Ectopic Primary Intrathyroidal Thymoma: A Case Report and Review of Literature
Jiby Soosen Ninan1, Sandhya Ilanthodi2, Muktha R Pai3
1 Postgraduate Student, Department of Pathology, A.J. Institute of Medical Sciences and Research Center, Kuntikana, Mangaluru, Karnataka, India.
2 Associate Professor, Department of Pathology, A.J. Institute of Medical Sciences and Research Center, Kuntikana, Mangaluru, Karnataka, India.
3 Professor and Head, Department of Pathology, A.J. Institute of Medical Sciences and Research Center, Kuntikana, Mangaluru, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Jiby Soosen Ninan, JoseVilla, K.Karodu Kozhuvallur P.O. Via Chengannur, Alappuzha District, Kerala-689521, India.
E-mail: jibysoosen@gmail.com
Thymomas are rare neoplasms comprising less than 1% of adult cancers. Ectopic thymomas are thought to arise from aberrant thymic tissue displaced during embryologic development and are extremely rare accounting for only upto 4% of all thymomas. Ectopic intrathyroidal thymoma is a rare entity with only eight previous cases reported to the best of our knowledge. Here we present a rare case of ectopic primary intra thyroidal thymoma with the clinical, morphological and immunohistochemical features.
Ectopic Intrathyroidal Thymoma, Hyperthyroidism, Thymus, Thyroid
Case Report
A 43-year-old woman presented to the Ear Nose and Throat outpatient department of A.J Institute of Medical Sciences and Research Centre, Mangaluru, Karnataka, India, with history of gradually progressive swelling in front of the neck since 15 years and was associated with dysphagia since two months [Table/Fig-1]. Her thyroid function tests were as follows: T3-167 ng/dL, T4-14.9 ng/ dL and serum creatinine and serum electrolytes were normal. The patient had no other comorbidities like diabetes or hypertension and was not taking any medications. Ultrasonography of the neck was suggestive of multinodular goitre. FNAC was done and reported as adenomatoid nodule.
Diffuse swelling in front of the neck associated with dysphagia.

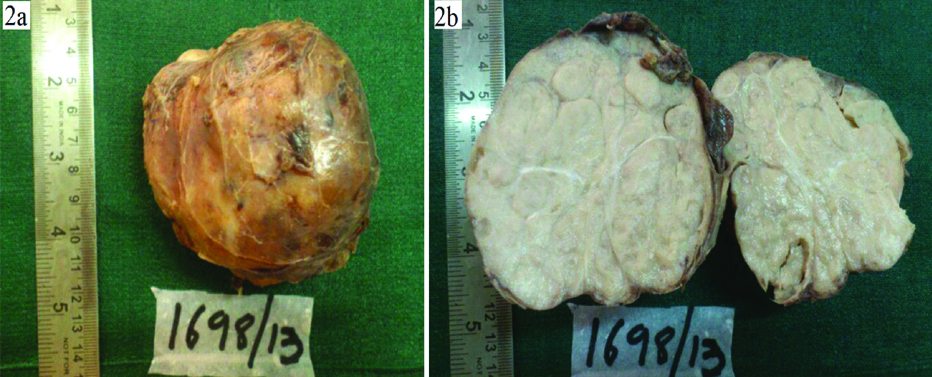
In view of the multinodular goitre with hyperthyroidism, she underwent total thyroidectomy and the specimen was sent for histopathological examination. The thyroid specimen measured 9x7x5 cm. The outer surface of thyroid gland was nodular and congested [Table/Fig-2a]. Cut surface showed firm, encapsulated grey white lobules of tumour tissue with compressed normal colloid filled areas at the periphery [Table/Fig-2b].
a) Thyroid specimen measuring 9x7x5 cm. Outer surface is nodular and congested with enlargement of the thyroid gland, capsule is intact; b) cut surface of the thyroid specimen showing grey-white lobules of tumour tissue, capsulated, firm in consistency with compressed thyroid tissue in the periphery.
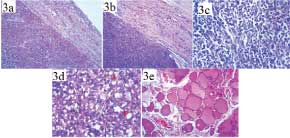
Microscopy showed well encapsulated tumour tissue composed of varying sized lobules delineated by fibrous septa [Table/Fig-3a,b]. Two types of cells were noted, epithelial cells and lymphocytes [Table/Fig-3c]. The epithelial cells were arranged in sheets, clusters and storiform pattern and exhibited ovoid to spindle shape with regular, round to oval vesicular nuclei and small nucleoli. Admixed in between were trapped normal thyroid follicles [Table/Fig-3d]. Numerous vascular spaces of varying sizes were noted focally. The second population of cells were reactive lymphoid cells with small round nuclei having dense chromatin. Lymphocytes were seen focally intermingled with epithelial cells and as separate lobules in other areas along with scattered tingible body macrophages, imparting a starry sky appearance. The fibrous capsule covering the tumour showed colloid free thyroid follicles of varying sizes. Sections from adjacent normal appearing thyroid show colloid filled follicles of varying sizes separated by thin fibrous septa [Table/Fig-3e].
