Introduction
Tuberculosis (TB) is a major health problem in both developing and developed countries. With the introduction of antituberculous treatment regimens, there was a fall in the incidence of TB. However, a re-emergence of the disease occurred with the pandemic of Acquired Immuno-Deficiency Syndrome (AIDS) and development of Multi-Drug Resistant (MDR) forms of TB.
Extrapulmonary TB occurs in approximately 20% of the patients with TB. Of that, musculoskeletal TB occurs in 1-3% [1]. Spondylitis constitutes 50% of the cases, followed by peripheral arthritis in 30%, osteomyelitis in 19% and tenosynovitis, bursitis and Poncet disease in the remaining 1% [2,3].
Mycobacterium tuberculosis is the main causative organism. The disease occurs following reactivation of dormant bacilli disseminated in the bones following initial mycobacteremia of primary infection. Primary foci are usually lung, kidney, lymph node or other viscera. Less commonly, Mycobacterium bovis and Non-Tubercular Mycobacteria (NTM) cause osteo-articular TB [4,5].
Modes of spread of Mycobacterium tuberculosis are by haematogenous route from the primary foci, contiguous spread to neighbouring bones and joints from adjoining tissues of direct inoculation, spread to joints directly through the subsynovial vessels or indirectly through the epiphyseal or metaphyseal arteries. NTM usually occurs following direct inoculation following trauma or surgical procedures [4-6].
Though, musculoskeletal TB constitute only a meagre 1-3% of the tuberculous infections, it causes significant morbidity to the affected population not only because of the disease per se but also because of the considerable delay in the diagnosis. Due to its indolent nature, affected populations present later in the course of the disease. Tuberculosis is also considered a ‘great mimicker’ with often atypical radiological findings and equivocal serological markers. An array of clinical conditions mimics the clinical and radiological features of musculoskeletal TB, often adding to the delay in the correct diagnosis and initiation of treatment. Clinical and radiological features of the extraspinal osteoarticular TB have been recapitulated in this review with illustrations. Radiological features and practical points of difference of the clinically relevant mimickers of the musculo-skeletal TB have been summarised.
Diagnosis
Confirmation of Acid Fast Bacillus (AFB) from body fluid like the synovial fluid still remains the gold standard for the diagnosis of TB. Preferably, two or three samples should be collected. Ziehl Neelsen stains reveals AFB only if the sample contains greater than 10000 bacilli/mL. In paucibacillary states, culture medium like the Lowenstein Jensen medium, radiometric and non radiometric techniques can be used for diagnosis [2].
Features of Tuberculous Arthritis
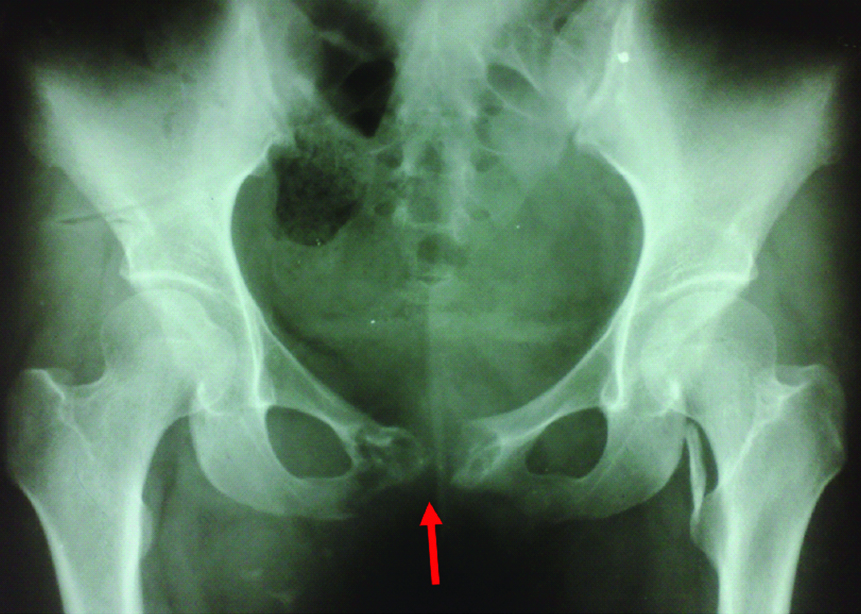
Clinical features and plain radiographic findings: Tubercular arthritis is usually monoarticular with insidious onset. Symptoms usually include chronic joint pain, restriction of joint motion with lack of constitutional symptoms. Chronic cases may present with wasting of muscles and deformity. Sometimes, cold abscess may be the first presentation. No joint or bone is immune from tuberculosis [7,8]. Tubercular arthritis usually involves appendicular joints like hip and knee joints. Tuberculosis of the pelvic girdle usually affects the sacroiliac joint and less frequently ilium, ischium and pubic symphysis [Table/Fig-1] [8].
A 45-year-old lady with tuberculosis of pubic symphysis. AP radiograph of pelvis shows pubic diastasis with destruction of pubic symphysis and erosion of adjoining pubic bones and right ischio-pubic ramus. Minimal sclerosis of the margins noted. No periosteal reaction is seen. Incidental note was made of calcification of left ilio-psoas tendon near lesser trochanter.
Tubercular arthritis has to be differentiated from Poncet’s disease or tubercular rheumatism. The latter is considered as a reactive arthritis associated with tuberculosis. It is typically a non destructive polyarthritis that occurs during an episode of acute TB infection. The cause is unknown. There is no evidence of infection of joints by the organism. On the other hand, tubercular arthritis tends to be monoarticular in most of the times with infection of the joint by mycobacterium and the organism can be isolated from the joint fluid [9].
Tubercular arthritis has been classified into five stages. Stage I is the synovitis stage. It clinically presents as soft tissue swelling surrounding the involved joint. Its radiographic features are localised osteoporosis and soft tissue swelling. Prognosis after treatment is excellent. Stage II is the early arthritis stage. Radiographic features are the marginal erosions of lytic lesions with mild diminution of joints space. Prognosis after treatment is good with mild stiffness. Stage III is the stage of advanced arthritis with subchondral and subperiosteal cysts with loss of joint space. Stage IV is the stage of more advanced arthritis with gross joint destruction. Stage V is the stage of ankylosis of joint [2].
Phemister triad is classically seen in tubercular arthritis. It is the triad of juxtaarticular osteopenia/osteoporosis, peripheral bony erosions and gradual narrowing of joint space [10,11].
Marks and McHenry divided tubercular arthritis based on the severity of disease [12]:
Class I - Infection of synovium with little or no bony involvement.
Class II - Infection of synovium and bone with preserved joint space.
Class III - Extensive osseous and synovial involvement and progressive loss of joint space.
Class IV - Tuberculous arthritis of any stage with superimposed pyogenic infection.
Ultrasound comes handy in confirming joint effusion and in guided aspiration of joint fluid for diagnosis. It is useful in characterizing soft tissue swelling remote from the joint. It demonstrates the fluid nature of the swelling and helps in detecting abscesses. Sometimes, it can be traced back to the affected neighbouring bones and joints.
