Diode Laser-Assisted Fibrotomy in the Management of Oral Sub-Mucous Fibrosis: A New Technique in Surgical Management
Sana Farista1, Butchibabu Kalakonda2, Shanin Farista3, Vidyaa Hari Iyer4
1 MDS, Department of Periodontics, Consulting Periodontist, Mumbai, Maharashtra, India.
2 Associate Professor, Department of Periodontics, Al Farabi Dental College and Hospital, Riyadh, KSA, Saudi Arabia.
3 Associate Professor, Department of Conservative dentistry and Endodontics, Chhattisgarh Dental College and Research Institute, Rajnandgaon, Chhattisgarh, India.
4 BDS, Department of General Dentistry, Private Practitioner Smile Dental Clinic, Chennai, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Shanin Farista, 702, I Wing, Green Park, Opp. Valavalkar Park, Mhada Colony, Best Colony Road, Oshiwara, Andheri West, Mumbai, Maharashtra, India.
E-mail: docshaninfarista@gmail.com
Oral Sub-Mucous Fibrosis (OSMF) has a high prevalence in the Indian subcontinent and is a matter of grave concern because of its alarming malignant potential. Numerous treatment modalities; from antioxidants, vitamin supplements, placental extract injections to surgical methods (fibrotomy either by the use of a scalpel or an electrocautery) have been attempted with varying degrees of success along with some disadvantages associated with each. With the advent of technology, laser offers certain advantages which was utilized in this case to overcome the shortcomings of conventional technique.
Check pattern, Fibrotic bands, Non invasive, Trismus
Case Presentation
Case 1: A 35-year-old woman presented to our hospital with a chief complaint of burning sensation on consumption of spicy food with associated difficulty in mouth opening. Her medical history was non-contributory, on further questioning, she revealed that she had the habit of chewing pieces of areca nut at least 5 times a day and she was doing this for the past 15 years. Further examination revealed that her mouth opening was restricted with an inter-incisal distance of less than 30mm whereas average mouth opening is 40mm [Table/Fig-1]. Intra oral examination revealed a generalised pale oral mucosa with fibrotic bands that were palpable bilaterally over the buccal mucosa. A diagnosis of moderate stage of OSMF was arrived on the basis of presenting clinical features and findings from an incisional biopsy wherein the photomicrograph of the tissue showed atrophic epithelium, relatively avascular hyalinized collagen with abundant inflammatory infiltrate.
Pre-operative view for case-1.

Case 2: A 36-year-old man presented to our hospital with a limited mouth opening. He was well aware that he was earlier diagnosed with OSMF two years back and was under medication comprising of antioxidants. Though he was advised to stop areca nut chewing habit, but he didn’t which deteriorated his condition further. On intraoral examination, it was found that his buccal mucosa was completely blanched and fibrosis was evident on palpation. His mouth opening was less than 30 mm, considering the presenting clinical features; a diagnosis of moderate stage of OSMF was made [Table/Fig-2].
Pre-operative view for case-2.

