SCD is an autosomal recessive disorder of the ß globin gene in which haemoglobin S polymerizes in erythrocytes in deoxygenated conditions causing occlusion of small blood vessels. SCD is highly prevalent in African countries (5-40%) followed by Asian Arabian and Asian countries [1,2]. It is found in many areas of India and in tribal community too, also is prevalent in different parts of Odisha [3-6].
Pain is the hallmark of presentation, patients presenting as painful vaso-oclusive crisis due to occlusion of blood vessel [7]. In the presence of cellular dehydration or oxidative stress, the red blood cells of sickle cell patients is transformed to a sickled shape instead of the normal bi-concave disc. They get stucked in the small vessels leading to ischemia, hypoxia, and subsequent tissue necrosis. The hypoxia leads to more sickling and a cycle becomes vicious [8]. Ophthalmic manifestations are also due to vaso-occlusion. Homozygous Sickle Cell Disease (HbSS) patients have the worst systemic complications while sickle cell C disease (HbSC) and Sickle thal (S-thal) patients have the most severe ocular problems like proliferative retinopathy and resultant vision loss. This is because the blood is more viscous in sickle cell trait and Sickle-thal group as small retinal arterioles occlude more easily [9]. Salmon-patch haemorrhages and black sunburst pigments are observed in pre-proliferative retinal changes. These are due to retinal pigment epithelial layer reaction to choroidal infarction and retinal haemorrhage [10]. Retinal examination may include silvering of peripheral arterioles and intra retinal refractile bodies, and proliferative retinal changes include sea fan like neovascularization, vitreous haemorrhages, and retinal detachments. Other associated manifestations include venous tortuosity, retinal holes, Central retinal artery occlusion, and angioid streaks. Treatment consists of Pan Retina laser Photocoagulation (PRP) or cryotherapy applied to the peripheral areas of retinal ischemia, usually anterior to the sea fans. New vessels formation occurs due to blockage of their feeder vessels. AntiVEGF agents have found to have good response in the treatment of sickle retinopathy. The present study evaluated the pattern of ophthalmic presentation of sickle cell disease (HbSS) patients in a tertiary care medical college in eastern India.
Materials and Methods
This prospective study was done in Institute of Medical Science (IMS) & SUM hospital a 700 bedded tertiary care and a medical college catering patients from most districts of Odissa and nearby states too, situated in Bhubaneswar, Odissa, India. This study was done over a period from April 2015 to May 2016. Patients coming to Department of Medicine for evaluation of anemia who were detected or suspected for haemoglobinopathy were advised for Haemoglobin electrophoresis. In this study, 49 patients including 31 males (63%) and 18 females (37%) having HbS window more than 40% (SCD) were considered randomly for inclusion in study group. Patients suffering from diabetes, hypertension, other metabolic diseases were excluded from study and patients with haemoglobin less than 8 mg% were also excluded from the study. All the 49 patients were sent to Department of Ophthalmology, IMS & SUM Hospital for examination and findings were analysed. External eye examination like lid, periorbital area, conjunctiva and sclera, slit lamp examination, Fundoscopy (Direct and if required Indirect Ophthalmoscopy), OCT (Optical Coherence Tomography) (If required) were done in all cases. Ethical committee clearance was taken from Institutional Ethical Committee (Ethical approval No EC/IMS/SOA/123/2014). Written consent was also taken from all patients according to protocol. Findings were tabulated and analysed.
Statistical Analysis
For statistical analysis, the software used was SPSS 20 version software. All the documented parameters compared using ANOVA test and p-value <0.05 was considered as statistical significant.