Computed Tomography (CT) and Magnetic Resonance Imaging (MRI)
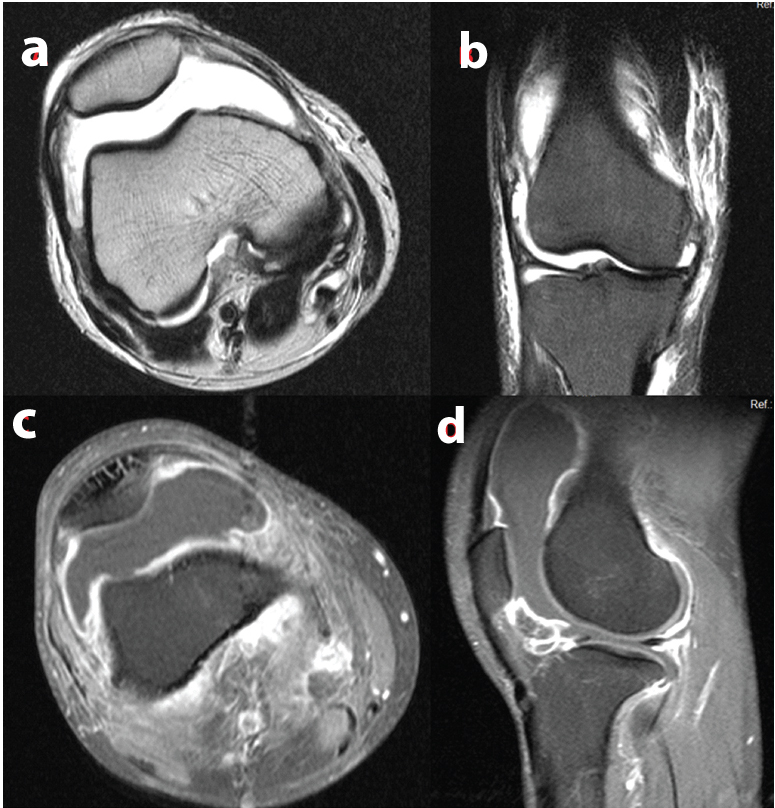
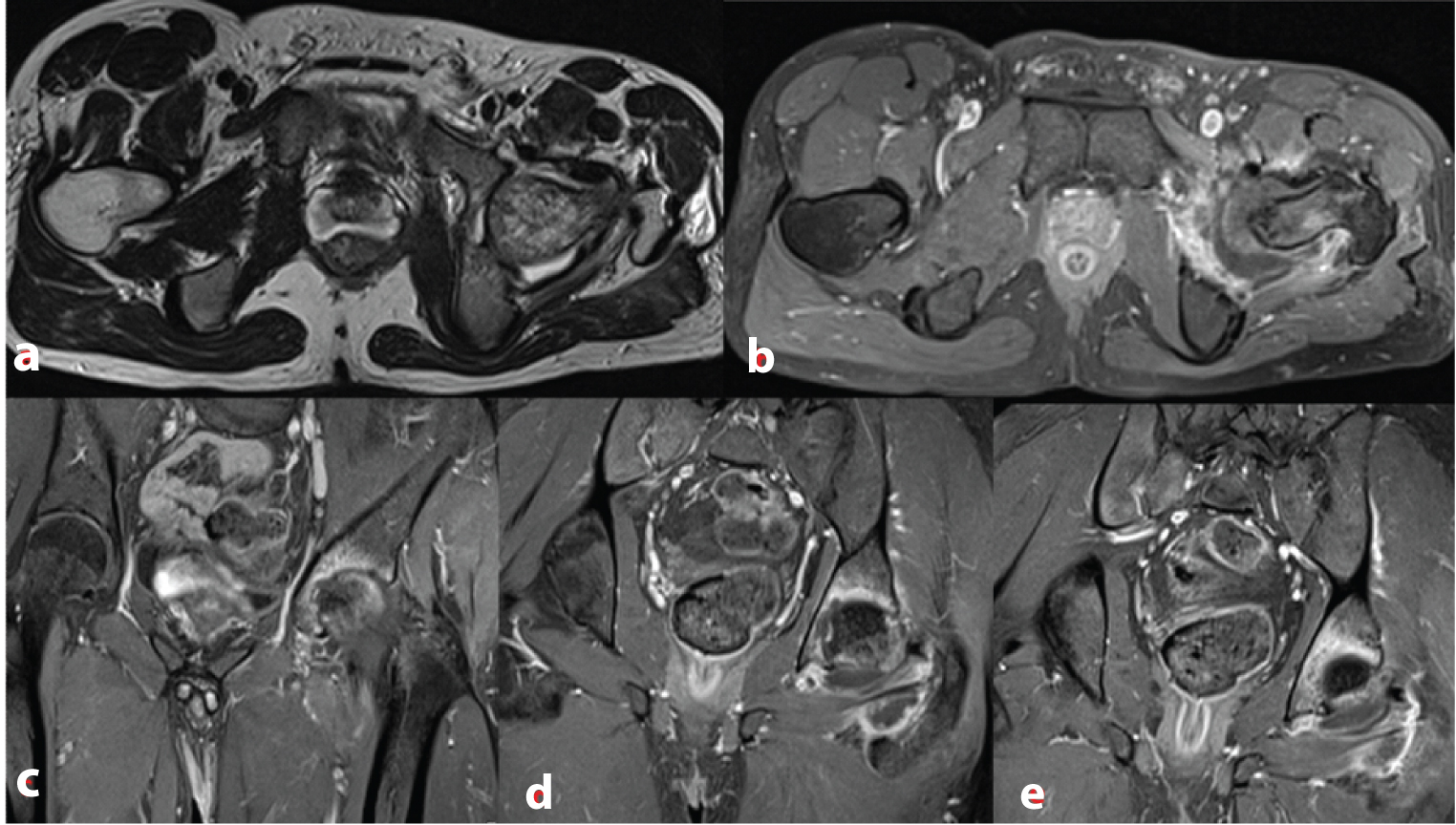
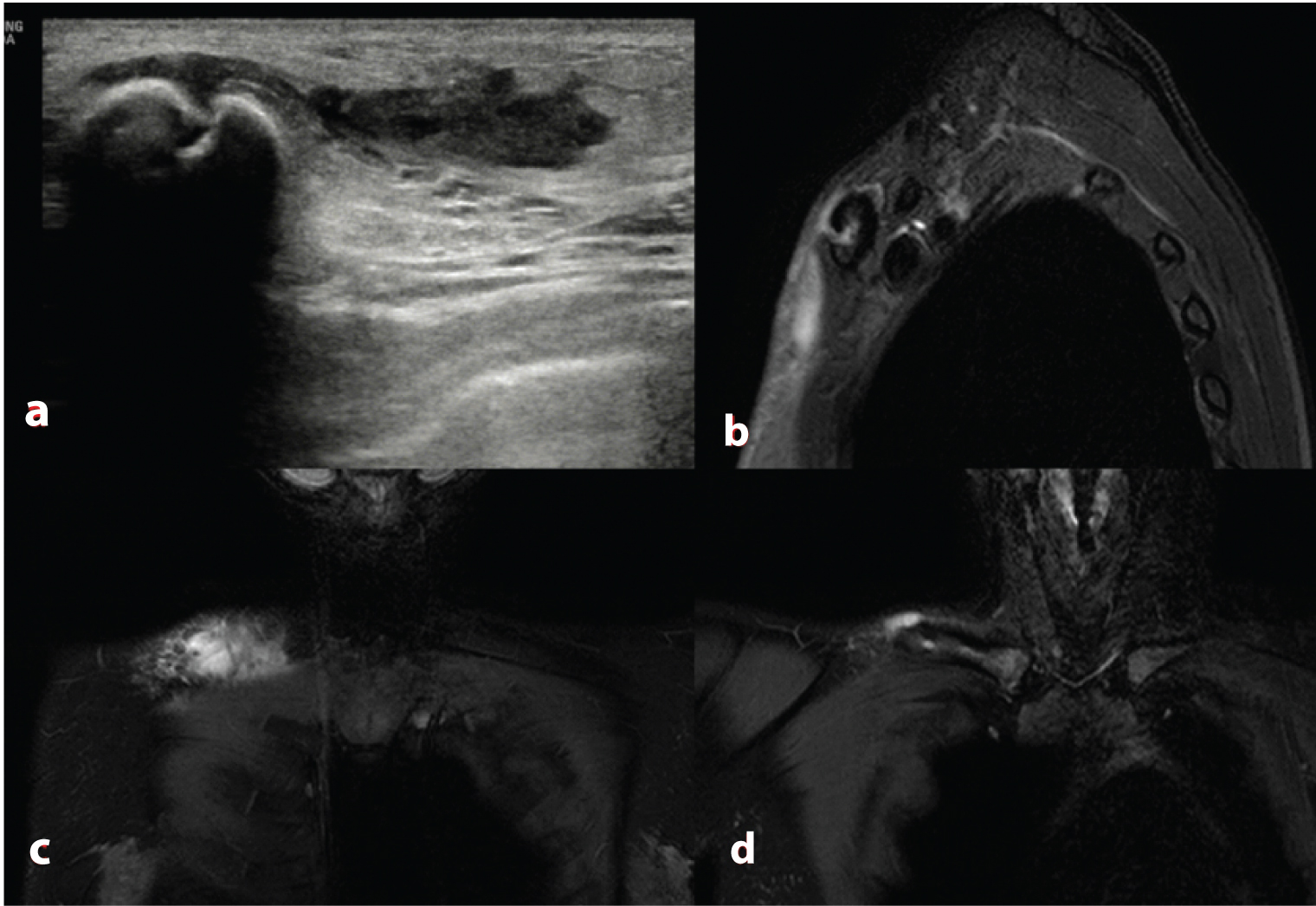
Computed tomography parallels the findings depicted by conventional radiography, albeit with a widened range. It gives a better picture of extent of bone destruction. MRI is the modality of choice in detecting surrounding soft tissue extension and sinus tract formation. CT is of less use in detecting surrounding soft tissue findings, although, contrast enhanced CT may be of some utility. MRI remains the modality of choice in the early detection of joint TB. Joint effusion with thickening and enhancement of synovium is noted in the initial stage of synovitis [Table/Fig-2a-d] [13-15]. Tubercular arthritis is characterised by synovial proliferation which is typically hypointense on T2-weighted images. According to Suh JS et al., hypointensity is due to presence of haemorrhage, fibrosis and inflammatory debris [15]. Articular cartilage defects, subchondral bone erosions, bone marrow oedema are depicted in the early stages before joint space loss occurs [Table/Fig-3a-e]. Soft tissue abnormalities like inflammation of surrounding muscles, subcutaneous tissues may also be seen. Sinus tracts are seen well in T2-weighted images as linear high signal intensity areas. These show tram track appearance on post gadolinium images. Typically, periarticular and para articular abscesses show thin and uniform peripheral enhancement [7,13-15].
A 33-year-old man with tuberculous arthritis of right knee joint. There is gross joint effusion with thickening and enhancement of the synovium. Axial T2 weighted image (A) shows gross joint effusion with thickening of the synovium. Coronal STIR image (B) shows extensive periarticular oedema. Postcontrast fat-saturated T1 weighted images, C and D (axial and sagittal) show thin uniform enhancement of the inflamed synovium.
