Cryptococcal meningitis is a fatal central nervous system disease commonly affecting immunocompromised patients, and rarely affects immunocompetent patients. We report a 51-year-old previously well male who presented with giddiness, altered sensorium and intermittent fever. India Ink stain and cryptococcal antigen test of cerebral spinal fluid were both positive. Immunodeficiency screening was negative. Although MRI brain demonstrated several features that are characteristic, they are unfortunately non-specific. It is important to realise immunocompetence does not exclude one from contracting cryptococcal meningitis, and a high index of suspicion with consideration of various imaging differentials and biochemical markers is helpful in narrowing down the diagnosis.
Basal leptomeningeal enhancement, Choroid plexus enlargement, Hydrocephalus, Periventricular cysts
Case Report
A 51-year-old male with no previous medical illness presented with intermittent headache, lethargy, giddiness and fever for three weeks. His symptoms progressively worsened and he developed vomiting, altered sensorium and facial asymmetry two days prior to admission. He had an episode of seizure a month ago while riding motorbike, and was admitted to another hospital where he was treated conservatively for the injuries. There was no history of Pulmonary Tuberculosis (PTB) or contact with PTB patients. No history of recent travel or malignancy. He was married and worked as a carpenter. He neither smoked nor drank. Family members denied any history of high-risk behaviour.
On examination, patient was confused but was able to answer simple questions. Glasgow Coma Scale (GCS) was E4V3M6. He was haemodynamically stable and afebrile. Pupils were equal and reactive bilaterally. Neck stiffness was present. Neurological examination showed presence of right 7th cranial nerve palsy. Babinski sign was negative. The rest of neurological examinations were unremarkable.
Computerised Tomography (CT) brain was performed and showed acute hydrocephalus and cerebral oedema. Initial diagnosis of TB meningitis was made based on clinical and radiological findings and empirical treatment was started, together with antibiotics. He underwent extraventricular drainage. Mycobacterium culture and sensitivity and tuberculosis Polymerase Chain Reaction (PCR) of Cerebrospinal Fluid (CSF) were both negative. Serology for HIV, Hepatitis B and C, repeated twice, were all non-reactive. Fasting blood sugar was normal.
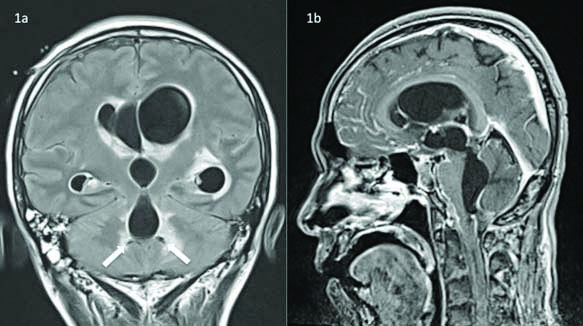
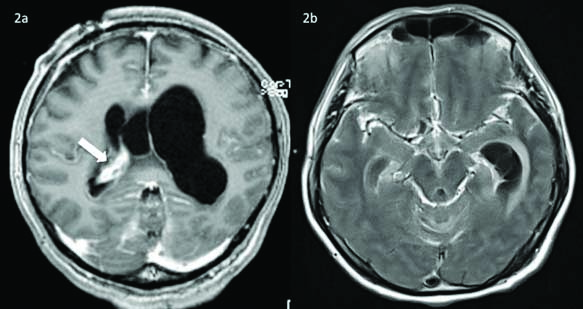
MRI Brain was subsequently done and showed basal and bifrontal leptomeningeal and pachymeningeal enhancement with non-communicating hydrocephalus, upper cervical hydromyelia and tonsillar herniation [Table/Fig-1,2(a,b)]. Multiple septations were present within both lateral ventricles suggestive of ventriculitis. There were also several small lesions of CSF intensity on all sequences at posterior left periventricular area around the dilated fourth ventricle [Table/Fig-2a]. The choroid plexus in right lateral ventricle was enlarged and enhancing compared to the left [Table/Fig-2a].
