirm ischaemic stroke by CT/MRI imaging. Demographic details, personal habits, clinical profiles of the patients were noted on a predesigned format. These patients were then subjected to haematological and biochemical investigations, including quantitative serum 25-Hydroxyvitamin D {25(OH)D} levels and CIMT measurement on day 1 of admission.
Vitamin D Estimation: Quantitative measurement of 25-OH vitamin D in serum and plasma samples was done using Chemiluminesecent Microparticle Immunoassay (CMIA) technology, (referred to as Chemiflex with flexible assay protocol). In the first step, the sample was pre-treated to dissociate the vitamin from its binding sites. An aliquot of the pre-treated sample was then reacted with paramagnetic anti-25-OH-vitamin D coated microparticles. After incubation, a biotinylated 25-OH-vitamin D anti-biotin acradinium-labeled conjugate complex was added. After washing, pre-trigger and trigger solutions were added to produce a chemiluminescent reaction and Relative Light Units (RLUs) were measured. An indirect relationship existed between the amount of 25-OH-vitamin D in the sample and the RLUs detected.
The criteria as proposed by Gallagher JC et al., was used to describe vitamin D deficiency, insufficiency and sufficiency [Table/Fig-1] [7].
Different Vitamin D levels categories.
| Category | 25(OH)D2 Levels |
|---|
| Deficiency | <10 ng/mL |
| Insufficiency | 10-30 ng/mL |
| Sufficiency | 30-100 ng/mL |
CIMT Measurement: All examinations were performed by a single examiner. The examination was performed with a Logiq 5 ultrasound system (GE Healthcare, Milwaukee, WI, USA) using 7–10 MHz linear transducer. CCA images were obtained to measure IMT by using three different angle views for each vessel. At least three IMT points were measured in the near and far walls in the most thickened area of each vessel. The maximum IMT value was selected for each angle. An IMT superior to 0.07cm was considered to be an abnormal finding [8].
Statistical Analysis
Data so obtained was subjected to statistical analysis using Statistical Package for Social Sciences version 20.0. (SPSS Inc., Chicago, IL, USA). Data were presented as mean±SD or n (%). Student’s t-test was used for comparison of continuous variables. The results of comparing the correlation between two continuous variables were indicated by the correlation coefficient (r) using correlation analysis. A result was deemed statistically significant when p <0.05.
Results
A total of 110 patients fulfilling the inclusion criteria were enrolled in the study. Apart from these, 55 age and gender matched subjects were included as controls. Baseline characteristic of all cases and controls are presented in [Table/Fig-2]. Majority of the subjects were males (55.45%) and more than 60 years of age (n=112; 67.88%). Male to female ratio in this study was 1.24:1 in cases and 1.29:1 in controls.
Baseline characteristics of study population.
| Characteristics | Cases (N=110) | Controls (N=55) | p-value |
|---|
| Age (Mean±SD) | 70.14±12.14 | 64.27±10.66 | 0.078 |
| Sex (M/F Ratio) | 1.24:1 | 1.29:1 | |
| SBP mmHg (Mean±SD) | 191.20±18.05 | 127.27±13.22 | <0.001 |
| DBP mmHg (Mean±SD) | 110.80±9.38 | 86.22±9.06 | 0.003 |
| Haematocrit (%) (Mean±SD) | 35.03±4.50 | 35.96±3.89 | 0.189 |
| WBC (x1000) (Mean±SD) | 8.83±3.80 | 7.11±2.17 | 0.002 |
| S. Na+ (mmol/L) (Mean±SD) | 137.72±4.84 | 137.18±4.97 | 0.507 |
| S. K+ (mmol/L) (Mean±SD) | 4.55±0.60 | 4.87±0.39 | <0.001 |
| HDL (mg/dl) (Mean±SD) | 37.18±5.13 | 41.84±6.09 | <0.001 |