Surgical Technique: The patients were explained about the pharmacological aspects and the use of lasers for the management of their problem. Both the patients had given their consent for the use of laser. All the necessary precautions were taken and the clinician and the patients were instructed to put on the protective eye wear.
EZLASETM, a 940 nm diode laser (BIOLASE International) was used for the procedure. Laser was used only in the area where fibrotic bands were present. Since both the patients were apprehensive, sufficient amount of local anaesthesia (2% lignocaine with 1:100,000 epinephrine) was used to thoroughly infiltrate the target area.
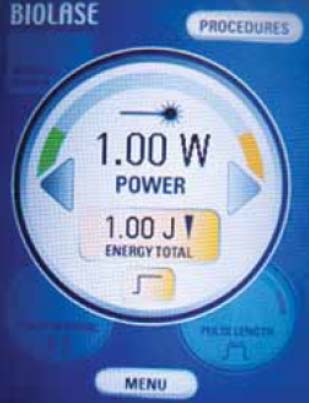
Initial demarcation of the fibrotic bands was done using the 400 μm laser tip in one Watt pulse mode (pulse interval 50 μsec and pulse duration 50 usec). Later, the laser was used in a continuous mode with 1 Watt power [Table/Fig-3], lasing from the retromolar area to the premolar area achieving a desired depth of 2-3 mm in the submucosal plane to release the bands. Care was taken to limit the extent of the procedure only to the mucosal and the submucosal layers avoiding penetration into the deeper muscular layer. Fergusson’s mouth gag was used for forcible mouth opening leading to the fibers getting dissected and ruptured, resulting in an enhanced mouth opening.
Diode laser (940 nm) used for laser assisted fibrotomy.
The area as well as tip was swabbed with moist gauze to remove any debris and permit thermal relaxation of the tissue before commencing again with the procedure. In the literature, cases were done using lasers wherein a single large incision or an inverted “Y” incision was performed leaving a wide inter-incisional gap [1] but we employed a few modifications. We performed multiple transbuccal incisions parallel to one another (vertical and horizontal incision to form a check pattern) to release the bands [Table/Fig-4] enhancing the mouth opening immediately after the procedure [Table/Fig-5,6] LLLT (Low Level Laser Therapy) was given immediately after the procedure and also on follow ups after which patient reported to have less post-operative discomfort.
Intra-operative view (check pattern used for fibrotomy).

Post-operative view for case 1 showing enhanced mouth opening.

Post-operative view for case 2 showing enhanced mouth opening.