A 20-year-old man with tubercular arthritis of left hip joint: Axial T2 weighted image (a) shows left hip joint effusion, and altered marrow signal intensity involving the head of left femur. Axial (b), coronal (c, d and e) post contrast fat-saturated T1-weighted images show left hip joint space reduction, mild joint effusion, thin enhancement of the inflamed synovium, enhancement of left acetabulum which may represent reactive hyperemia and well defined periarticular enhancement representing inflammation.
Features of Tubercular Osteomyelitis
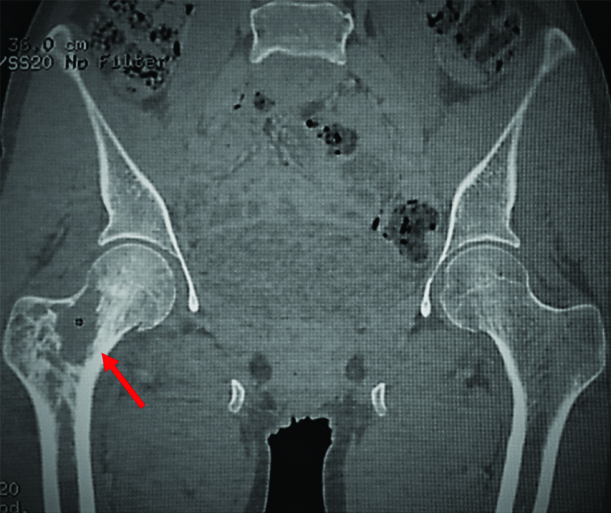
Clinical features and plain radiographic findings: Virtually any bone in the body can be affected by TB. Solitary as well as multiple bones can be affected. Most commonly spreads by haematogenous route from a primary focus. As with other infections, metaphysis is the most common site, though diaphysis can also be affected. Transphyseal spread is considered to occur more commonly in TB than in pyogenic cases. Patient has an insidious onset with gradual onset of pain and swelling. Granulomatous lesion develops at the site of deposition of mycobacteria, which appears as an eccentric osteolytic lesion in the metaphyseal region. Pathologically, two types of lesions are found. In caseous exudative type, there is destruction of bony trabeculae with softening and caseation necrosis of the bone followed by formation of abscess [Table/Fig-4]. In caries sicca type, granulation tissue is formed with minimal caseation [7,14]. Multifocal tuberculous osteomyelitis is also known as osteitiscystica tuberculosa multiplex. Multiple sites of involvement are usually seen in children [16].
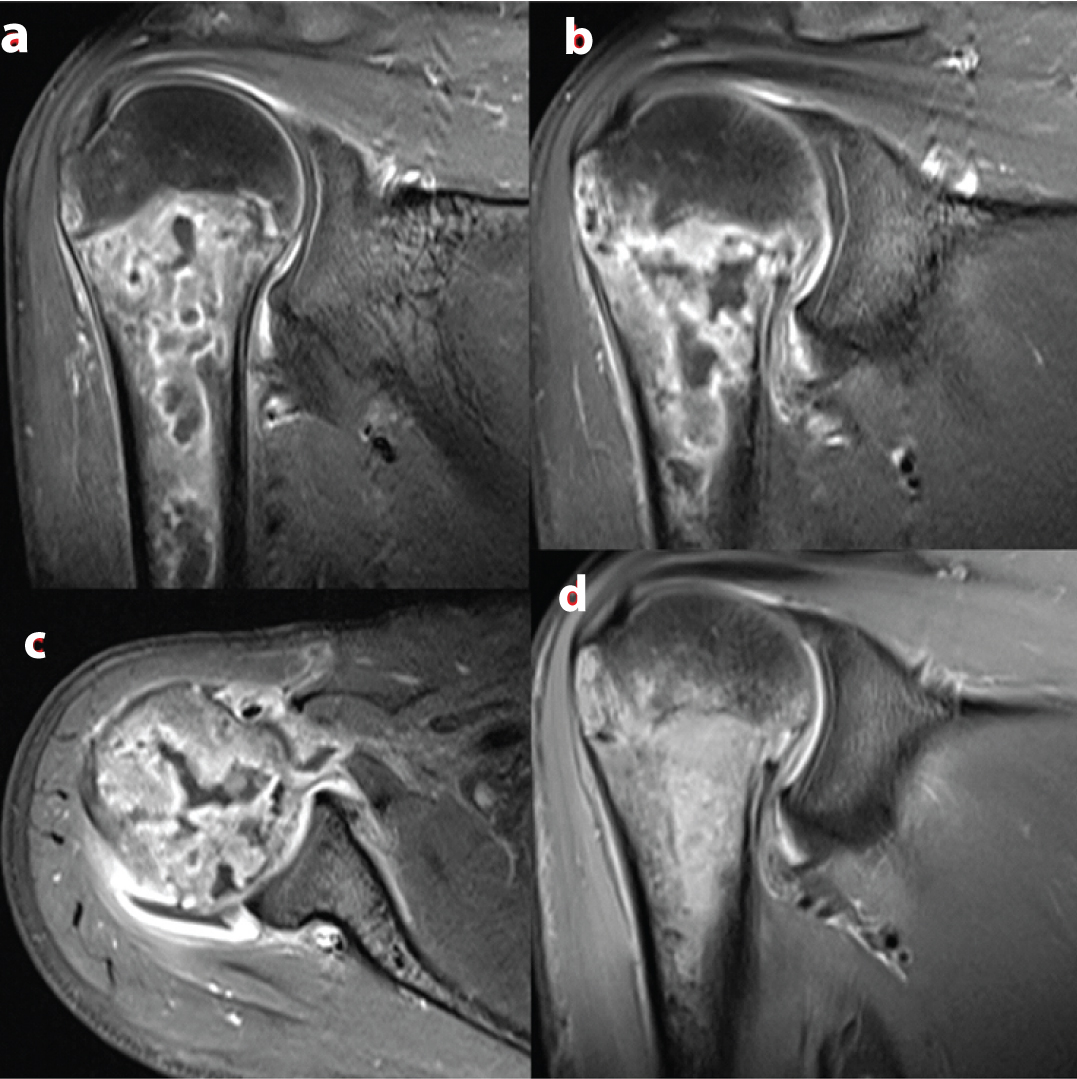
MRI demonstrates involvement of the bone much earlier than other modalities. Early focus of altered marrow signal is noted with irregular margins and cortical erosion is seen at the site of infection. The granulomatous response typically shows intermediate to low signal intensity on T2-weighted images and low signal intensity on T1-weighted images [Table/Fig-5a-d]. This appearance with associated soft tissue abscesses is considered typical of tuberculous infection. Lesions with peripheral rim of high signal intensity on T1-weighted images with surrounding bone marrow oedema is considered non-specific and is seen in infectious cases. Enhancement is noted in post Gadolinium sequences. Caseous necrosis is seen as high signal intensity on T2-weighted images [17-19].
A 35-year-old man with tubercular osteomyelitis of right femur. Coronal Multi-Planar Reformatted CT image shows irregular destruction of bony trabeculae of neck of right femur with small lytic areas in the adjoining bone. No periosteal reaction noted.
A 16-year-old girl with tubercular osteomyelitis of right clavicle. Ultrasound image (a) shows a small subcutaneous collection in the infraclavicular region. It can be traced to the anterior cortex of right clavicle. Cortical discontinuity noted. STIR MR images, sagittal (b) coronal (c and d) show erosion of anterior cortex of mid shaft of clavicle with surrounding mild bone marrow oedema. Soft tissue oedema noted in the surrounding region with small collection in the infraclavicular region
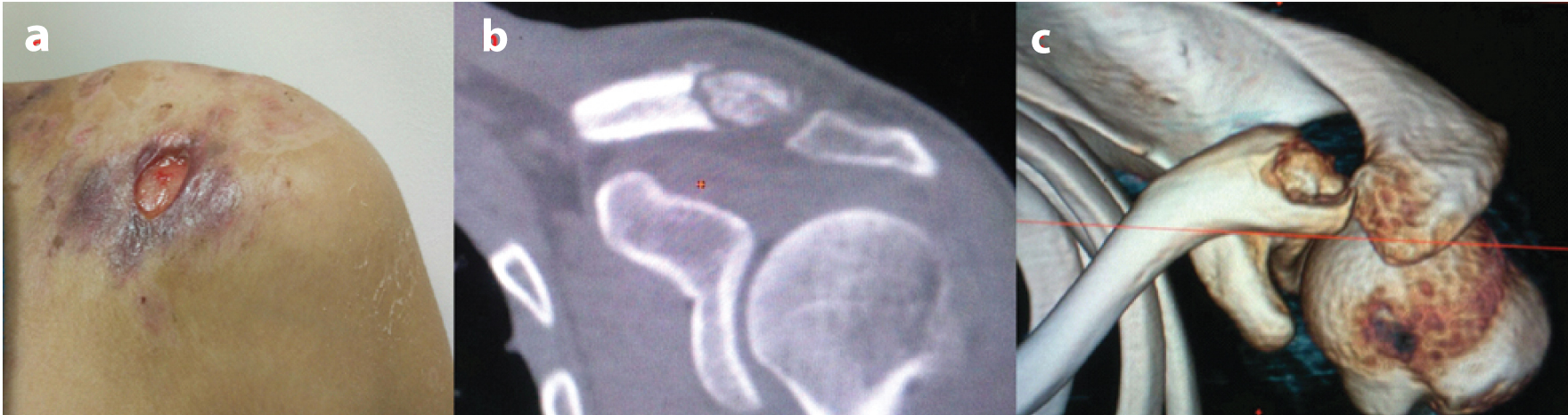
Plain radiographic appearance varies in children and adults. The lesions are typically well-defined lytic bone destruction with minimal sclerosis and bone expansion. In adults, the lesions tend to be along the long axis with of the bone with sclerotic margins. Minimal periosteal reaction is noted [17,20]. CT, as mentioned previously, will add to the information provided by the plain radiographs. While CT is better in demonstrating the extent of bone destruction and sequestrum formation [Table/Fig-6a-c], soft tissue abscesses, fistulae and sinuses are better delineated by MRI.
