Platelets play a critical role in normal haemostasis, where they stop bleeding by clumping and forming plugs at the site of blood vessel injuries. Platelet count estimation is a basic hematological investigation. Various methods used for platelet count estimation include, examination of stained peripheral blood smears, phase contrast microscopy using haemocytometer, automated cell counters and fluorescent labeling techniques [1-3]. Amongst these, the most frequently used method is the manual count of platelets using stained smears [4]. However, stained smears have certain limitations, such as suboptimal staining quality and stain precipitates may cause difficulty in estimation of accurate platelet count. Besides this, the staining techniques are time consuming which further delays platelet evaluation. In present era, automated blood cell counter has largely replaced the manual method of platelet counting, but it also has its own limitations like cost, quality assurance and their unavailability in small peripheral centers [2,5]. Finding out accurate platelet count in Grade 3 and 4 thrombocytopenia is crucial in clinical practice to facilitate decisions for prophylactic or therapeutic platelet transfusion. All the abnormal platelet values generated by the cell counters require confirmation by manual examination of stained peripheral blood smear [6]. To the best of our knowledge, only two studies have been published in literature regarding the estimation of platelet count on unstained smears [7,8]. Hence, we planned to use unstained peripheral blood smear for platelet count estimation which is less time consuming to assess whether it can be used to detect the platelet count in emergency situations like dengue period when workload is more. The objectives of the present study were to compare the platelet count on unstained and stained peripheral blood smear and to compare the advantages and disadvantages of these two methods.
Materials and Methods
The present comparative study was conducted in University College of Medical Sciences and Guru Teg Bahadur Hospital, Delhi, India, in August and September 2016. A total of 500 venous blood samples in Ethylene Diamine Tetraacetic Acid (EDTA) vacutainer, received in Outpatient Department (OPD), were included in the study. Each sample was given a unique numeric identifier with no personal identifying information. An extra peripheral blood smear was prepared from the blood sample on a clean glass slide besides the slide prepared for routine reporting within three hours of collection. The unstained smears were scanned under 10X objective and 40X objectives to choose an ideal area (where RBCs were uniformly spread) for platelet count. A circular area of about 2-3 mm in diameter was marked on the back side of smear in the chosen area using a diamond pencil. Then the smear was examined under 100X objectives without placing immersion oil. The condenser of microscope was lowered and the iris diaphragm was closed allowing minimum light to pass. Platelets were counted in 10 fields and the average number of platelets per field was calculated in marked area. Platelet count per micro liter was calculated by multiplying the average number of platelets per field by 20,000. The same smear was stained using Wright’s stain and the area marked with diamond pencil prior to staining was examined under light microscope using 100X objective and immersion oil. Average number of platelets per Oil Immersion Field (OIF) was multiplied by 20,000 to get platelet count estimate per micro litre (μL) [9].
Two pathologists independently counted the platelets separately both in unstained and stained slides blinded to each other’s findings. Number of platelets was compared between unstained slides and stained slides. Study was conducted after obtaining clearance from the Institutional Ethics Committee.
Statistical Analysis
Statistical analysis was done using intra class correlation coefficient.
Results
In unstained smears platelets appeared as refractile and round structures while in Wright stained peripheral blood smear they were seen as blue to purple colour body. Based on the average number of platelets per 10 fields (×1000 magnification) in stained peripheral blood smears, 500 cases were categorised into four classes [Table/Fig-1].
Classification of cases according to average number of platelets per 10 field under oil immersion in stained peripheral smears (n=500).
| Class | No. of platelets on stained slides | No. of cases | Percentage of cases |
|---|
| 1 | 0-10 | 190 | 38% |
| 2 | 11-20 | 177 | 35.4% |
| 3 | 21-30 | 122 | 24.4% |
| 4 | >30 | 11 | 2.2% |
On the basis of present division, p-value and agreement between unstained and stained smears were assessed using ICC [Table/Fig-2].