MRI brain: (a) T2 FLAIR coronal image showing two small cystic lesions (arrows) at posterior periventricular area around the dilated fourth ventricle, likely representing dilated VR spaces. These are of CSF intensity on all sequences, including DWI/ADC. Hydrocephalus is present; (b) T1 post-contrast sagittal image showing tonsillar herniation and cervical hydromyelia. Note the basal cistern leptomeningeal enhancement and non-communicating hydrocepahlus.
MRI brain: (a) T1 post-contrast axial image showing hydrocephalus and enlarged enhancing choroid plexus (arrow) in right lateral ventricle; (b) T2 FLAIR post-contrast axial image shows basal cistern leptomeningeal enhancement and effacement.
Lumbar puncture was performed. CSF protein was raised, 5652 mg/L, and glucose was low, <0.28 mmol/L. India Ink stain and Cryptococcus Antigen test were both positive. A diagnosis of cryptococcal meningitis was made and he was started on intravenous amphotericin B 35 mg three times daily and intravenous flucytosine1.25 gm four times daily.
In the ward, his condition was complicated by acinetobacter bacteraemia and he was treated with concurrent antibiotics. He completed six weeks of amphotericin B and flucytosine, and continued with oral fluconazole 400 mg daily. He was discharged three months later on tracheostomy. GCS upon discharge was E4VTM2. The plan was to complete six months of oral fluconazole.
Discussion
Cryptococcal meningitis is the most common fungal infection affecting the central nervous system. It is caused by Cryptococcus neoformans, an encapsulated yeast found in soil contaminated by animal and bird droppings [1]. It occurs commonly as an opportunistic infection in immunocompromised, cancer, diabetic and organ transplant patients, and most commonly AIDS patients [2]. As it is rarely seen in otherwise healthy individuals, the diagnosis is often delayed in this group of patients, not to mention the commonly non-specific presenting symptoms.
Cryptococcal meningitis is typically acquired via inhalation with further haematogeneous dissemination crossing the blood brain barrier into the brain and meninges [3]. Although it is relatively uncommon in immunocompetent individuals, cases have been reported [4,5]. In a study done by Mahale K et al., 20 out of 242 patients with meningitis were found to have cryptococcal meningitis, and all of them were immunocompromised [2]. Our patient is immunocompetent with no known risk factor.
Radiological findings of cryptococcal meningitis are generally non-specific. Normal imaging finding does not exclude the diagnosis [6]. The variability of the imaging findings makes the radiological diagnosis difficult [3].
The most common imaging findings in cryptococcal meningitis are hydrocephalus, meningeal enhancement, infarcts, dilated Virchow-Robin (VR) spaces, and normal findings. Less common findings include intraparenchymal cryptococcomas, abscesses, ventriculitis, and choroid plexus enlargement [7,8]. Enhancement of leptomeninges is a common MRI feature of cryptococcal meningitis, and is most obvious in the basal cisterns [9]. A study done by Chen S et al., showed that meningeal enhancement is more common in immunocompetent patients, as in our patient. Hydrocephalus is a common complication of cryptococcal meningitis [9], was present in our patient too. Dilated VR spaces are seen as multiple, small, round or oval cysts filled with mucoid gelatinous material giving rise to “soap bubble” appearance on imaging, most commonly reported at the basal ganglia, thalami, midbrain, cerebellum and at the periventricular regions [3,7]. Although scattered VR space dilatation can be found in normal persons especially in the elderly, cluster of these in typical locations and in the correct clinical setting are highly suggestive of cryptococcal infection [4,8]. In this patient, there were two small cysts seen at the left posterior periventricular area adjacent to the fourth ventricle on T2 FLAIR sequence. The scattered instead of clustered distribution is rather non-specific in this case, but given the location in perventricular region and clinical presentation of meningitis, cryptococcosis should be considered. Parenchymal involvement may occur in two forms; cryptococcoma and miliary pattern [3]. Cryptococcoma demonstrates intermediate to low signal intensity on T1 Weighted Imaging (T1WI), high signal nodular lesions on T2 weighted and FLAIR sequences with surrounding oedema. Most common sites of involvement are adjacent to the perivascular spaces, basal ganglia and midbrain [3]. Both forms of parenchymal involvement were not demonstrated in this patient.