A 48-year-old gentleman with tubercular osteomyelitis of left clavicle. Photograph (a) of the patient shows a discharging ulcer in the anterior aspect of left shoulder with surrounding indurated margins; b) Coronal reformatted CT image shows a devitalised piece of bone (sequestrum) involving the acromial end of left clavicle. Volume rendered image; c) clearly illustrates the sequestrum from the surrounding normal appearing bone.
Tubercular dactylitis is a form of osteomyelitis involving the small bones of hands and feet. It is described in the subsequent section.
Mimickers of Bone and Joint TB
Pyogenic arthritis: Both tubercular and pyogenic arthritis tend to be monoarticular; though, polyarticular cases may occur in tuberculosis. The presentation is usually insidious in TB with non specific vague pain with minimal systemic signs of inflammation. On the other hand, presentation in septic cases is usually dramatic with florid signs of inflammation such as fever and generalised malaise [11].
Difference in radiologic manifestations of pyogenic and tubercular infection of bones and joints stems from the fact that proteolytic enzymes are not involved in tubercular infection. It is the granulation tissue that erodes and destroys the articular cartilage [21-23].
Conventional radiographic features of pyogenic arthritis include features of joint effusion, juxta-articular osteopenia due to hyperemia, joint space narrowing due to destruction of articular cartilage, subchondral bony erosions and eventually juxta-articular sclerosis and bony ankylosis. It is difficult to differentiate pyogenic arthritis from tubercular arthritis by conventional radiography alone. Gradual reduction in joint space is noted in TB. Destruction of articular cartilage is not evenly distributed in TB. Alternate areas of normal cartilage and eroded cartilage may co-exist. Fibrous ankylosis develops in untreated cases of TB as opposed to bony ankylosis in pyogenic arthritis [7,21-24].
MRI is used extensively due to better sensitivity and helps to differentiate to a greater extent between these two conditions [Table/Fig-7a-d]. An important point to remember is that tubercular arthritis at any stage can be superimposed by pyogenic infection and in that case it can be diagnosed only by microbiological or pathological means.
A 25-year-old man with pyogenic osteomyelitis with reactive joint effusion/arthritis of right shoulder joint. Post contrast fat saturated T1-weighted images (a-c) show multiple intraosseous abscesses involving proximal metaphysis and adjoining diaphysis of humerus. These abscesses show irregular shaggy walls. Coronal fat saturated T2-weighted image; d) shows extensive bone marrow oedema. Mild shoulder joint effusion noted
Joint effusion is noted in both conditions. Subsequent reduction in joint space is severe and progressive in pyogenic arthritis than in TB due to greater destruction of articular cartilage by proteolytic enzymes in septic cases. Abnormalities of the adjoining bone marrow signal intensities noted in both conditions. It is hypothesized as either reactive or due to osteomyelitis. This finding is commonly seen in pyogenic cases than in TB [25,26].
Signal intensity of the affected synovium is due to combined features of hypertrophied and inflamed synovium and joint effusion. Intermediate signal intensity is noted in cases of TB due to presence of admixture of haemorrhage, debris, fibrosis and caseous necrosis. But, not much difference in signal intensity is noted between pyogenic and TB cases [15].
Extra-articular lesions like myositis, abscess are seen in infective arthritis. It depends not only on the type and virulence of organism causing the infection, but also the immunity of the host and duration of infection. Contrast enhanced MR imaging is used for better delineation. Extra-articular lesions in tubercular arthritis consist of abscess with thin and smooth walls and tend to be well marginated. While, in pyogenic arthritis, extra-articular lesions tend to show irregular ill-defined boundaries and abscesses with thick irregular margins. This is due to comparatively minimal inflammation in TB together with chronic insidious course of the disease [21,24,27].
In summary, it is not possible to categorically differentiate between the two conditions. But few features may help the radiologists to discriminate between the two. Arthritis with greater joint space loss, extensive bone marrow oedema with irregular ill-defined extra-articular inflammation with thick and shaggy abscess walls tends to be pyogenic while slower and progressive joint space loss, minimal bone marrow oedema with well-defined extra-articular inflammation with thin and smooth abscess wall is seen in TB. The points of difference between these two conditions have been summarized in the [Table/Fig-8].
Points of difference between tubercular and pyogenic arthritis.
| S.No | Salient features | Tubercular arthritis | Pyogenic arthritis |
|---|
| 1 | Pathophysiology | Absence of proteolytic enzymes and presence of granulation tissue | Presence of proteolytic enzymes |
| 2 | Clinical course | Chronic and insidious | Acute |
| 3 | Joint effusion | Present | Present |
| 4 | Juxta-articular osteopenia | Present | Present |
| 5 | Prominent signal intensity of synovial abnormalities | Predominantly tends to be intermediate | No specific predominance. Can be high or intermediate |
| 6 | Joint space reduction | Gradual joint space loss with uneven distribution of destruction of articular cartilage | Greater degree of joint space loss with extensive destruction of articular cartilage. |
| 7 | Extra-articular lesions | Thin smooth walls of abscesses. Lesions tend to be well marginated | Thick irregular walls of abscesses.Lesions tend to be ill-defined. |
| 8 | Long term sequalae | Fibrous ankylosis | Bony ankylosis |
Rheumatoid Arthritis
Rheumatoid arthritis is a chronic systemic disease with predominant musculoskeletal manifestations. It affects approximately 1% of the population with a female preponderance. Synovitis is the major characteristic of chronic inflammatory disease of autoimmune origins. Synovial hyperemia, hyperplasia and finally pannus formation are the hallmarks of disease pathogenesis. Frequently, joint effusion along with the synovial swelling results in joint space widening. The most vulnerable site in the joint is the ‘bare area’ where the bone is devoid of the articular cartilage and is lined only by the synovium. This results in synovitis induced marginal bone erosions [28,29].
Rheumatoid arthritis is often confused with tubercular arthritis due to overlapping clinical presentation and imaging features. Both the diseases have similar chronically inflamed hypertrophied synovium. While it is the plasma cells and lymphocytes with activation of various cytokines does the damage in rheumatoid arthritis, it is the granulation tissue formed from caseous necrotic areas with leukocytes, mononuclear phagocytes and multinucleated giant cells does it in tuberculosis [29-31].
Radiological findings such as periarticular osteopenia, joint effusion and bony erosions are common in both conditions. As far as distribution and involvement of joints are concerned, oligoarticular rheumatoid arthritis and polyarticular tuberculosis do occur and add to the clinical and radiological dilemma.
Certain features are relatively more common in rheumatoid arthritis than in tubercular arthritis. As shown in the study conducted by Choi JA et al., synovial thickening tends to be uneven and non-uniform in RA. Greater the thickness of inflamed synovium (>1cm), greater the possibility of RA ([Table/Fig-9a-f] compare the severity of thickened synovium in [Table/Fig-2] [29].
A 46-year-old man with rheumatoid arthritis of knee joint. Proton density (PD) fat-saturated multiplanar images (a-Coronal, b and d-Sagittal, c and f-axial) and sagittal PD image (e) show marked synovial thickening which is of intermediate signal intensity. Popliteal bursal cyst noted in (c) with synovial thickening. Marginal erosions noted in the femoral and tibial condyles and head of fibula (d,e). Moderate joint effusion noted.