| LDL (mg/dl) (Mean±SD) | 99.9±21.10 | 81.65±12.41 | <0.001 |
| VLDL (Mean±SD) | 22.46±3.31 | 21.10±2.82 | 0.01 |
| S.Cholesterol(mg/dl) (Mean±SD) | 159.55±20.63 | 144.59±12.77 | <0.001 |
| S.Triglyceride (mg/dl) (Mean±SD) | 112.32±16.55 | 105.49±14.08 | 0.01 |
| Vitamin D levels (ng/mL)(Mean±SD) | 13.35±5.58 | 18.78±9.28 | <0.001 |
| CIMT (mm) R (Mean±SD) | 0.09±0.01 | 0.07±0.01 | <0.001 |
| CIMT (mm) L (Mean±SD) | 0.09±0.01 | 0.07±0.01 | <0.001 |
| CIMT (mm) Mean (Mean±SD) | 0.09±0.01 | 0.07±0.01 | <0.001 |
| Hypertension (n) (%) | 79(71) | 29(52) | |
| Diabetes mellitus (n) (%) | 80 (72) | 17 (31) | |
| Obesity (n) (%) | 68 (62) | 17 (31) | |
| Smoking (n) (%) | 74 (67) | 30 (54) | |
| C-Reactive protein (positive) (%) | 80 (77) | 0 (0) | <0.001 |
Between 110 cases, diabetes mellitus (80, 72.72%) and hypertension (79, 71.82%) were the most common cardiovascular. History of smoking was recorded in 74 (67.27%) cases. 12 (10.91%) cases had only single risk factor, 29 (26.36%) cases had two risk factors, 45 (40.91%) cases had three risk factors and 24 (6.7%) cases had four or more risk factors. Proportion of cardiovascular risk factors was higher in cases as compared to controls.
C-Reactive protein was negative in all the controls while it was positive in the majority of cases (77.27%). Difference in C-reactive protein of both the groups was found to be statistically significant (p<0.001).
Majority of subjects (59.39%) of the study population had vitamin D insufficiency. Another one-third (34.44%) had vitamin D deficiency and only 6.06% had Vitamin D levels within normal limits. Difference between the mean Vitamin D levels of cases (13.35±5.58 ng/mL) and controls (18.78±9.28 ng/mL) was found to be statistically significant (p<0.001).
CIMT of left as well as right internal carotid artery in both groups ranged from 0.06-0.10. Mean CIMT of cases (0.09±0.01 mm) was found to be higher than that of controls (0.07±0.01 mm), and the difference between the two groups in CIMT of left artery was found to be statistically significant (p<0.001).
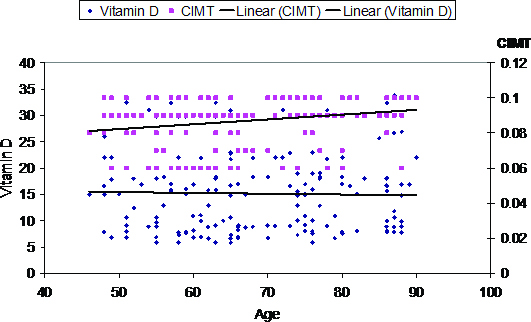
We subsequently analysed the correlation between age and vitamin D levels in the entire study cohort, it was observed that the correlation between age and vitamin D levels was not statistically significant (r= -0.024; p=0.759). A weak (r= -0.184) statistically significant (p=0.018) negative correlation between CIMT and Vitamin D levels was found [Table/Fig-3,4].
Correlation of Age, CIMT (Mean) with serum Vitamin D.
| Age | CIMT (Mean) |
|---|
| R | Grade of correlation | ‘p’ | r | Grade of correlation | ‘p’ |
| -0.024 | Weak | 0.759 | -0.184 | Weak | 0.018 |
Linear regression analysis of age with Vitamin D levels and CIMT showing a weak correlation between age and CIMT(r=-0.184; p=0.018). There is no evident linear relationship between age and Vitamin D levels.
CIMT: Carotid Intima Media Thickness
Prevalence of various risk factors in subjects with vitamin D deficiency, vitamin D insufficiency, and normal vitamin D levels is presented in [Table/Fig-5]. It was observed that Type 2 Diabetes Mellitus was higher in Vitamin D deficient (71.93%) as compared to Vitamin D insufficient (52.04%) and Vitamin D sufficient (50.00%). This association was also found to be statistically significant (p=0.045). Proportion of smoker subjects was higher in Vitamin D deficient (100.00%) as compared to Vitamin D insufficient (47.96%) and Vitamin D sufficient (0.00%). This association was also found to be statistically highly significant (p<0.001) [Table/Fig-5].