a) Low power view of the tumour with the capsule (H&E 4X); b) Tumour tissue infiltrating into the capsule, composed predominantly of spindle shaped epithelial cells (H&E 4X); c) Section shows spindle shaped epithelial cells and lymphoid cells (H&E 40X); d) Trapped normal thyroid follicles admixed between the epithelial tumour cells (H&E 40X); e) Adjacent normal thyroid follicles at the periphery (H&E 4X).
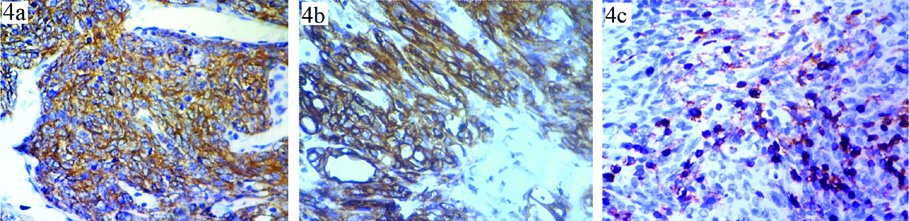
Immunohistochemical studies showed CD45 positivity in the interspersed lymphoid cells. Cytokeratin AE1/AE3 showed cytoplasmic membrane positivity in the spindle shaped epithelial cells [Table/Fig-4a-c].
a) IHC for cytokeratin shows spindle shaped epithelial cells showing membranous positivity for cytokeratin; b) (IHC Pancytokeratin AE1/AE3 40X); c) Section shows CD 45 positivity in lymphoid cells sparing spindle shaped epithelial cells (IHC CD45 40X).
After analysing histomorphological features with immunohistochemical markers, a diagnosis of Ectopic Intrathyroid Thymoma was made. The patient was lost to follow-up.
Discussion
The thymus is formed embryologically from the third and occasionally the fourth pair of pharyngeal pouches along with the inferior pair of parathyroid glands. It descends to its usual location in the anterior superior mediastinum by the end of the second month of gestation [1,2]. Histologically it is composed of the lymphoid cells and the thymic epithelial cells. The thymic epithelium begins as two flask-shaped endodermal diverticula that form from only the third pharyngeal pouch and extend laterally and backward into the surrounding mesoderm and neural crest-derived mesenchyme in front of the ventral aorta [3].
The mature thymus gland is pyramidal in shape and is composed of two incompletely fused lobes within a fibrous capsule extending from the lower poles of the thyroid gland to the pericardium and great vessels. The gland’s capsule has fibrous extensions which divides the thymic lobes into many lobules, each of which has an outer cortical layer and a central medulla [1].
Ectopic thymomas are thought to arise from aberrant thymic tissue displaced during embryologic development and are extremely rare, accounting for only up to 4% of all thymomas [4,5]. Thymic maldescent, sequestration, or persistent thymic rests along the thymopharyngeal tract have been implicated to be the origin of ectopic thymomas [5]. Reported sites of ectopic thymoma include the neck, posterior and middle mediastinum, trachea, pericardium, lung, and pleural cavity [5].
Previously, tumours reported as Primary Intrathyroidal Thymomas (PITs) comprised a heterogeneous group of neoplasms that, in addition to true thymomas, included entities later redefined as “Spindle Epithelial Tumour With Thymus-Like Differentiation” (SETTLE) and “Carcinoma Showing Thymus-Like Differentiation” (CASTLE) [5,6]. PITs also need to be separated from ectopic cervical thymomas that often occur in the general region of the thyroid near the thoracic inlet but are either separate from or only adhere to the inferior poles of the gland [5].
The occurrence of PIT is extremely uncommon with only 8 previously reported cases [1,5-8]. The cases were described in [Table/Fig-5].