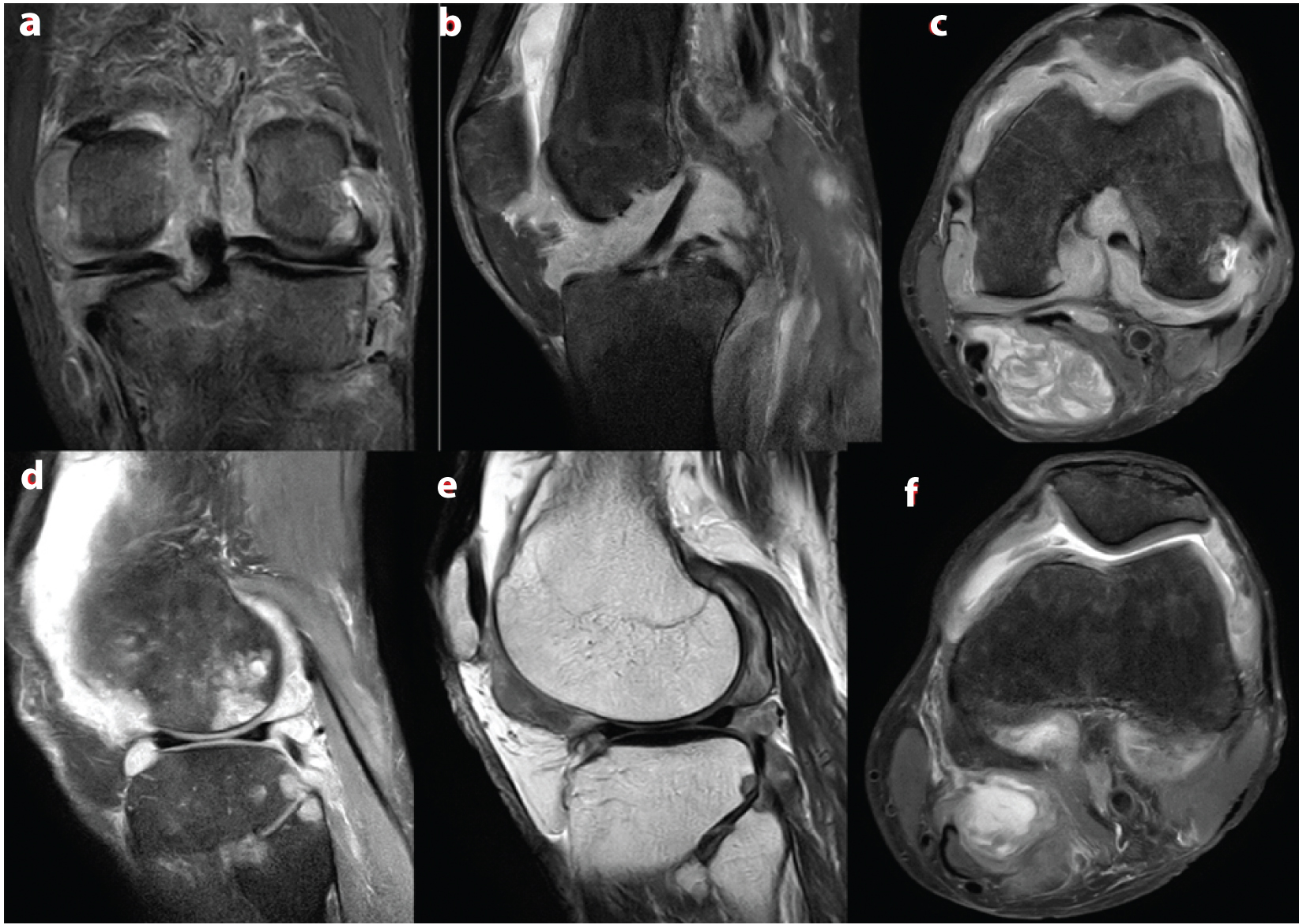
Size of the bony erosions tends to be smaller in RA than TB. Erosions are due to destruction of the articular cartilage by the proteolytic enzymes followed by destruction of the subchondral bone in RA. Hence, subchondral bony erosions occur after cartilaginous erosions in RA except at the bare area as described above. However, in TB, bone erosion can happen even without cartilage erosion due to insinuation of the granulation tissue between the cartilage and subchondral bone. Non-peripheral bony erosions are common in TB and they tend to be larger [29].
Bone marrow oedema is found in both conditions due to hyperemia and increased vascular permeability of bone marrow. Extra-articular cold abscesses are more common in TB. However, periarticular fluid collections in the bursae and other fluid collections like Baker’s cyst can occur in both conditions, albeit commoner in RA. Hence, extra-articular cystic masses should be viewed with caution while making a diagnosis [29-32].
Pigmented Villonodular Synovitis
Pigmented Villonodular Synovitis (PVNS) is a benign synovial proliferative condition characterised by villous, villonodular and nodular proliferation of synovium. Deposition and pigmentation by haemosiderin is a characteristic feature. It affects any part of the musculoskeletal system with synovium-namely the joints, bursa, tendon sheaths etc. It has variable presentations-diffuse and localised intraarticular and localised extra-articular forms. It is a relatively rare disease with localised disease either intra-articular or extra-articular constitutes the majority of the cases. It is most commonly seen in the third to fifth decades of life. Intra-articular forms occur with equal frequency in both sexes, while extra-articular shows a female predilection [33].
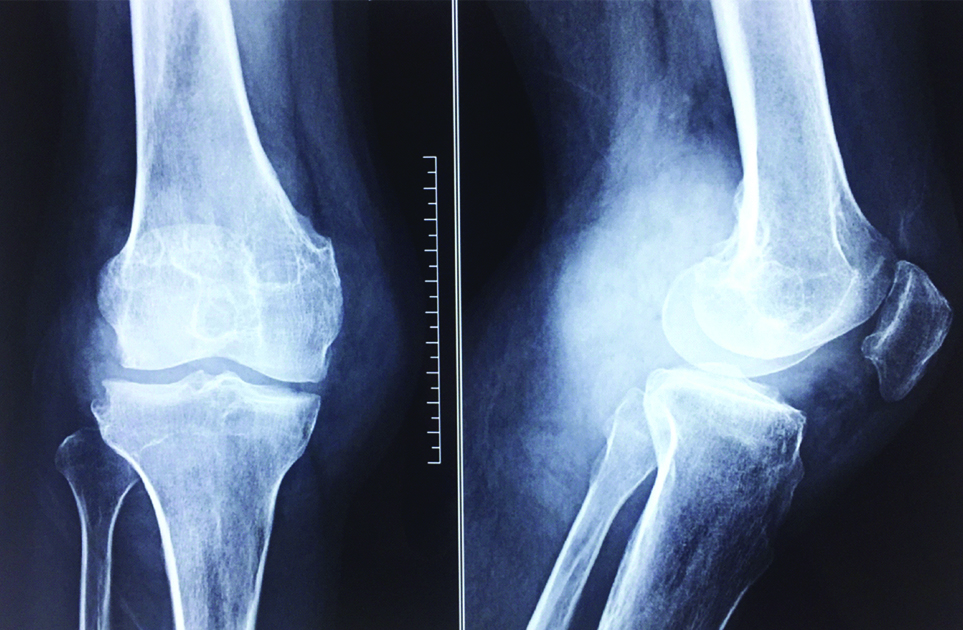
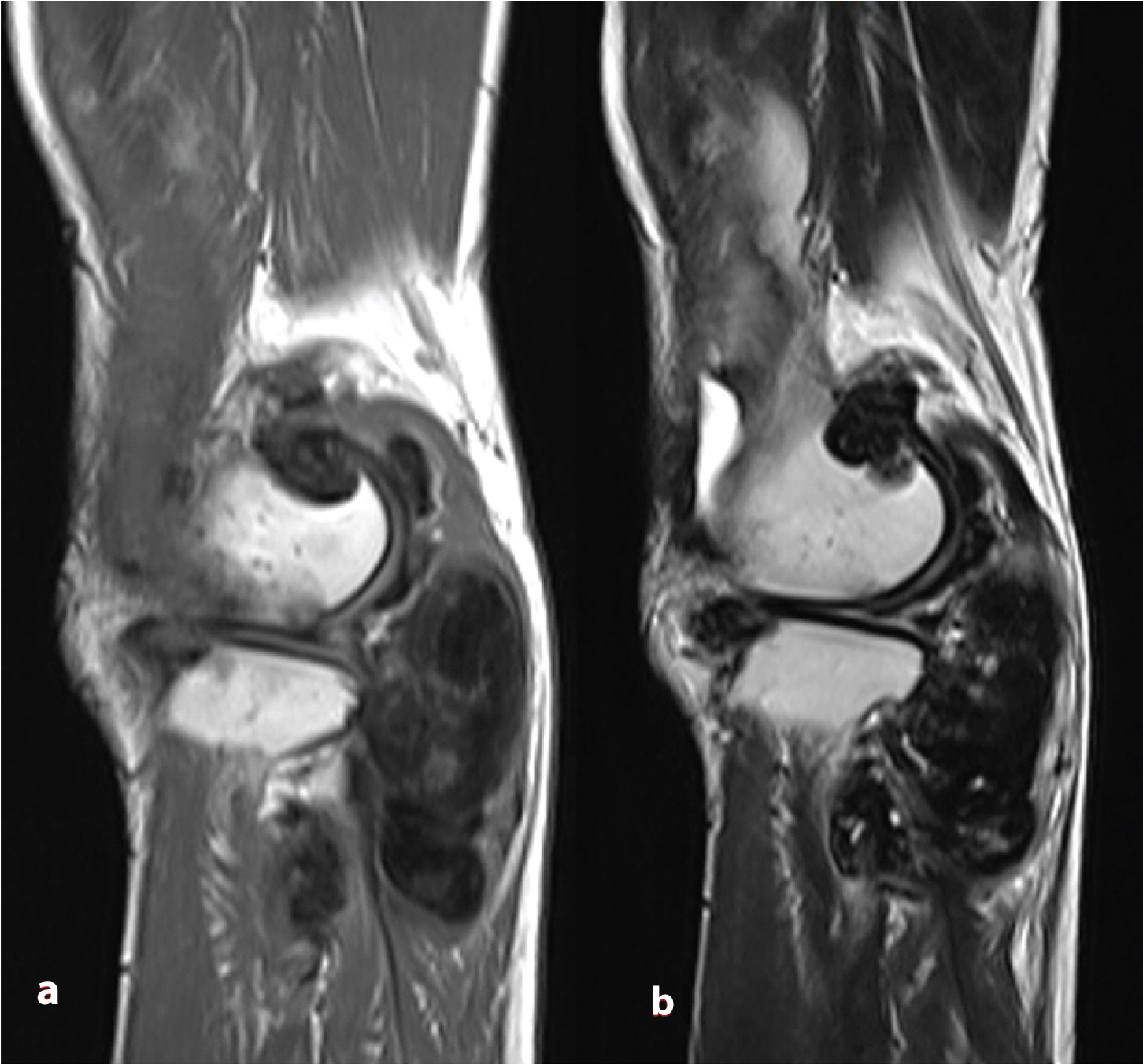
Radiographic features vary according to the subtype: Localised and diffuse intraarticular forms of PVNS mimic the radiographic features of tubercular arthritis. Diffuse intraarticular forms most commonly affect the knee joint. Most common presentation is a soft tissue swelling around the involved joint. Radiographs demonstrate features of soft tissue swelling and joint effusion in the initial phases. Joint space is preserved. Extrinsic erosions of the bone in the form of subchondral lucent areas with thin rim of sclerosis may be noted [Table/Fig-10]. The presence of this finding greatly depends on the capacity of the joint. Large joints like the knee have relatively lesser erosions than the joints with smaller and tighter compartments like the ankle and hip. Bony changes are more clearly depicted in CT. MRI shows heterogeneous localized or diffuse synovial plaque like or nodular thickening. It shows intermediate signal intensity on T1- weighted images. Low signal intensity on T2-weighted images is the characteristic feature due to haemosiderin deposition [Table/Fig-11a,b]. This effect is also demonstrated as blooming on gradient echo images caused by magnetic susceptibility artifact which is considered to be pathognomonic of PVNS on MRI. Treatment depends on the extent and location of the disease. Diffuse intraarticular forms are difficult to treat with high recurrences. Treatment options include surgery, radiation and disease modifying agents or a combination of all.