Results
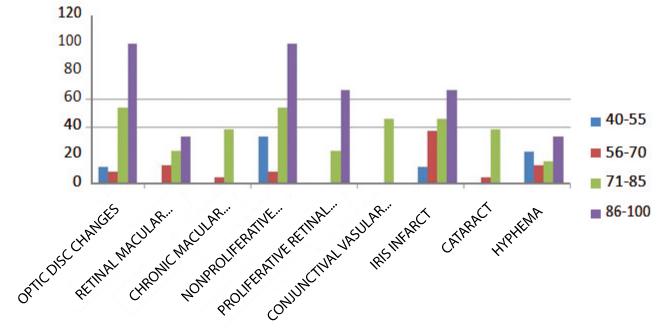
In this prospective study, 49 SCD were screened for different ophthalmic manifestations. Among the 49 sickle cell patients, 13 patients (26%) (includes both male and female) were observed with optic disc changes like dark red intravascular spots [Table/Fig-1] and from them 21-25 age group revealed maximum number of patients (5). Similarly, from investigation like Slit lamp examination, Fundoscopy, 7(14%) patients were found with retinal macular vascular change like dark, small and red dilated capillaries [Table/Fig-1]. Fifteen (30%) presented with Non-proliferative retinal changes like salmon patches, and Angioid streak affecting all age group except the group 51-56 year [Table/Fig-1]. Proliferative retinal changes like Hair pin loop capillaries, Sea fan retinopathy in sickle cell patients were found in total of 5 patients [Table/Fig-1]. Retinal detachment was detected in 2(4%) patients. Eighteen (36%) patients involving all the age group suffered conjunctival vascular changes like comma shaped vascular segments, cork screw shaped or abnormally long, linear dilatations of vessels. Posterior Segment Manifestations findings are significantly different at p=0.001 in ANOVA Test [Table/Fig-1]. With Cataract (opacity in lens) screening, it was revealed that younger age groups were not suffered where as all the older age grouped patients suffered. Total 8 cases (16%) with age between 38 to 56 suffered with cataract, most of cases above 45 years [Table/Fig-2]. Hyphema (blood in anterior segment) an uncommon finding was found in two cases only (4%) affecting the 15-20 age and 31-35 age group only [Table/Fig-2]. Anterior Segment Manifestations findings are significantly different at p=0.0001 in ANOVA test. Patients with optic disc changes were found 11.1% in patients with S-window in range of 40 to 55, 8.33% in 56-70 S-window, 53.8% in 71-85 S-window, 100% in 86-100 S-window. Retinal macular vascular changes were found 0% in patients with HbS window 40-55, 12. 5% in HbS window of 56-70, 23.08% in HbS Window 71-85, 33.33% in HbS Window of 86-100 [Table/Fig-3]. Similarly chronic macular vascular changes was found to be with 0%, 4.17%, 38.46%, 0%, non proliferative retinopathy was found to be 33%, 8.33%, and 53.85%, 100%, conjunctival vascular changes 0%, 0%, 46%, 0%, iris infarct in 11.1%, 37.5%, 46.15%, 66.6%, cataract in 0%, 4.1%, 38.4%, 0% and hyphema in 22.2%, 12.5%, 15.3%, and 33.3% correspondingly in the HbS Window range of 40-55, 56-70, 71-85, 86-100 respectively [Table/Fig-3]. Ophthalmic manifestation in different HbS window are shown in [Table/Fig-4] which significantly increases at p=0.0027 in ANOVA test.
Posterior segment manifestations (According to no. of patients).
| Age (years) | No of patients | Optic disc change | Retinal macular vascular changes | Retinal detachment | Non-proliferative retinal change | Proliferative retinal change |
|---|
| 15-20 | 7 | 1 | 1 | 0 | 0 | 0 |
| 21-25 | 10 | 5 | 2 | 0 | 5 | 0 |
| 26-30 | 8 | 4 | 1 | 0 | 3 | 2 |
| 31-35 | 5 | 0 | 0 | 0 | 1 | 0 |
| 36-40 | 9 | 2 | 2 | 1 | 3 | 2 |
| 41-45 | 4 | 1 | 1 | 0 | 1 | 0 |
| 46-50 | 3 | 0 | 0 | 1 | 2 | 0 |
| 51-56 | 3 | 0 | 0 | 0 | 0 | 1 |
| Total | 49 | 13 | 7 | 2 | 15 | 5 |
Anterior segment manifestations (According to no. of patients).
| Age (years) | No of patients | Conjunctival vascular changes | Cataract | Hyphema |
|---|
| 15-20 | 7 | 3 | 0 | 1 |
| 21-25 | 10 | 2 | 0 | 0 |
| 26-30 | 8 | 3 | 0 | 0 |
| 31-35 | 5 | 1 | 0 | 1 |
| 36-40 | 9 | 3 | 1 | 0 |
| 41-45 | 4 | 1 | 1 | 0 |
| 46-50 | 3 | 2 | 3 | 0 |
| 51-56 | 3 | 3 | 3 | 0 |
| Total | 49 | 18 | 8 | 2 |
HbS window & Ophthalmic manifestation (according to % age of patients).
| S-window | Optic disc changes | Retinal macular vascular changes | Chronic macular vascular changes | Non-proliferative retinal changes | Proliferative retinal changes | Conjunctival vascular changes | Irisinfarct | Cataract | Hyphema |
|---|
| 40-55 | 11.11 | 0 | 0 | 33.33 | 0 | 0 | 11.11 | 0 | 22.22 |
| 56-70 | 8.33 | 12.5 | 4.17 | 8.33 | 0 | 0 | 37.5 | 4.17 | 12.5 |
| 71-85 | 53.85 | 23.08 | 38.46 | 53.85 | 23.08 | 46.15 | 46.15 | 38.46 | 15.38 |
| 86-100 | 100 | 33.33 | 0 | 100 | 66.67 | 0 | 66.67 | 0 | 33.33 |
Ophthalmic manifestation in different HbS window are significantly increases at p=0.0027 in Anova test
HbS window & ophthalmic manifestation.