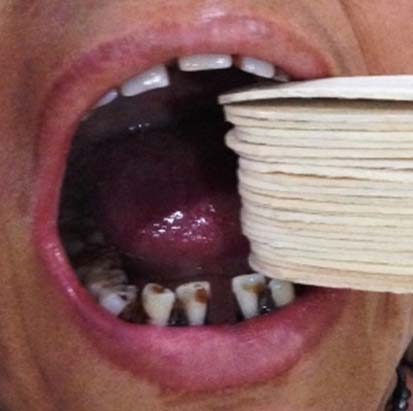
All the necessary post-operative instructions were given to the patients. The patients were advised oral physiotherapy by the use of a bunch of wooden ice-cream sticks (provided by us) for atleast 5 to 6 times daily [Table/Fig-7]. The number of sticks given for oral physiotherapy was eventually increased with number of days passing by. Analgesics were prescribed and the patients were instructed to use them if necessary. Further to supplement the benefits of the laser, a course of antioxidants was prescribed for both the patients. Both the patients were well motivated to leave the habit which was the main causative factor.
Post-operative physiotherapy.
Follow-up of both the patients revealed a mouth opening of 40 mm which was quite satisfactory even after a year. A detailed history after a year reported that both the patients had quit the habit since the time of treatment.
Discussion
The prevalence of OSMF cases in India has been reported to be in the range of 0.2 to 1.2% with a female to male ratio of 3:1.2. The risk of malignant transformation is about 7-13% [2,3]. Areca nut and its alkaloids have been implicated as the primary aetiological agent in the development of OSMF [4]. With the evolution of technology, researchers have focused on Lasers in the management of OSMF [5-7]. A modified technique for use of diode laser was implemented in our two cases, which is compared with the conventional technique as below:
Advantages of New Technique over Conventional Technique:
A single incision is deficient to cut all the fiber bands and may cause re-occurrence of trismus whereas in this technique we palpate the band and where ever it is required we perform the check pattern technique so as to make sure that we chopped the bands in all possible direction followed by use of Fergusson’s mouth gag which leads to dissection of any remaining bands.
2-3mm deep check pattern technique can be done in multiple areas in the mucosa where the fibrous bands are present.
Low laser power setting causes minimal damage to the tissue resulting in no delay in wound healing.
Rationale for the use of lasers for this procedure was photo-thermal action which resulted in disruption of the tissue by sufficient deposition of heat to vaporize the tissue. An important aspect regarding this can be explained from the fact that laser energy being selectively absorbed in the target tissue results in either a direct tissue cut (cold cut) or cause rupture (thermal cut) due to vaporization of the water within a cell, a process known as thermo-mechanical tissue ablation. This unique mechanism limits the amount of collagen damage to as little as 5 μm (approximately 2 cell widths), sparing the extracellular collagen matrix. Minimal post-operative pain and inflammation associated with the use of laser was reported due to less histamine release in tissues treated with laser. Additional benefits includes absence of scarring and minimal tissue shrinkage. Evidence from studies indicates that there was only 0.5 mm of tissue shrinkage attributed to a laser when compared to 3 mm with a Bard-Parker blade [8]. The procedure gives immediate mouth opening and immense post-operative benefits for the patient. Also, use of laser caused no wound dehiscence and no second site surgery was required to cover the raw area. Less scar formation leads to more supple and elastic mucosa, accounting for no recurrence or tissue shrinkage after surgery. In our case, follow-up period of one year showed no recurrence which to an extent can also be contributed to the discontinuation of the causative habit.
Just like every procedure, laser has its merits and demerits but the overall benefit of laser surgery surpasses the demerits of the conventional technique. Advantages of laser includes, a relatively bloodless operative field and thus excellent visibility, less chances of bacterial infection, reduced mechanical tissue trauma, quicker healing, and reduced post-operative edema, scarring and tissue shrinkage. At the same time, the possible complications in laser surgery can be excessive or collateral tissue damage due to misdirected usage.
Both of the cases are now kept under long-term follow-up for a longitudinal study.
Conclusion
It is a simple surgical procedure with effective results in the management of OSMF. More extensive studies involving a greater number of cases and proper study designs are required for a definitive outcome. Such promising results should encourage more widespread use of this new technique in the management of OSMF.
[1]. Shah A, Raj S, Rasaniya V, Patel S, Vakade M, Surgical management of oral submucous fibrosis with opus -5 diode laserJournal of Oral Laser Application 2005 5:37-43. [Google Scholar]
[2]. Murti PR, Bhonsle RB, Pindborg JJ, Daftary DK, Gupta PC, Mehta FS, Malignant transformation rate in oral submucous fibrosis over a 17-year periodCommunity Dent Oral Epidemiol 1985 13(6):340-41.as sited from https://doi.org/10.1111/j.1600-0528.1985.tb00468.x10.1111/j.1600-0528.1985.tb00468.x3866655 [Google Scholar] [CrossRef] [PubMed]
[3]. Tilakaratne WM, Klinikowski MF, Saku T, Peters TJ, Warnakulasuriya S, Oral Submucous fibrosis: Review on aetiology and pathogenesisOral Oncol 2006 42:561-68.10.1016/j.oraloncology.2005.08.00516311067 [Google Scholar] [CrossRef] [PubMed]
[4]. Murti PR, Bhonsle RB, Gupta PC, Daftary DK, Pindborg JJ, Mehta FS, Etiology of oral submucous fibrosis with special reference to the role of areca nut chewingJ Oral Pathol Med 1995 24:145-52.10.1111/j.1600-0714.1995.tb01156.x7783003 [Google Scholar] [CrossRef] [PubMed]
[5]. Nayak DR, Mahesh SG, Pavithran P, Pujary K, Pillai S, Role of Ktp-532 Laser in management of oral submucous fibrosisThe Journal of Laryngology and Otology 2009 123:418-21.10.1017/S002221510800364218845031 [Google Scholar] [CrossRef] [PubMed]
[6]. Chhaya VA, Sinha V, Rathor R, Modi N, Rashmi GS, Parmar V, Oral submucous fibrosis - surgical treatment with CO2 laserWorld Articles in Ear, Nose and Throat 2010 3:1-2. [Google Scholar]
[7]. Chaudhary Z, Verma M, Tandon S, Treatment of oral submucous fibrosis with Er, Cr: YSGG laserIndian J Dent Res 2011 22:472-74.10.4103/0970-9290.8707322048591 [Google Scholar] [CrossRef] [PubMed]
[8]. Chaudhary Z, Verma M, Tandon S, Treatment of oral submucous fibrosis with Er, Cr: YSGG laserIndian J Dent Res 2011 22:472-74.10.4103/0970-9290.8707322048591 [Google Scholar] [CrossRef] [PubMed]