A 30-year-old man with diffuse intraarticular form of pigmented villonodular synovitis. Radiograph of knee joint AP and lateral views (left to right) show soft tissue swelling with relative preservation of joint space. Erosions noted in the lateral tibial condyle with thin sclerotic margins.
Same patient as in figure 10; Diffuse nodular synovial thickening noted involving the knee joint. They are typically hypointense on T1-weighted (a) and T2-weighted (b) MR images due to haemosiderin deposition.
Features of PVNS often overlap with tubercular arthritis, particularly the monoarticular type. Features of soft tissue swelling, joint effusion, bony erosions are noted in both conditions. Both conditions have an insidious onset with nonspecific symptoms like pain and joint swelling. Incorrectly treating a case of tubercular arthritis as PVNS could delay the diagnosis with ultimate loss of the joint mobility. Haemosiderin deposition and the resultant blooming on GRE are seen only in 82% of the cases and absence of haemosiderin deposition does not rule out PVNS. Also, haemosiderin deposition in intra-articular tissues like menisci is also found in other disorders like rheumatoid arthritis, haemophiliac arthropathy, haemochromatosis and tubercular arthritis [34]. Although, exact incidence of haemosiderin deposition in tubercular arthritis is not known, tuberculosis should be ruled out in an otherwise healthy appearing young individual with monoarticular involvement and joint swelling of long duration. While extraarticular cystic masses are common in tubercular arthritis, extraarticular spread of nodular masses into the popliteus tendon sheath and posterior aspect of posterior cruciate tendon are seen in PVNS. High index of suspicion is needed to make a correct diagnosis [33-36].
Tubercular Dactylitis (Spinaventosa) and its Mimickers
Tubercular dactylitis varies slightly from the usual radiographic manifestation. It appears as a fusiform expansile cyst-like or bubbly lesion due to trabecular destruction with radiolucent medulla and ballooning of the remaining thinned out cortex giving the appearance of spinaventosa (meaning wind-filled sail) [37]. Associated spindle shaped soft tissue swelling is noted. Minimal periosteal reaction and absence of sequestrum formation differentiates it from pyogenic infections [Table/Fig-12]. Healing usually results in the shortening of the involved bone and deformity of the adjoining joint. Following treatment, these lesions show sclerosis with coarse trabeculations with near normal restoration of bone density [38].
A nine-year-old boy with tubercular dactylitis of right foot. Radiograph of foot shows fusiform mildly expansile lesion involving diaphysis of 4th metatarsal bone. Irregular lucent areas noted within the medullary cavity with trabecular destruction and thinning of the cortex.

Fungal infection of small bones may occur and resemble tubercular forms. Absent or very minimal periosteal reaction is seen in fungal infections also. The affected extremity is swollen and oedematous with multiple granule draining sinuses. Definitive diagnosis is by microscopic examination of the draining granules and culture. Imaging helps to delineate the extent of the infection [39].
A variety of tumours like giant cell tumour, enchondroma, chondroblastoma, periosteal chondroma, fibroxanthoma and osteochondroma can affect the small bones and mimic spinaventosa radiologically. Of these, giant cell tumour and enchondroma frequently affect the small bones and mimic tubercular dactylitis.
Giant Cell Tumour (GCT) of the small bones is relatively rare. It has a reported incidence of 1.2 to 4% in hands and 0.9 to 1.8% in feet. Tumours of the hand tend to have a more aggressive biological behavior. Main symptom is pain. Characteristic radiographic appearance is marked cortical ballooning due to multidirectional expansion of the cortex [Table/Fig-13]. Presence of pseudo-trabeculations giving honeycomb appearance, absence or minimal periosteal reaction, absence of sclerosis, absence of matrix mineralization and involvement of the subchondral bone differentiates it from infections and other benign tumours. MRI also aids in diagnosing GCT. The tumour has low signal intensity in all sequences due to deposition of haemosiderin or collagen [40,41].
A 32-year-old man with giant cell tumour of hand. Radiograph of hand-AP view shows marked cortical ballooning with multidirectional expansion of cortex involving proximal phalanx of middle finger. Pseudo-trabeculations giving honey comb appearance is noted with involvement of subchondral bone.

Enchondroma, a common benign tumour of hands and feet, also presents as a geographic lytic lesion mimicking spinaventosa. It is usually detected incidentally. In the presence of pain, always look for pathological fracture. In the absence of fracture, a painful lesion is unlikely to be enchondroma and requires further evaluation. It appears as a well marginated lytic lesion arising from the medullary cavity closer to the epiphysis. There is cortical expansion with thinning, although to a lesser extent than GCT [Table/Fig-14]. Being a cartilaginous lesion, characteristic appearance is the presence of chondroid matrix with popcorn-like, rings, arcs or whorls of calcification and endosteal scalloping. Pathological fractures can be obvious with displacement or very subtle in the form of cortical discontinuity [41].
An eight-year-old boy with multiple enchondromatosis. Mulitple expansile lytic lesions noted involving metacarpal, proximal and middle phalanges. Endosteal scalloping noted

Tubercular Sacroilitis and its Mimickers
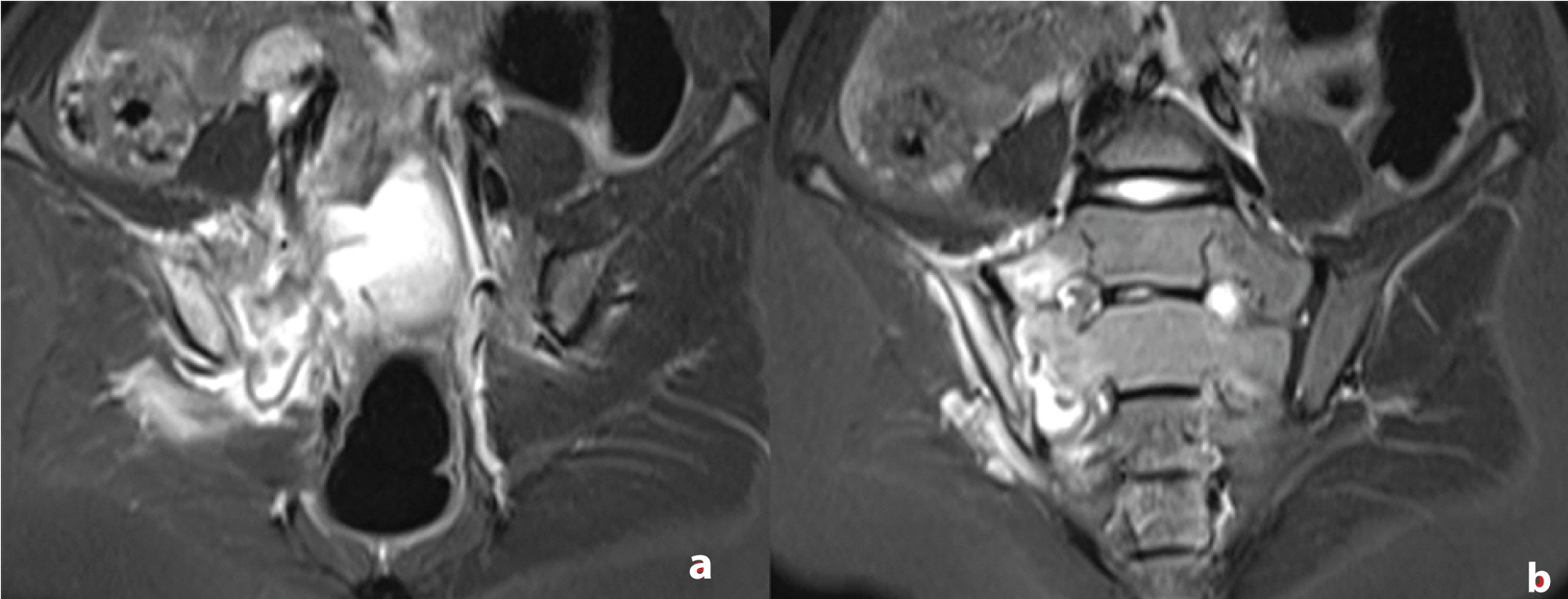
Sacroiliac joint has two distinct parts. Lower anterior part is cartilaginous while upper posterior part is fibrous. Joint margins are smooth and regular in the cartilaginous part and irregular in the fibrous part. Also, the hyaline cartilage is thinner on the iliac side than the sacral side. Sacroiliac joint is affected by tuberculosis in 3-9.7% of cases [42,43]. The diagnosis is usually delayed due to non-specific symptoms. Buttock pain is the most common presenting symptom. Pain may be referred to groin, thigh and rarely knee. Irritation of lumbosacral plexus may cause signs of femoral or sciatic nerve irritation. Infection tends to be usually unilateral. Bilateral involvement is noted in cases of secondary spread from psoas abscess in caries of the lower lumbar spine. Plain radiographs may be negative in the early stages. Subtle haziness or loss of joint line and periarticular osteopenia may be seen. CT scan shows clearly the extent of the joint destruction while MRI shows the soft tissue extent of the infection. MRI shows capsular distension and bone marrow oedema [Table/Fig-15a,b]. Later stages show joint space widening due to articular cartilage destruction, sclerosis of the margins and sequestrum formation. These findings are better delineated in CT scan [42,43].
