Successful Management of Traumatic Rupture of the Inferior Rectus Muscle
Teena Mariet Mendonca1, Gurudutt M Kamath2
1 Senior Resident, Department of Ophthalmology, Kasturba Medical College, Manipal University of Higher Education, Mangalore, Karnataka, India.
2 Professor, Department of Ophthalmology, Kasturba Medical College, Manipal University of Higher Education, Mangalore, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Teena Mariet Mendonca, Senior Resident, Department of Ophthalmology, Kasturba Medical College Hospital, Attavar, Mangalore-575001, Karnataka, India.
E-mail: tmendonca87@gmail.com
A 25-year-old male patient presented with diplopia after a penetrating injury to the right eye. Examination revealed right hypertopia and limitation of infraduction of right eye with rupture of Inferior Rectus (IR) muscle and conjunctival tear. Computed Tomography (CT) of the orbits did not reveal any remarkable findings. Immediate surgical exploration was done and IR was retrieved and anastomosis was carried out. On follow-up after two months postoperatively, he was free of diplopia and had normal infraduction and no vertical strabismus.
Injury, Oculomotor muscles, Orbital trauma
Case Report
A 25-year-old male patient presented with the history of an injury to the right eye with sharp iron rod on the previous day from the day of presentation. He complained of redness, pain in the right eye and vertical diplopia.
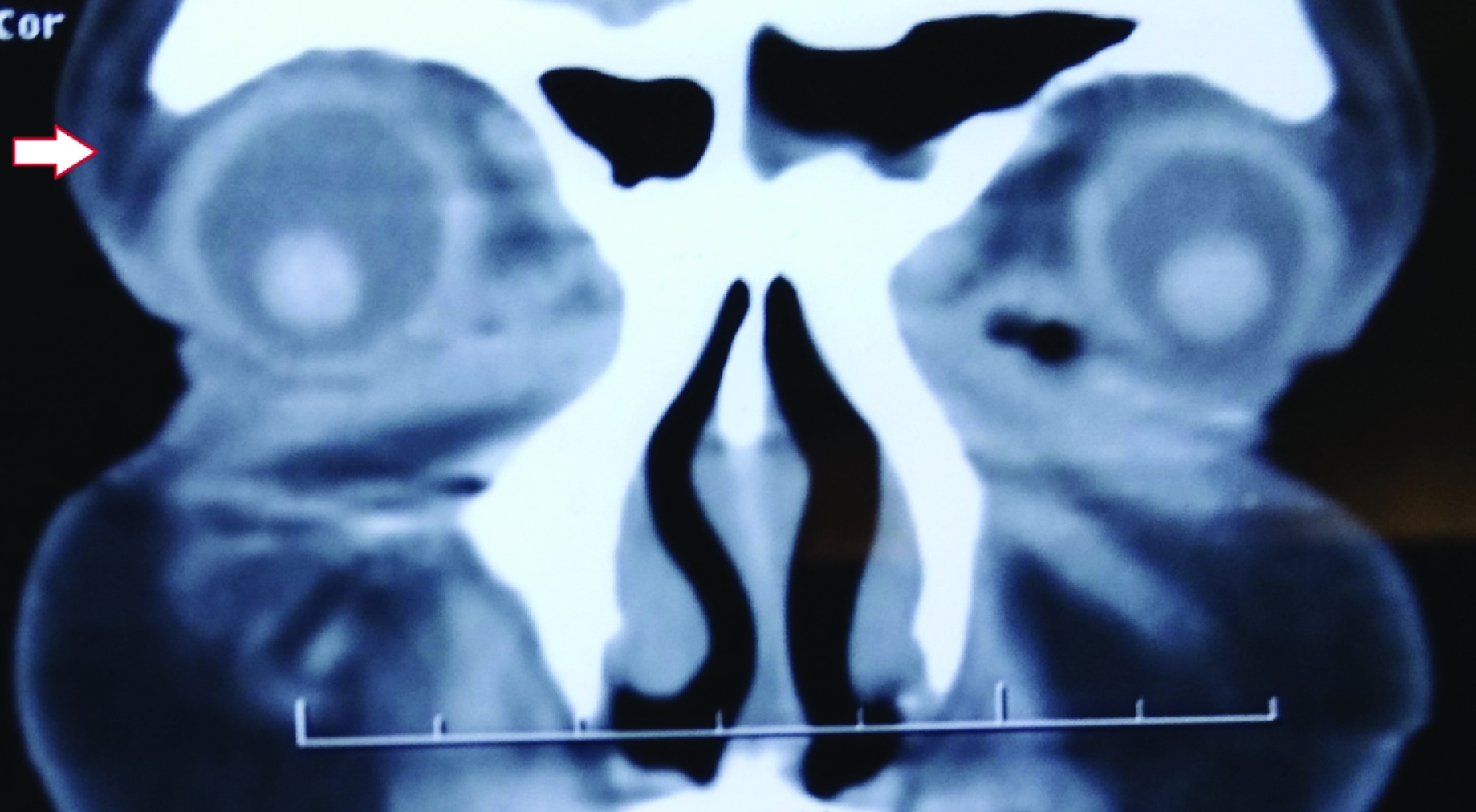
On examination, his best corrected visual acuity was 6/18 in right eye and 6/6 in the left eye. Refraction was Plano in both eyes. He had 18 Prism Dioptres (PD) of exotropia and 35 PD of right hypertropia on modified Krimsky test [1]. Examination of extraocular motility revealed -4 limitation of infraduction and dextro-depression of right eye [Table/Fig-1]. Periorbital ecchymosis and injury to eyelids was not present. A linear horizontal conjunctival laceration was present 8 mm from inferior limbus, measuring about 10 mm in length. A torn stump of IR muscle was visible at the insertion suggestive of full thickness laceration of IR. No sclera or corneal injury was noted. There was no periorbital ecchymosis or step deformity of orbital rim. Anterior segment evaluation was normal except for efferent pupillary defect of right eye. Fundus examination was within normal limits. Left eye examination was unremarkable. Computed tomography of the orbit revealed periorbital oedema [Table/Fig-2]. Bony orbital walls were intact with no fractures. Patient was taken up for right eye IR laceration repair under local anaesthesia (peribulbar block). Intraoperative forced duction test was negative. Thorough search for distal end of IR was done, few fibers were identified, retrieved and end to end suturing was done with proximal fibers with 6-0 polygalactin suture material. Conjunctival resection was done and conjunctiva was sutured with 8-0 polygalactin sutures. On postoperative Day1, he had persistent diplopia with -2 limitation of infraduction. He had 20PD exotropia with 15PD right hypertropia. He was treated with topical steroid and antibiotics with systemic anti-inflammatory drugs. On follow-up, after two months postoperatively, he was free of diplopia. Extraocular motility was full in right eye with no limitation of movements [Table/Fig-3]. He had 10PD of intermittent exotropia and no vertical deviation. Conjunctival wound had healed well.
Right eye hypertropia along with -4 limitation of infraduction and dextro-depression and levo-depression. Overhanging lacerated inferior conjunctiva can be noted.

CT orbit of the patient showing mild periorbital oedema with no other abnormalities
Nine gaze photographs of the patient after two months following surgery showing normal extraocular motility and absent vertical strabismus.

Discussion
Orbital trauma is associated with various periorbital and ocular injuries. Diplopia is a common occurrence due to orbital wall fractures and incarceration of Extraocular Muscles (EOM) in fracture site. Other causes of diplopia are flap tear of extraocular muscle or palsy of a cranial nerve. Rupture of extraocular muscle is usually associated with penetrating trauma to the orbit. Rupture or loss of EOM requires urgent surgical intervention and it is quite challenging to the surgeon.
Traumatic extraocular muscle injuries are more frequently seen in cases of orbital wall fractures caused by blunt orbital trauma [2]. Penetrating injuries result in direct muscle trauma causing contusion or rupture of EOM. Complete rupture of EOM is infrequently seen. Rectus muscles are more susceptible to injuries when compared to oblique muscles due to anatomical predisposition [3]. Due to exposure during Bell’s phenomenon, inferior and medial rectus muscles are more commonly involved [4]. Disinserted or severed muscles are more commonly seen after strabismus and scleral buckling surgeries.