Association of risk factors with Vitamin D.
| | Deficiency (n=57) | Insufficiency (n=98) | Sufficiency (n=10) |
|---|
| Hypertension | | | | |
| Absent | 57 | 22 | 31 | 4 |
| Present | 108 | 35 | 67 | 6 |
| | χ2=0.913 (df=2); p=0.634 | |
| Obesity | | | | |
| Absent | 80 | 41 | 34 | 5 |
| Present | 85 | 16 | 64 | 5. |
| | χ2=20.015 (df=2); p<0.001 | |
| Diabetes | | | | |
| Absent | 68 | 16 | 47 | 5 |
| Present | 97 | 41 | 51 | 5. |
| | χ2=6.223 (df=2); p=0.045 | |
| Smoking | | | | |
| Absent | 61 | 0 | 51 | 10 |
| Present | 104 | 57 | 47 | 0 |
| | χ2=60.034 (df=2); p<0.001 | |
| CIMT | | | | |
| <0.07 | 31 | 10 | 17 | 4 |
| >0.07 | 134 | 47 | 81 | 6 |
| | χ2=3.140(df=2); p=0.208 | |
| Age | | | | |
| Upto 60 | 53 | 17 | 32 | 4 |
| 61-70 | 42 | 20 | 20 | 2 |
| >70 | 70 | 20 | 46 | 4 |
| | χ2=4.679(df=4); p=0.322 | |
Overlapping of these risk factors was found in the majority of the patients. Whether combination of these risk factor can affect the Vitamin D levels was further evaluated. A declining trend in Vitamin D levels was observed with an increase in the number of risk factors i.e., Vitamin D levels were found to be maximum in patients with a single risk factor (20.24±4.39 ng/mL) followed by with two risk factors (15.21±6.09 ng/mL), with three risk factors (11.65±4.30 ng/mL) and minimum with all the four risk factors (10.82±4.01 ng/mL). This association was found to be statistically significant (p<0.001).
Discussion
We observed that mean vitamin D levels of cases (13.35±5.58 ng/mL) was significantly lower as compared to that of controls (18.78±9.28 ng/mL). With respect to mean levels, a number of studies in past using case-control design have reported different findings [11-13].
The mean levels between cases and controls were found to be lower in the present study in comparison to another cross-sectional case-control study data from the Indian subcontinent [8]. Incidentally, none of the previous studies showed a significant difference in mean vitamin D between cases and control [8,12]. However, the present study showed this difference to be statistically significant.
A variability in prevalence of vitamin D deficiency in different study populations might be owing to the difference in cut-off values taken for consideration of deficiency. In the present study, it was taken as <10 ng/mL. However, Chaudhuri JR et al., and Gupta A et al., considered it at a cut-off value <20 ng/mL and thus reported the deficiency rate to be higher as compared to present study. Whereas, Thapa L et al., considered <20 ng/mL as the criteria for deciding vitamin D deficiency and classified 20-29 ng/mL as insufficiency yet found its rate to be much lower. The findings thus suggest that on a population basis, the vitamin D deficiency rates vary substantially and do not correspond to a particular trend [9,14,15].
Previous studies indicate a higher prevalence of ischaemic stroke in males [16-18]. These findings indicated that gender could be instrumental in determining the vitamin D levels.
In the present study, on haematological assessment, no statistically significant difference was observed in any of the parameters except total leucocyte count, which was significantly higher in cases as compared to controls. In previous studies, it was observed that leucocytosis is a characteristic finding in acute phase of stroke, which is subsequently normalized within days of successful thrombolysis [13,19].
This study also showed a significant difference between cases and controls with respect to C-reactive protein levels. Like white blood cells, which is marker of acute phase of inflammation in stroke, CRP levels as an indicator of inflammatory response were observed to be raised in acute ischaemic stroke patients and magnitude of their rise depends on the extent of blood pressure rise during the stroke [20].