A 22-year-old girl with tubercular sacroilitis right side. Fat saturated T2-weighted images show right sacroiliac joint distension, bone marrow oedema involving both iliac and sacral articular surfaces and periarticular soft tissue oedema. Left sacroiliac joint appears normal.
Pyogenic sacroilitis occurs by haematogeneous spread from cutaneous sources. Pregnancy, immunocompromised states, trauma are few of the predisposing factors. Infection usually begins in the ilium due to sluggish blood flow as osteomyelitis which subsequently spread to the joint.
Seronegative spondyloarthropathy associated sacroilitis is the important differential diagnosis and includes a number of diseases. CT features include subchondral osteopenia, erosions and subchondral sclerosis. Erosions tend to occur early on the iliac side due to thinner cartilage. MRI features include joint effusion, subchondral bone marrow oedema, erosions, capsulitis and enthesitis in the early stages and subchondral sclerosis, subchondral fatty deposition in the late stages. Bony ankylosis occurs in terminal stages [44].
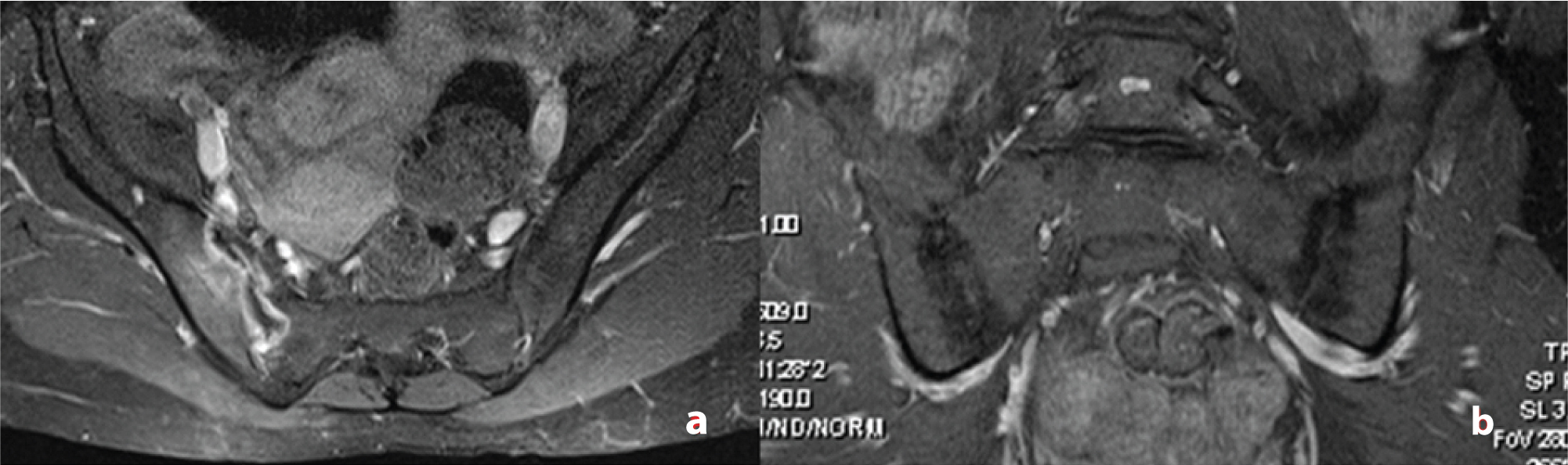
Though most of the features show considerable overlap between infective and inflammatory sacroilitis, few points’ aid in distinguishing between these two conditions. Infective sacroilitis tend to be unilateral with disproportionate bone marrow oedema and soft tissue collection or abscess formation. Inflammatory sacroilitis tend to be bilateral with asymmetric involvement and associated changes in the vertebrae may be seen in most cases. Intraosseous and periarticular soft tissue collection or abscess formation favours the diagnosis of infective sacroilitis [Table/Fig-16a,b] [42-44].
Comparison of infective and inflammatory sacroilitis. a) shows a 24-year-old lady with tubercular sacroilitis. Post contrast image demonstrates the acute phase of sacroilitis with enhancement of the articular and periarticular tissues. Left sacroiliac joint appears normal; b) shows a 33-year-old man with seronegative spondyloarthropathy. STIR MR image shows symmetrical involvement of bilateral sacroiliac joints with joint space narrowing and subchondral sclerosis.
Conclusion
Extraspinal osteoarticular TB poses a significant clinical challenge. Strong suspicion with methodical analysis of the clinical features and radiological findings are mandatory for making a correct diagnosis. With atypical radiological findings, absence of pathognomonic signs and variety of other disease processes mimicking TB, only a comprehensive clinical, imaging and pathological scrutiny can help the clinicians to make an accurate diagnosis. Given the situation, the need for histo-pathological evidence of tuberculosis from the affected bones and joints before initiation of therapy cannot be undermined.