Y axis denotes Hb S Window (level of Hb S in patient)
X axis denotes Ophthalmic manifestations
Discussion
Sickle cell ophthalmic involvement is not uncommon in India. Features of mild conjunctival involvement to retinal changes of non proliferative and proliferative retinopathy are found in sickle cell anemia which may lead to visual impairment to vision loss too. More number of males presented with ophthalmic involvement in the present study. Age of presentation is middle age, but the trend is now lower, about 60% of cases seen are below 35 years of age. Goldberg MF et al., had observed the mean age for the ocular changes as 28 years [11], while Condon PI et al., had seen maximum changes in 10-20 years [12].
Our study determines non-proliferative retinopathy (NPSCR) (30%) followed by optic disc changes (26%) in posterior segment abnormalities of eye. Condon PI et al., (97.4% in HbSS cases) have observed such changes in various degree in sickle cell anemia and sickle cell HbC disease other than sickle cell trait. Significant changes were observed in major retinal vessels (28.57%). They had noted retinal haemorrhage (2.6%) and tortuosity and dilatations of capillary network with micro-aneurysmal formation and neovascularisation (39.5%) in the Hb-SS cases of his study which was uncommon in our observation [12]. Menaa F et al., describes NPSCR, more commonly observed in SS patients, is manifested by typical alterations depending on the retinal location also the retinal periphery of patients with NPSCR is frequently characterized as bilateral changes [13]. Retinal macular vascular changes seen in 14% cases which was also noted by other studies like Condon PI et al., Weich RB et al., and Asdourian G et al., [12,14,15].
Vision loss is uncommon in patients with HbSS [16]. A study from Ghana showed that vision loss is confined to HbSC patients [17]. Study in children with HbSS showed increased vascular tortuosity. HbSS patients have relatively less vaso-occlusion in the small-caliber vessels of the retina because of their overall lower haematocrit although they have more number of circulating sickled red cells [11]. The occlusions in HbSC disease may be less severe, but with continuous secretion of angiogenic substances by the damaged tissues may lead to chronic ischemia without complete infarction [18]. Most patients require laser photocoagulation to the peripheral ischemic retina to destroy VEGF producing cells and improve retinal oxygenation. Bevacizumab may be used similarly in proliferative diabetic vision loss [19]. In our study, conjunctival vascular changes found maximum 18(36%) in anterior segment abnormalities and less commonly cataract 8(16%) and hyphema 2(4%) cases. Nagpal KC et al., observed conjunctival vascular changes like comma shaped vascular segments, cork screw shaped or abnormally long, linear dilatations of vessels in their study [20]. Al-salem M et al., found comma conjunctival sign was found in 8 out of 54 patients (14. 8%) and tortuous vessels in the anterior segment (conjunctival and episcleral) were found in 1% of cases [16]. Routray K et al., found 90.4% conjunctival vascular changes in an Indian study [21]. Osaffo-Kwaako A et al., observed 46% of conjunctival vascular changes and 2.6% of cataract in their HbSS patient group [17]. Both anterior and posterior segment manifestations significantly (p=0.0027) increased with progressive increase in HbS window. No definite comparative study was found in this context, however in contrary, most of African studies demonstrate ophthalmic manifestation and morbidity are more in HbSC than in HbSS [11,17,22]. This may be explained by the fact that patients of studied geographical area are more with HbF level possibly providing protection for late presentation and also there is no HbSC in this study group [5,6,22].
Limitation
This study has limitations of not including Sickle cell trait and HbSC cases for comparison and also having less number of study population, however larger study-group with comparative analysis is required for better results.
Conclusion
SCD is a disease of increased concern due to repeated vaso-occlusion leading to crisis, hospitalization and no definite cure. Ophthalmic manifestations although not a common presentation is a matter of concern as early diagnosis and appropriate management may prevent visual loss especially in Sickle cell retinopathy. Both anterior and posterior segment manifestations increase with progressive increase in HbS window in HbSS patient’s. Hence Sickle cell haemoglobinopathy patients routinely should be screened for ophthalmic manifestations.
Ophthalmic manifestation in different HbS window are significantly increases at p=0.0027 in Anova test