Tuberculosis (TB) is a global public health crisis. As per the Global TB Burden report published by World Health Organization, there were 6.3 million reported new cases of TB in 2016 [1]. TB is the ninth leading cause of death worldwide and is obviously the leading cause of death from a single infectious agent ranking above HIV/AIDS [1]. Most of the deaths due to TB can be prevented with the help of early diagnosis and treatment. It is reported that millions of TB cases are successfully diagnosed and put on treatment averting millions of deaths which accounted to 53 million from 2000 to 2016 however, there are still large gaps in detection and treatment [1]. The current TB diagnosis and detection tool ranges from a 100-year-old microscopic technique to the newest form of molecular techniques [2]. In India at program level, the diagnosis of TB is done either through sputum smear microscopy or through a rapid molecular test through a chain of three tier laboratory network [3]. These consist of National Reference Laboratories, Intermediate Reference Laboratories, Culture and Drug Susceptibility Test (DST) Laboratories, Cartridge Based Nucleic Acid Amplification Test (CBNAAT) Laboratories and Designated Microscopy Centres (DMC) [3]. However, the TB diagnostic pattern in private sector does not really follow any pattern and is based primarily on the choice of the concerned physician who renders services to a wide range of patients that seek medical care at the private sector health care in India. In addition to the physicians’ choice and preference for a particular test, there exists a market mindset which also governs the usage of certain diagnostic tools for TB diagnosis in India. With this backdrop, a cross sectional study was conducted to understand the pattern and usage of the TB diagnostic procedures adopted by the private sector across three cities of Chhattisgarh. Albeit information on a wide range of services for TB diagnosis has been collected however, the article primarily focused on discussing about the significance of commercial sero-diagnosis, sputum microscopy and CXR owing to certain limitations.
Materials and Methods
Seven months (June 2016 to December 2016) data on various pathological and radiological tests advised for TB diagnosis were collected from selected leading laboratories across three cities of Chhattisgarh. The number of laboratories contacted in three cities; Bilaspur, Durg & Bhilai and Rajnandgoan include six, six and three respectively.
Results
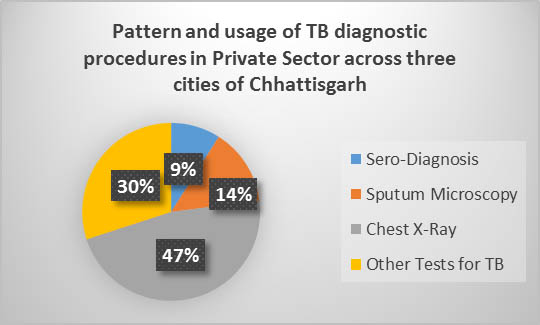
Apart from sputum microscopy, adopted by RNTCP, various other diagnostic procedures are found to be practiced in these three cities, as listed in [Table/Fig-1]. These tests include ADA for TB, FNAC, Abdominal USG, CXR, IGM and serological tests such as TB Gold. A particular pattern could not be observed across these three cities and medical practice for TB in these cities has preference of some tests over the other. Similarly among all the tests 9.4%, 13.4%, 46.7% and 30.3% (n=3295) are serological tests, sputum microscopy, CXR and other tests respectively across all the cities, as represented in [Table/Fig-2].
List of different test carried out for TB in three different cities of Chhattisgarh, India (from June 2016 to December 2016).
| Name of the City | Types of investigation for TB |
|---|
| Sero-Diagnosis | Sputum Microscopy | Chest X-Ray | Others | Total |
|---|
| Bilaspur | 68 (20.48%) | 40 (12.04%) | 49 (14.75%) | 175 (52.71%) | 332 |
| Durg & Bhilai | 186 (11.52%) | 403 (24.96%) | 245 (15.17%) | 780 (48.32%) | 1614 |
| Rajnandgoan | 59 (4.37%) | 00 | 1245 (92.29%) | 45 (3.33%) | 1349 |
| Total | 313 (9.4%) | 443 (13.44%) | 1539 (46.70%) | 1000 (30.34%) | 3295 |
# Others include ADA TB, FNAC, Abdominal USG, IGM
Pattern of usage of TB diagnostic procedures.
Discussion
The study assessed the pattern and usage of TB diagnostic procedures in private sector across three cities of Chhattisgarh. It was observed that the most common approach to TB diagnosis in private sector is the use of CXR followed by other methods, sputum microscopy and sero-diagnosis in a descending order. In addition, it has also been observed that one of the cities has over reliance on CXR for the diagnosis of TB. The private practitioners’ preference on the usage of CXR is attributed to two important factors; personal choice and market demand. There are many studies which suggest that private practitioners have special interest in advising CXRs for the diagnosis of TB in India [4]. In addition, the beneficiaries also expect the practitioners to advice for CXRs for the diagnosis of TB as they believe CXRs as an important and sophisticated tool for TB diagnosis compared to sputum microscopy. However, CXR, many a time, is believed to be the major fuelling factor for irrational therapy and Drug Resistant-TB [5]. However, the recent RNTCP -2016 guideline suggests that the Sputum Microscopy and Chest-X-ray should be performed together in order to ascertain the diagnosis of TB. The guideline has not endorsed the use of CXR as a single tool for TB diagnosis as practiced in private sector in which private practitioners diagnose TB cases purely on the basis of CXR. The recent guideline clearly states that if the sputum smear is negative and CXR is suggestive of TB, then a second sample should be subjected to sputum microscopy and CBNAAT simultaneously to ascertain TB, thus completely ruling out the use of CXR as the only tool for TB diagnosis [6]. It has been further suggested by studies that CXRs form excellent screening tools instead of upfront diagnostic tools in case of TB diagnosis [2].