Intra-class correlation coefficient and p-value of four classes in unstained and stained smears.
| Class | ICC | p-value |
|---|
| 1 | 0.995 | 0.0001 |
| 2 | 0.993 | 0.0001 |
| 3 | 0.947 | 0.0001 |
| 4 | 0.511 | 0.001 |
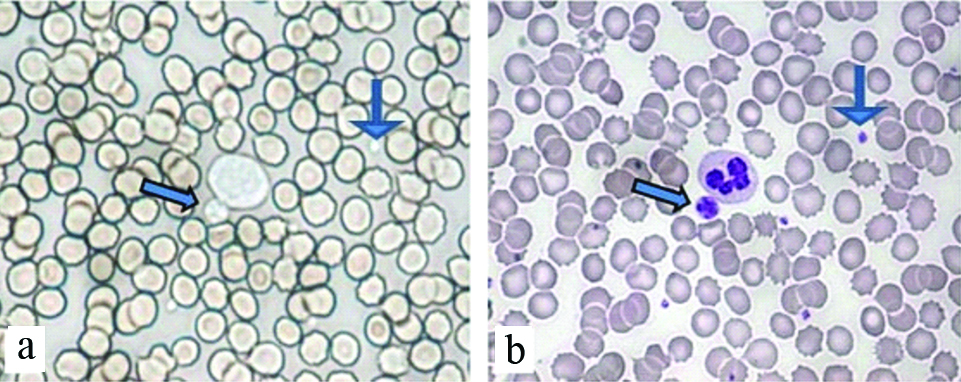
Excellent agreement was noted in Class 1 (0.995) while in Class 4 it was average (0.511). A p-value of less than 0.05 was considered as statistically significant. As far as platelet size is concerned, large platelets were identifiable but micro platelets were not recognised easily on unstained smears [Table/Fig-3a,b].
a) Unstained smear shows refractile, round platelets and a giant platelet sitting in the vicinity of a white blood cell (Unstained smear, 100X); b) Findings confirmed on smear stained with Wright stain by comparing the same area (Unstained smear, 100X).
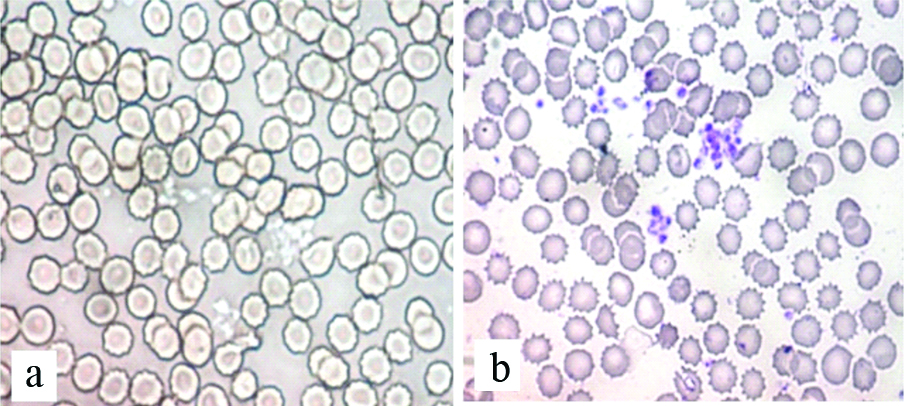
Platelet clumping could also be appreciated in most of the cases on unstained smears [Table/Fig-4a,b].
a) Unstained smear shows presence of three variable size clumps of platelets (Unstained smear, 100X); b) Smear stained by Wright stain further confirmed the findings (Unstained smear, 100X).
The cases with discrepant results of platelet count on unstained smears in comparison to stained smears are shown in the [Table/Fig-5].
Difference in number of platelet count per 100X in unstained smears in comparison with stained smears.
| Difference in the number of platelet count/100x between stained and unstained smears | Higher number of platelets in unstained smears (No. of cases) | Lower number of platelets in unstained smears (No. of cases) |
|---|
| 1 | 9 | 19 |
| 2 | 5 | 9 |
| 3 | 5 | 7 |
| 4 | 3 | 4 |
| 5 | 2 | 5 |
| 6 | 1 | - |
| Total | 25/500 cases | 44/500 cases |
Out of 500 cases, in unstained smears 25 cases had higher and 44 cases had lower platelet count in comparison with stained smears. The comparison of advantages and disadvantages of platelet estimation using unstained and stained peripheral blood smears are summarised in [Table/Fig-6].