[1]. Malaviya AN, Kotwal PP, Arthritis associated with tuberculosisBest Pract Res Clin Rheumatol 2007 17:319-343.10.1016/S1521-6942(02)00126-2 [Google Scholar] [CrossRef]
[2]. Tseng C, Huang RM, Chen KT, Tuberculosis arthritis: epidemiology, diagnosis, treatmentClin Res Foot Ankle 2014 2:131-38. [Google Scholar]
[3]. Iademarco MF, Castro KG, Epidemiology of tuberculosisSemin Respir Infect 2003 18:225-40.10.1053/S0882-0546(03)00074-4 [Google Scholar] [CrossRef]
[4]. Sequeira W, Co H, Block JA, Osteoarticular tuberculosis: Current diagnosis and treatmentAm J Ther 2000 7:393-98.10.1097/00045391-200007060-0000911304648 [Google Scholar] [CrossRef] [PubMed]
[5]. Abdelwahab IF, Bianchi S, Martinoli C, Klein M, Hermann G, Atypical extraspinal musculoskeletal tuberculosis in immunocompetent patients: part II, tuberculous myositis, tuberculous bursitis, and tuberculoustenosynovitesCan Assoc Radiol J 2006 57(5):278-86. [Google Scholar]
[6]. Tuli SM, General principles of osteoarticular tuberculosisClin Orthop Relat Res 2002 398:11-19.10.1097/00003086-200205000-0000311964626 [Google Scholar] [CrossRef] [PubMed]
[7]. Vanhoenacker FM, Sanghvi DA, De Backer AI, Imaging features of extraaxial musculoskeletal tuberculosisIndian J Radiol Imaging 2009 19(3):176-86.10.4103/0971-3026.5487319881081 [Google Scholar] [CrossRef] [PubMed]
[8]. Pigrau-Serrallach C, Rodríguez-Pardo D, Bone and joint tuberculosisEur Spine J 2013 22(4):S556-66.10.1007/s00586-012-2331-y22711012 [Google Scholar] [CrossRef] [PubMed]
[9]. Kroot EJ, Hazes JM, Colin EM, Dolhain RJ, Poncet’s disease: reactive arthritis accompanying tuberculosis. Two case reports and a review of literatureRheumatology (Oxford) 2007 46(3):484-89.10.1093/rheumatology/kel26816935915 [Google Scholar] [CrossRef] [PubMed]
[10]. Resnick D, Diagnosis of Bone and Joint Disorders 1984 42nd EditionPhiladelphia, PAWB Saunders:2661-86. [Google Scholar]
[11]. Shah BH, Mir T, Concomitant tuberculosis and septic arthritis of knee joint in a diabetic patientJK-Practitioner 2003 10(2):127-29. [Google Scholar]
[12]. Marks KE, Mchenry MC, Non-spinal tuberculosis Ini Evarts CM, edSurgery of the Musculo-skeletal system 1990 New YorkChurchill Livingstone:4557-72. [Google Scholar]
[13]. Sawlani V, Chandra T, Mishra RN, Aggarwal A, Jain UK, Gujral RB, MRI features of tuberculosis of peripheral jointsClin Radiol 2003 58(10):755-62.10.1016/S0009-9260(03)00271-X [Google Scholar] [CrossRef]
[14]. Engin G, Acunas B, Acunas G, Tunaci M, Imaging of extrapulmonary tuberculosisRadiographics 2000 20:471-88.10.1148/radiographics.20.2.g00mc0747110715344 [Google Scholar] [CrossRef] [PubMed]
[15]. Suh JS, Lee JD, Cho JH, Kim MJ, Han DY, Cho NH, MR imaging of tuberculous arthritis: clinical and experimental studiesJ Magn Reson Imaging 1996 1:185-89.10.1002/jmri.18800601338851426 [Google Scholar] [CrossRef] [PubMed]
[16]. Kritsaneepaiboon S, Skeletal involvement in pediatric tuberculosis: radiologic imaging manifestationsTB Corner 2016 2(2):01-06. [Google Scholar]
[17]. De Vuyst D, Vanhoenacker F, Gielen J, Bernaerts A, De Schepper AM, Imaging features of musculoskeletal tuberculosisEur Radiol 2003 13:1809-19.10.1007/s00330-002-1609-612942283 [Google Scholar] [CrossRef] [PubMed]
[18]. Sharma P, MR features of tuberculous osteomyelitisSkeletal Radiol 2003 32(5):279-85.10.1007/s00256-003-0621-512679845 [Google Scholar] [CrossRef] [PubMed]
[19]. Atasoy C, Oztekin PS, Ozdemir N, Sak SD, Erden I, Akyar S, CT and MRI in tuberculous sternal osteomyelitisClin Imaging 2002 26(2):112-15.10.1016/S0899-7071(01)00374-6 [Google Scholar] [CrossRef]
[20]. Teo HE, Peh WC, Skeletal tuberculosis in childrenPediatr Radiol 2004 34:853-60.10.1007/s00247-004-1223-715278319 [Google Scholar] [CrossRef] [PubMed]
[21]. Hong SH, Kim SM, Ahn JM, Chung HW, Shin MJ, Kang HS, Tuberculous versus Pyogenic Arthritis: MR Imaging EvaluationRadiology 2001 218:848-53.10.1148/radiology.218.3.r01fe2784811230666 [Google Scholar] [CrossRef] [PubMed]
[22]. Yao DC, Sartoris DJ, Musculoskeletal tuberculosisRadiol Clin North Am 1995 33:679-89. [Google Scholar]
[23]. Akeson WH, Amiel D, Gershuni DH, Articular cartilage physiology and metabolism. In: Resnick D, edDiagnosis of bone and joint disorders 1995 3rd edPhiladelphia, PaSaunders:785-787. [Google Scholar]
[24]. Jon A, Jacobson JA, Girish G, Jiang Y, Resnick D, Radiographic evaluation of arthritis: inflammatory conditionsRadiology 2008 248:378-89.10.1148/radiol.248206211018641245 [Google Scholar] [CrossRef] [PubMed]
[25]. Forrester DM, Feske WI, Imaging of infectious arthritisSemin Roentgenol 1996 31:239-49.10.1016/S0037-198X(96)80032-0 [Google Scholar] [CrossRef]
[26]. Deely DM, Schweitzer ME, MR imaging of bone marrow disordersRadiol Clin North Am 1997 35:193-212. [Google Scholar]
[27]. Hopkins KL, Li KC, Bergman G, Gadolinium-DTPA-enhanced magnetic resonance imaging of musculoskeletal infectious processesSkeletal Radiol 1995 24:325-30.10.1007/BF001970597570151 [Google Scholar] [CrossRef] [PubMed]
[28]. Sommer OJ, Kladosek A, Weiler V, Czembirek H, Boeck M, Stiskal M, Rheumatoid arthritis: a practical guide to state-of-the-art imaging, image interpretation, and clinical implicationsRadiographics 2005 25:381-98.10.1148/rg.25204511115798057 [Google Scholar] [CrossRef] [PubMed]
[29]. Choi JA, Koh SH, Hong SH, Koh YH, Choi JY, Kang HS, Rheumatoid arthritis and tuberculous arthritis: differentiating MRI featuresAJR 2009 193:1347-53.10.2214/AJR.08.216419843752 [Google Scholar] [CrossRef] [PubMed]
[30]. Baeten D, Demetter P, Cuvelier C, Van den Bosch F, Kruithof E, Van Damme N, Comparative study of the synovial histology in rheumatoid arthritis, spondyloarthropathy, and osteoarthritis: influence of disease duration and activityAnn Rheum Dis 2000 59:945-53.10.1136/ard.59.12.94511087697 [Google Scholar] [CrossRef] [PubMed]
[31]. Harris ED Jr, In: Kelly WN, Harris ED Jr, Ruddy S, Sledge CB, edsEtiology and pathogenesis of rheumatoid arthritis 1993 4th edPhiladelphia, PASaunders:855-864. [Google Scholar]
[32]. Winalski CS, Palmer WE, Rosenthal DI, Weissman BN, Magnetic resonance imaging of rheumatoid arthritisRadiol Clin North Am 1996 34:243-58. [Google Scholar]
[33]. Murphy MD, Rhee JH, Lewis RB, Fanberg-Smith JC, Flemming DJ, Walker EA, Pigmented villonodular synovitis: radiologic-pathologic correlationRadiographics 2008 28:1493-518.10.1148/rg.28508513418794322 [Google Scholar] [CrossRef] [PubMed]
[34]. Bennett GL, Leeson MC, Michael A, Extensive hemosiderin deposition in the medial meniscus of a knee. Its possible relationship to degenerative joint diseaseClin Orthop Relat Res 1998 230:182-85.10.1097/00003086-198805000-00020 [Google Scholar] [CrossRef]
[35]. Lee DH, Lee DK, Lee SH, Park JH, Kim CH, Han SB, Tuberculous arthritis of the knee joint mimicking pigmented villonodularsynovitisKnee Surg Sports Traumatol Arthrosc 2012 20(5):937-40.10.1007/s00167-011-1662-221912886 [Google Scholar] [CrossRef] [PubMed]
[36]. Meena S, Gangary SK, Knee tuberculosis masquerading as pigmented villonodularsynovitisJ Res Med Sci 2014 19(12):1193-95. [Google Scholar]
[37]. Clarke JA, Case Report: Tuberculousdactylitis in childhood the need for continued vigilanceClin Radiol 1990 42(4):287-88.10.1016/S0009-9260(05)82122-1 [Google Scholar] [CrossRef]
[38]. Dhillon MS, Sharma S, Gill SS, Nagi ON, Tuberculosis of the bones and joints of the foot: An analysis of 22 casesFoot Ankle 1993 14:505-13.10.1177/1071100793014009048314185 [Google Scholar] [CrossRef] [PubMed]
[39]. Cuellar ML, Silveira LH, Espinoza LR, Fungal arthritisAnn Rheum Dis 1992 51:690-97.10.1136/ard.51.5.6901616344 [Google Scholar] [CrossRef] [PubMed]
[40]. Yanagisawa M, Okada K, Tajino T, Torigoe T, Kawai A, Nishida J, A clinicopathological study of giant cell tumor of small bonesUps J Med Sci 2011 116:265-68.10.3109/03009734.2011.59629021919814 [Google Scholar] [CrossRef] [PubMed]
[41]. Uppin SG, Sundaram C, Umamahesh M, Chandrashekar MS, Rani J, Prasad VBN, Lesions of the bones of the hands and feet. A Study of 50 CasesArch Pathol Lab Med 2008 132:800-12. [Google Scholar]
[42]. Papagelopoulos PJ, Papadopoulos EC, Mavrogenis AF, Themistocleous GS, Korres DS, Soucacos PN, Tuberculoussacroiliitis. A case report and review of the literatureEur Spine J 2005 14:683-88.10.1007/s00586-004-0831-015690213 [Google Scholar] [CrossRef] [PubMed]
[43]. Ramlakan RJS, Govender S, Sacroiliac joint tuberculosisInternational Orthopaedics 2007 31:121-24.10.1007/s00264-006-0132-916673102 [Google Scholar] [CrossRef] [PubMed]
[44]. Prakash D, Prabhu SM, Irodi A, Seronegative spondyloarthropathy-related sacroiliitis: CT, MRI features and differentialsIndian J Radiol Imaging 2014 24(3):271-78.10.4103/0971-3026.13704625114391 [Google Scholar] [CrossRef] [PubMed]