In addition to this, it has also been observed that a substantial proportion of private practitioners prefer commercial sero-diagnosis as the tool of diagnosing active TB. Serological tests are the kind of tests that are performed to detect active TB based on the antibodies elicited by antigens of Mycobacterium tuberculosis recognised by the humoral immune response system. Most of these serological tests use ELISA (Enzyme Linked Immuno Sorbent Assay) formats while others use rapid tests such as immune-chromatographic and lateral flow analysis [7]. Thus, the faster and rapid delivery of results by these serological tests make them attractive compared to sputum based diagnostic tests [8]. However, one of the systematic reviews carried out on the commercial serological tests reveal that the results are inconsistent and of low quality [9]. Despite Government of India’s ban on sero-diagnosis, these tests are being widely used by the private sector in India [10]. Furthermore, none of the international guidelines support the use of serological tests for the diagnosis of active TB [11], but a rampant usage of these tests by the private sector is being observed in developing countries including India and 16 of 21 other high-burden countries in the world [12]. It is estimated that 1.5 million serological tests are being performed alone in India every year by the private sector for the diagnosis of active TB in India. The cost has been estimated at US $15 million (825 million INR) per year [13]. According to the reports of a cost-effectiveness modeling study serological tests, if used in the place of sputum microscopy, would increase the costs of TB control program in India approximately by 4-fold and result in 102,000 fewer disability-adjusted life years (DALY) averted and 121,000 more false-positive diagnoses and 32,000 more secondary infections [14]. In 2011, WHO issued a policy statement mentioning that serological tests provide inconsistent and imprecise estimates of sensitivity and specificity. Further, there is no evidence that these commercial serological tests improve patient outcomes and high proportions of false-positive and false-negative results adversely impact patient safety [15]. As per the findings of different systematic reviews and meta-analysis [9,14], no serological test can really match with the performance of sputum microscopy. Thus, the usage of these tests at private sector should strongly be discouraged and the private practitioners should personally avert themselves in relying on these tests for the diagnosis of active TB cases. Most importantly these tests do more harm than benefit to the patient community by providing false positive or false negative results. Mimicking the steps taken by Indian Academy of Paediatrics which strongly discourages the usage of serological tests, other professional bodies should also come forward to discourage the usage of serological tests for the diagnosis of active TB in India [16].
It was further observed that despite the emphasis of National TB control program on sputum microscopy in India, not a single test of sputum microscopy was seen to be carried out in the same city, where the practice of CXR for TB diagnosis was high, during the seven month period. To stop the malpractice on TB diagnosis, the private sector should adhere to the Standards of Tuberculosis Care in India guidelines developed jointly by World Health Organization and Govt. of India [5,17,18]. In addition a range of other investigational measures are also being used for TB diagnosis accounting to 30.3% of the total procedures followed, the utility of which in routine clinical practice is also questionable.
Limitation
The study assessed the pattern and usage of TB diagnostic services used for the purpose of diagnosing TB in private sector based on the reports obtained from different private laboratories conducting these diagnostic procedures. However the study could not audit the prescriptions of the private practitioners suggesting these TB diagnostic procedures. Thus, it could only discuss tests that are most commonly used without specific indications such as CXR, Sputum Microscopy and sero-diagnosis. The suitability and rationality of other diagnostic procedures can only be found out if the prescription audit is carried out which has not been done in this study. An example can explain this limitation; ADA is carried out in some specific situation such as, pleural effusions to ascertain Tuberculous Pleuritis [19] and ascetic fluid to ascertain Peritoneal Tuberculosis [20,21], thus assessing the use of ADA in case of TB diagnosis without auditing prescription would be difficult. The same is applicable to other tests as well. In addition the study could have also assessed the significance of adhering to clinical guidelines by the private practitioners however, it was beyond the scope of this study and a separate qualitative approach in order to assess the same can be planned by other researchers.
Conclusion
Early detection and effective treatment can reduce the TB mortality in India, however, if the detection of TB through different diagnostic tools is not rational then the repercussion of the same would be disastrous. There are effective approaches available and guidelines on diagnosis and treatment ably guide the private practitioner for diagnosis and treatment however, adoption of standard treatment guidelines, such as Standards of Tuberculosis Care in India (STCI) guideline is very poor among the private practitioners in India. Thus cooperation of private sector for TB care and control in needed in India and is also the vision of National Strategic Plan for TB however, the same is only possible if the sector stops malpractice and adheres to standard guidelines.
# Others include ADA TB, FNAC, Abdominal USG, IGM