Another imaging manifestation of cryptococcal meningitis is choroid plexus involvement. Cryptococcal lesions in choroid plexus are typically mixed solid cystic on CT and MRI. Choroid plexus may be enlarged and enhancing and can appear striking to the extent that it could be mistaken for a mass. Although choroid plexus involvement is not pathognomonic of cryptococcal infection, it should be considered when present in HIV patients [3]. In our patient, on T1WI, the choroid plexus at right lateral ventricular trigone appears enlarged. No definite cystic lesion was seen within.
The imaging manifestation of cryptococcal meningitis in immunocompetent and immunocompromised patients may differ depending on host immune response. Meningeal enhancement is commonly absent or minimal in AIDS patients who have cryptococcal meningitis, possibly related to impaired cell-mediated immunity [6,9]. Cryptococcoma is more likely to be seen in immunocompetent patients while normal or mildly dilated VR spaces and cortical atrophy are seen in immunocompromised patients [6,7]. The imaging findings are however not mutually exclusive [8]. Our immunocompetent patient had prominent meningeal enhancement, but at the same time also had dilated VR spaces that were supposedly more common in the immunocompromised.
Differential diagnoses based on imaging findings include TB meningitis and bacterial meningitis. TB meningitis typically presents with hydrocephalus, meningeal enhancement, vasculitic infarcts and tuberculomas. Dilated VR spaces and choroid plexus enlargement however are not its features. Bacterial meningitis may present with similar radiological features as those of TB meningitis, but clinical presentation is usually more acute, unlike this patient.
Conclusion
Cryptococcal meningitis can present with a wide spectrum of imaging findings depending on host immune response. Although the disease is generally uncommon in immunocompetent patients, the diagnosis should be considered when a constellation of suggestive imaging findings, in particular VR space dilatation and choroid plexus enlargement, are present.
[1]. Pappas PG, Cryptococcal infections in non-HIV-infected patientsTransactions of the American Clinical and Climatological Association 2013 124:61-79. [Google Scholar]
[2]. Mahale K, Patil S, Ravikumar Nagabhushan Mahale R, Prevalence of Cryptococcal Meningitis Among Immuno-competent and Immuno-compromised Individuals in Bellary, South IndiaA Prospective Study Journal of Clinical and Diagnostic Research 2012 6(3):388-92. [Google Scholar]
[3]. Offiah CE, Naseer A, Spectrum of imaging appearances of intracranial cryptococcal infection in HIV/AIDS patients in the anti-retroviral therapy eraClinical Radiology 2016 71(1):09-17.10.1016/j.crad.2015.10.00526564776 [Google Scholar] [CrossRef] [PubMed]
[4]. Bello YB, Machado HG, Silveira JF, Schettini F, Junior GM, Junior SD, Cryptococcal Meningitis in Immunocompetent Patient-Case ReportAmerican Medical Journal 2013 4(1):100-04.10.3844/amjsp.2013.100.104 [Google Scholar] [CrossRef]
[5]. Arif S, Ghazanfar K, Muhammad WW, Malik H, Cryptococcal meningitis in immunocompetent patientJ Ayub Med Coll Abbottabad 2015 27(4):942-44. [Google Scholar]
[6]. Xia S, Li X, Li H, Imaging characterization of cryptococcal meningoencephalitisRadiology of Infectious Diseases 2016 3(4):187-91.10.1016/j.jrid.2016.05.003 [Google Scholar] [CrossRef]
[7]. Kumari R, Raval M, Dhun A, Cryptococcal choroid plexitis: rare imaging findings of central nervous system cryptococcal infection in an immunocompetent individualThe British Journal of Radiology 2010 83(985):e014-e7.10.1259/bjr/5094521620139243 [Google Scholar] [CrossRef] [PubMed]
[8]. Cheng Y-C, Lirng J-F, Chang F-C, Wang S-J, Fuh J-L, Chen S-S, Radiological Manifestations of cryptococcal in fection in central nervous systemJ Chin Med Assoc 2003 66:19-26. [Google Scholar]
[9]. Chen S, Chen X, Zhang Z, Quan L, Kuang S, Luo X, MRI findings of cerebral cryptococcosis in immunocompetent patientsJournal of Medical Imaging and Radiation Oncology 2011 55(1):52-57.10.1111/j.1754-9485.2010.02229.x21382189 [Google Scholar] [CrossRef] [PubMed]