Proportion of subjects with type 2 diabetes mellitus, obesity, smoking and hypertension were significantly higher among cases as compared to controls. These variables have a strong proven link with acute ischaemic stroke, and this difference was statistically significant and well documented in the present study too [21,22].
It was also observed that most of the subjects (93.94%) in the entire study population had mean vitamin D levels much below the normal range (30-100 ng/mL). With such a widespread vitamin D deficiency even in the controls, it is difficult to assume that only vitamin D deficiency is the cause of acute ischaemic stroke, more so in view of the findings that except for present study, none of the previous studies from Indian subcontinent had shown a significant difference in mean vitamin D levels of stroke patients as compared to matched healthy subjects and only one study has observed it in categorical terms [9]. Thus, in categorical terms, we were unable to find an association of vitamin D insufficiency/deficiency to be associated with risk of ischaemic stroke.
Working on the above postulates we looked for the possible reasons that could be responsible for lower mean vitamin D levels in stroke patients as compared to controls. One of the reasons for this could be the difference in age profile of two groups. An association between age and declining vitamin D levels is well established, and as such could be responsible for the difference in mean vitamin D levels of cases as compared to controls [6]. However, age did not emerge as a counfounding factor in our study.
It is noteworthy to mention here, patients in the present study were enrolled throughout the year and in different seasons and as such, the slight yet statistically significant difference in mean values of vitamin D levels between cases and controls could be dependent on these confounders rather than on stroke status of patients [9].
Contrary to present study and most of the other studies that have been carried out using a case-control design, examining the relationship between vitamin D levels and acute ischaemic stroke risk, the western studies have followed longitudinal design and used vitamin D levels and their changing pattern as a predictor of outcome in stroke patients. In these studies, large sample sizes, and longer follow up have focused on dietary vitamin intake and then correlated it with stroke risk, thus providing a more cogent risk assessment rather than a cross-sectional observation as observed in present study and several other studies from Indian subcontinent as reported above.
Hence, despite finding a significant difference in mean vitamin D levels of cases as compared to controls, we do not find it to be a convincing evidence as yet and recommend further studies to corroborate these findings in wider perspective. This assumption of ours is based on the premise of studies from western literature that show no significant association of vitamin D levels with risk of stroke when considered in a wider perspective taking into account socio-demographic factors, co-morbidities and laboratory values, including parathyroid hormone despite showing a higher risk of stroke [23].
As far as the association of CIMT with vitamin D levels is concerned it also seems to be controversial with some studies endorsing its existence while some others denying this in some specific group of patients [24,25]. A recent study from India has shown a mild inverse correlation between Vitamin D levels and CIMT [10]. We found the CIMT values of either side as well the mean to be significantly higher in cases as compared to controls, thus showing an association between CIMT with an increased risk of acute ischaemic stroke. The present study revealed no significant association between CIMT and Vitamin D level. Although assessment of a linear correlation between CIMT and vitamin D levels yielded a significant yet a weak inverse correlation (r=-0.184; p=0.018) between two, thereby indicating that two are very weakly interrelated and probably confounded by other factors. The findings thus suggest that there can be a role of vitamin D in acute ischaemic stroke but it is confounded by a number of factors such as obesity, diabetes and smoking as observed in present study and age, sex, hypertension, dyslipidemia as observed in other studies and hence it is still premature to jump on existence of any such relationship in view of the conflicting evidence in literature as well as absence of any such association on categorical evaluation in view of high vitamin D insufficiency/deficiency in our study population. However, CIMT were better correlated with ischaemic stroke risk. Similar to stroke, CIMT also had poor correlation with vitamin D levels.
Limitation
Vitamin D levels are affected by a host of factors, including exposure to sun, dietary habits, age and menopausal status in women. Apart from this, the effect of smoking habit and its frequency and duration has also been shown to exist. In the present study, owing to limitations we could not evaluate all these factors.
Conclusion
The findings suggest that there is a probable association between low Vitamin D levels and acute ischaemic stroke. However, in view of presence of numerous confounding factors like diabetes, hypertension and obesity in our study a definite causal relationship cannot be established. Although both Vitamin D levels and CIMT show a strong association with acute ischaemic stroke; the linear relationship between Vitamin D levels and CIMT is rather weak.