PIT in previously reported cases [5-8].
| S No. | Study | Year of study | No. of cases | Gender | Age (years) | Site (In Thyroid) |
|---|
| 1. | Lewis JE et al., [7] | 1987 | 1 | F | 40 | Right lobe Isthmus |
| 2. | Chan JK et al., [6] | 1991 | 1 | F | 71 | Left lobe |
| Chan JK et al., [6] | 1991 | 1 | F | 38 | Isthmus |
| 3. | Asa SL et al., [8] | 1988 | 1 | F | 35 | Right lobe |
| 4. | Cohen JB et al., [1] | 2003 | 1 | F | 39 | Left lobe |
| 5. | Weissferdt A and Moran CA [5] | 2015 | 1 | M | 48 | Left lobe |
| Weissferdt A and Moran CA [5] | 2015 | 1 | F | 53 | Left lobe |
| Weissferdt A and Moran CA [5] | 2015 | 1 | F | 43 | Right lobe |
| 6. | Current case | 2018 | 1 | F | 43 | Right and left lobes |
The present case being discussed was noted in a 43-year-old lady with a diffuse swelling in front of the neck. Histologically and immunophenotypically intrathyroidal thymomas are similar to those of mediastinal thymomas. They are composed of epithelial cells admixed with lymphocytes in varying proportions and stain positively for Pancytokeratin (AE1/AE3). However compared to mediastinal thymomas, primary ectopic intrathyroidal thymomas appear more commonly in females and are not associated with any autoimmune disorders [5].
When ectopic intrathyroidal thymoma is suspected, differential diagnosis including Hashimoto’s thyroiditis, lymphoma, insular carcinoma of thyroid and CASTLE should be ruled out. Histologically, when ectopic intrathyroidal thymomas contain large proportion of lymphocytes, Hashimoto’s thyroiditis and lymphomas can be ruled out by immunohistochemical markers like cytokeratins and lymphoid markers like TdT and CD1a which help identify the epithelial component and the immature lymphocytic component in ectopic thymomas. Insular carcinoma of thyroid can be differentiated from PIT due to absence of lymphocytic infiltrate and diffuse reactivity with thyroglobulin immunostain. CASTLE has high grade cytological features, squamoid differentiation and mature lymphocytic elements lacking expression of TdT and CD1a seen in thymocytes [5].
The prognosis seems to depend on the status of invasion at the time of diagnosis [5]. In the present case the tumour was limited to the capsule.
Conclusion
Ectopic thymoma is a very rare entity and can occur in neck, anterior and posterior mediastinum, lung, pleura and heart. Ectopic intrathyroidal thymoma is even rarer and the differential diagnosis of CASTLE, insular carcinoma of thyroid, lymphoma and Hashimoto’s thyroiditis should be considered before a final diagnosis is made. Complete surgical resection is the treatment of choice if the tumour is only confined to the thyroid. However if the tumour is invasive, additional treatment like radiotherapy may be required to prevent recurrence or metastasis.
[1]. Cohen JB, Troxell M, Kong CS, McDougall IR, Ectopic intrathyroidal thymoma: a case report and reviewThyroid 2003 13(3):305-08.10.1089/10507250332158213212729482 [Google Scholar] [CrossRef] [PubMed]
[2]. Rosai J, Levine GD, Tumors of the ThymusAFIP Atlas of Tumor Pathology, Second Series 1987 13:01-19. [Google Scholar]
[3]. Farley AM, Morris LX, Vroegindeweij E, Depreter MLG, Vaidya H, Stenhouse FH, Dynamics of thymus organogenesis and colonization in early human developmentDevelopment 2013 140(9):2015-26.10.1242/dev.08732023571219 [Google Scholar] [CrossRef] [PubMed]
[4]. Filosso PL, Delsedime L, Cristofori RC, Sandri A, Ectopic pleural thymoma mimicking a giant solitary fibrous tumour of the pleuraInteract Cardiovasc Thorac Surg 2012 15(5):930-32.10.1093/icvts/ivs36022922387 [Google Scholar] [CrossRef] [PubMed]
[5]. Weissferdt A, Moran CA, Ectopic primary intrathyroidalthymoma: a clinicopathological and immunohistochemical analysis of 3 casesHum Pathol 2016 49:71-76.10.1016/j.humpath.2015.10.01126826412 [Google Scholar] [CrossRef] [PubMed]
[6]. Chan JK, Rosai J, Tumors of the neck showing thymic or related branchial pouch differentiation: a unifying conceptHum Pathol 1991 22(4):349-67.10.1016/0046-8177(91)90083-2 [Google Scholar] [CrossRef]
[7]. Lewis JE, Wick MR, Scheithauer BW, Bernatz PE, Taylor WF, Thymoma. A clinicopathologic reviewCancer 1987 60(11):2727-43.10.1002/1097-0142(19871201)60:11<2727::AID-CNCR2820601125>3.0.CO;2-D [Google Scholar] [CrossRef]
[8]. Asa SL, Dardick I, Van Nostrand AW, Bailey DJ, Gullane PJ, Primary thyroid thymoma: a distinct clinicopathologic entityHum Pathol 1988 19(12):1463-67.10.1016/S0046-8177(88)80242-9 [Google Scholar] [CrossRef]