Comparison between estimation of platelet count using unstained and stained peripheral smears.
| Parameters | Unstained smear | Stained smear |
|---|
| TAT | 2-4 minutes | 15-20 minutes |
| Cost effectiveness | No staining required, hence cost-effective | Comparatively costly |
| Stain artifacts | No stain artifact | Stain artifacts and poor staining quality leading to poor preservation of morphology |
| Reliability | It is useful in certain conditions where the platelet count is urgently required In thrombocytopenic blood disorders, it gives reliable values but it does not show good agreement where platelet count is high
| Reliable as visual evaluation from a stained smear clearly differentiates platelets and non-platelet particles in contrast to unstained smears and most automated counters In addition, the original smear can be preserved and re-evaluated
|
| Labour intensive | Easy to perform, less labour intensive | Labour intensive as staining of smears is required Repeat smear and staining is required in cases with staining artifacts
|
| Usefulness | It has short TAT and is less labour intensive hence it can be used as a screening test in certain circumstances like in dengue outbreaks and bleeding disorders where the platelet count is the basic and mandatory investigation Number of platelets, morphology of platelets, giant platelets, platelet clumping and platelet superimposed on RBCs can be recognised with expertise Its usefulness is much in rural centers where resources are limited
| In a well stained smear platelet clumping and micro platelets can be easily differentiated from other dust particles Wherever platelet count is low on automated counter findings must be cross checked using stained smears as gold standard
|
Discussion
The use of unstained smear has been largely limited to the examination of urine, semen, vaginal smears and other body fluids [10-12]. Examination of stained smears for platelets which is considered gold standard for platelet count has its own limitations. Stain artifacts, improper staining and poorly preserved morphology on stained smear interfere in platelet counting and require repeated smear preparation which delays the report. Since, the manual method of platelet counting is time consuming and cumbersome, it is now replaced by automated blood cell counter. However, all abnormal platelet counts must be cross checked by examination of stained blood smears [4]. On unstained peripheral smear platelets can be easily identified owing to their refractile nature.
In the present study, 44 out of 500 cases showed falsely low platelets and this may be due to the presence of micro platelets which are difficult to recognise in unstained smears. Platelets were overestimated in unstained smears in 25 cases and this could be due to counting the refractile dust particles. However, expertise in examining the unstained peripheral smears might further reduce the number of cases with discordant results between unstained and stained peripheral smears.
Umashankar T et al., in their study found that platelet clumping could not be identified on unstained smears and no comments on platelet morphology were made in their study [7]. However, in present study we were able to comment upon these parameters as platelet clumping was appreciated in most of the cases on unstained smears where it was present in stained smears. Also, the platelets superimposed on RBCs appeared as round and refractile body over non refractile RBCs. As far as platelet morphology is concerned, large platelets were identified but there was problem in identification of micro platelets which may be the cause of low platelet count in most of the cases.
In a study by Muthu S et al., no significant difference was found in platelet counts between unstained peripheral smears and stained smears. Hence, they concluded that platelet count estimation using unstained peripheral smears is a good preliminary method and can be used where round the clock laboratory facilities are not available, particularly in rural areas [8].
In the present study, we found that platelet count by unstained peripheral smear has short Turn-Around Time (TAT) of 2-4 minutes as compared to 15-20 minutes by stained smear technique. Hence, unstained smears may be used as an initial screening method whenever there is a large sample load such as in dengue outbreak which can greatly reduce the TAT. Unstained smear examination is rapid, cost effective, reliable, and easy to perform. The problems faced due to poor staining quality are also curtailed.
Limitation
There was also some limitations of the present study that the estimation of platelet count on unstained smears efficiently and accurately requires training and more expertise compared to present stained smears.
Conclusion
Platelet count estimation using unstained smears has good correlation with platelet count estimated by stained smears especially in conditions where the platelet counts were low (thrombocytopenia). Hence, use of unstained peripheral smears for platelet estimation can be used in situations like dengue outbreaks when workload is more and where laboratory facilities are not available round the clock. Also, it greatly reduces the TAT, requires less manpower and is cost-effective.