Preoperative imaging plays a vital role in planning the management of orbital injuries. CT orbits with 0.5 mm cuts reveals orbital wall fractures and associated muscle injury.
Repair of ruptured or lost extraocular muscle is very challenging to the surgeon. Every attempt should be made to retrieve the proximal segment through the attachments to intermuscular septum. Superior, inferior and lateral rectus muscles can be found in the Sub-Tenon’s space by their septal attachments to adjacent oblique muscles. Though the recuts muscles might be completely severed due to the trauma, the detached muscles are usually held by check ligaments and intermuscular septum which are of great help to the surgeons [5]. During exploration, it is advocated that surgeon should not jerk the eye in opposite direction which may lead the muscle to recoil back in the orbit through Tenon’s capsule. Instead, eye should be retro placed against opposite orbital wall and thorough search is done in the Tenon’s capsule [6].
There are reports of IR rupture due to blow out fracture of orbital floor [7]. In our case, no other orbital injury was noted except for ruptured IR. The patient had severe vertical diplopia due to induced vertical strabismus. Intraoperatively, complete transection of IR was noted just beneath the site of conjunctival laceration and severed muscle stump was visible at the insertion site. We went ahead with immediate exploration; hence we could achieve partial retrieval of IR which was sutured to distal stump. We also performed conjunctival resection in addition to the muscle anastomosis. On follow-up after six weeks post operatively, our patient was free of diplopia with normal infraduction and no vertical strabismus.
Lando L et al., have described a case similar to our case, however, they have performed preoperative forced duction testing which we preferred not to do; because, undue manipulation can lead to retraction of the ruptured proximal segment of the muscle in to the orbit which is not desirable [8].
Patient consent for this case report was obtained.
Conclusion
Here, we have described a case of isolated IR rupture due to orbital trauma and its successful surgical management by anterior conjunctival approach. Early exploration and surgical repair aims at restoring anatomical integrity of extraocular muscles which results in better structural and functional outcomes.
[1]. Mehta A, Chief complaint, history and physical examination. In: Rosembaum A (ed)Clinical Strabismus Management 1999 Philadelphia PAWB Saunders:03-21. [Google Scholar]
[2]. Sloan B, McNab AA, Inferior rectus rupture following blowout fractureAust N Z J Ophthalmol 1998 26:171-73.10.1111/j.1442-9071.1998.tb01537.x9630302 [Google Scholar] [CrossRef] [PubMed]
[3]. Godeiro KD, Teixeira AG, Souza JP, Noriega AM, Nakanami CR, Traumatic tear of the inferior rectus muscle treated with inferior oblique anterior transpositionInt Ophthalmol 2005 26:185-89.10.1007/s10792-007-9035-z17286186 [Google Scholar] [CrossRef] [PubMed]
[4]. Paysse EA, Saunders RA, Coats DK, Surgical management of strabismus after rupture of the inferior rectus muscleJ AAPOS 2000 4(3):164-67.10.1016/S1091-8531(00)70007-3 [Google Scholar] [CrossRef]
[5]. Murray AD, An approach to some aspects of strabismus from ocular and orbital traumaMiddle East Afr J Ophthalmol 2015 22(3):312-19.10.4103/0974-9233.15973226180469 [Google Scholar] [CrossRef] [PubMed]
[6]. Parks M, Slipped, disinserted or severed, and lostmuscles. In: Rosembaum A (ed)Clinical Strabismus Management 1999 WB SaundersPhiladelphia PA:529-53. [Google Scholar]
[7]. Tomasetti P, Metzler P, Jacobsen C, Isolated inferior rectus muscle rupture after blunt orbital traumaJ Surg Case Rep 2013 2013(9):rjt076Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3813725/10.1093/jscr/rjt07624963904 [Google Scholar] [CrossRef] [PubMed]
[8]. Lando L, Oliveira T, Rezende JC, Inferior rectus muscle rupture due to orbital traumaRev bras oftalmol 2017 76(1):40-42.Published online Jan./Feb. 2017. Available from: http://dx.doi.org/10.5935/0034-7280.2017000910.5935/0034-7280.20170009 [Google Scholar] [CrossRef]